CHAPTER 85 THE DIAGNOSIS AND MANAGEMENT OF CARDIAC DYSRHYTHMIAS
With increasing frequency, patients undergoing surgery have multiple medical comorbidities, not necessarily associated with their surgical disease. Cardiac dysrhythmia in this setting can be a primary event, a secondary event related to ischemia or myocardial infarction, or may be due to toxic or metabolic abnormalities associated with perioperative care. The type of dysrhythmia can usually be diagnosed with a focused physical exam, a standard 12-lead electrocardiogram (ECG), and from the response to specific maneuvers or drug therapy. The acute management depends on the hemodynamic stability of the patient, the accurate classification of dysrhythmia, and an understanding of the underlying mechanism so that appropriate treatment can be given in an expeditious fashion. Management may include a combination of cardioversion for the acutely unstable, pharmacological intervention, percutaneous or transvenous pacing, or modalities such as aberrant pathway ablation and implantation of pacemakers or defibrillators.
INCIDENCE
The incidence of dysrhythmia following cardiac surgery can be high as 40% in some studies, with a large proportion caused by atrial fibrillation. It is well known that up to 15% of patients with inferior wall myocardial infarction present with atrioventricular (AV) nodal conduction disturbances or complete heart block. Patients with pre-existing cardiac or pulmonary disease have an increased risk of dysrhythmia, which is compounded in the face of noncardiac surgery, trauma, or other critical illness. Vasopressor requirement is associated with an increased risk of dysrhythmia due to the proarrhythmic effect of catecholamines on the heart. It has been shown that dysrhythmias, in a standard intensive care unit (ICU) that admits cardiac, noncardiac, and medical critical care patients, occur in up to 20% of patients. The vast majority are tachyarrhythmias, while 10% are bradyarrhythmias. Dysrhythmias are distributed equally between atrial and ventricular origin. Atrial fibrillation and ventricular tachycardia are by far the most common. Patients that have dysrhythmias have longer ICU stays and had worse survival overall, likely signifying that dysrhythmias in patients are an indicator of more severe critical illness.
BRADYARRYTHMIAS
Atrioventricular Node
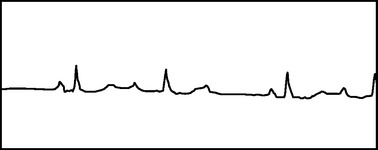
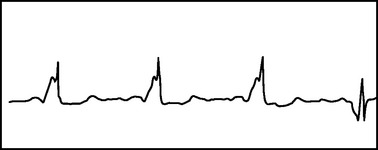
Disturbances in conduction through the AV node or His-Purkinje system are classified as atrioventricular blocks. These may be temporary or permanent, depending on the etiology of the delayed conduction. In adults, the most common causes are drug toxicity, coronary artery disease, and degenerative disease of the conduction system. Many other conditions, such as electrolyte disturbances, myocarditis, sarcoidosis, scleroderma, and hypervagal responses, can cause AV block. The P-R interval is a measure of the conduction time through the AV node and bundle of His. When the P-R interval is prolonged (>210 milliseconds), a patient has first-degree AV block. Second-degree AV block is when intermittent failure of the conduction of the impulse to the ventricles occurs. In Mobitz type I, second-degree AV block (Wenckebach block), there is progressive prolongation of the P-R interval until failure of conduction to the ventricle occurs (Figure 1). The P-R interval then shortens following the dropped beat. This failure in conduction originates from the AV node itself and the QRS complex remains narrow. In Mobitz type II, second-degree AV block, there is intermittent failure of conduction reaching the ventricles that is not associated with progressive prolongation of the P-R interval. There is not a shortened P-R interval following the dropped beat. This failure in conduction is considered “infranodal” and originates from the His-Purkinje system. The QRS complex may be prolonged, and this type of AV block is more concerning. There is a significant likelihood of progression to complete heart block associated with inadequate ventricular response with this rhythm. Third-degree or complete heart block results from failure of all impulses through the AV node and His-Purkinje system, resulting in atrioventricular disassociation. The ventricles rely on their innate automaticity which produces a typical wide QRS escape rhythm between 40 and 50 beats per minute. The atrial rate is commonly faster, producing multiple P waves with no relationship to the ventricular QRS complexes (Figure 2).
Management of AV block depends on the hemodynamic stability of the patient, the transient nature of the dysrhythmia, and where the focus originates from within the conduction system. Acute pharmacotherapy relies upon atropine and isoproterenol. Isoproterenol use should be avoided in patients with ischemia heart disease because of the associated increase in myocardial oxygen demand. There is no long-term pharmacotherapy for AV block, and removal of any of the common offending agents, such as digitalis or beta-blockers, should first be attempted. Temporary pacing is used for those with ongoing instability, and permanent pacing is typically required for Mobitz type II second-degree AV block and third-degree AV block.
TACHYARRHYTHMIAS
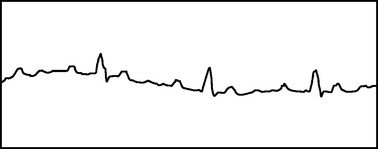
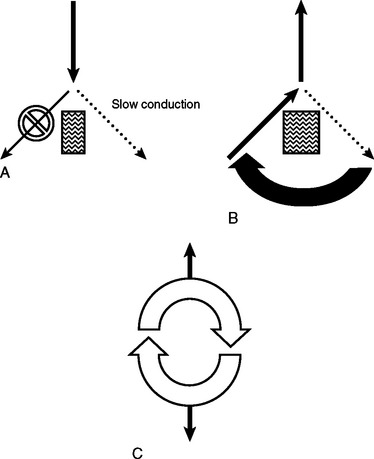
Tachyarrhythmias are classified according to their anatomical origin in relation to the AV node. Those that originate at or above the AV node are considered supraventricular tachyarrhythmias; the most relevant include sinus tachycardia, paroxysmal supraventricular tachycardia, multifocal atrial tachycardia, atrial flutter, and atrial fibrillation. Ventricular tachyarrhythmias originate from below the AV node and include ventricular tachycardia and ventricular fibrillation. Important determinants of the malignant potential of these tachyarrhythmias are the duration, the hemodynamic consequences, and the presence of significant structural heart disease. The acute management depends on a basic understanding of the mechanism, the choices for pharmacological intervention (Table 1), and the indications for urgent cardioversion for each situation. Interventional techniques, such as aberrant pathway ablation and implantation of pacemakers and defibrillators, have drastically improved long-term outcome once patients have left the ICU setting, and have added significantly to our armamentarium in treating these dysrhythmias.
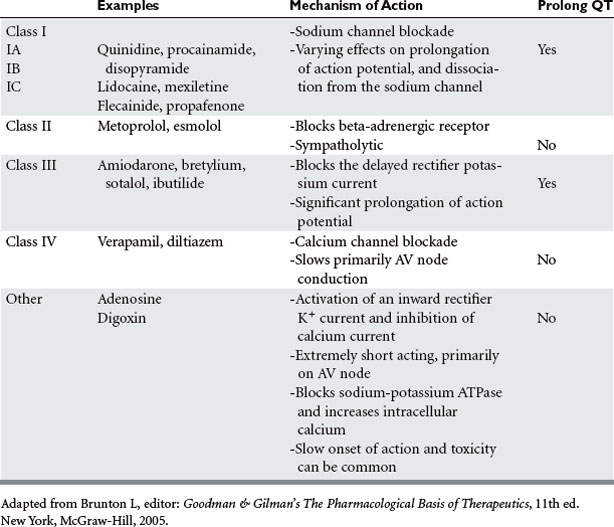
The mechanism by which tachyarrhythmias arise are categorized into (1) abnormal automaticity, (2) triggered activity, or (3) re-entry. Abnormal automaticity occurs when cells outside the normal conduction system generate spontaneous impulse formation. Triggered activity occurs during “after depolarizations,” which cause the membrane potential to reach threshold early and generate abnormal impulse formation. Re-entry, the most common mechanism, occurs when an impulse can travel down two pathways separated by an area of unexcitable tissue. One of the pathways contains a unidirectional block, with slowed conduction, so that recovery and further excitation can subsequently occur. This defines an area of cardiac tissue that can self-propagate and thus becomes the focus for the generation of the tachyarrhythmia (Figure 3).
Sinus Tachycardia
Sinus tachycardia should be considered a physiological reflex rather than a true dysrhythmia, but it is an important sign for which the etiology must be sought. Fever, hypovolemia, and anemia all appropriately increase heart rate to at least maintain or increase cardiac output. Blunting this reflex with pharmacotherapy without knowledge of the etiology can be dangerous. Thyrotoxicosis, pheochromocytomas, or side effects of sympathomimetic drugs also cause sinus tachycardia without regard for reflex mechanisms. The primary goal for management of sinus tachycardia is to find and appropriately treat the confounding condition. Sinus tachycardia will resolve with resolution of this inciting process.
Paroxysmal Supraventricular Tachycardia
When the accessory pathway has the potential for antegrade conduction, the QRS complex will be wide, since conduction occurs between the ventricular myocytes themselves rather than the His-Purkinje system. Wolfe-Parkinson-White syndrome occurs when the accessory pathway allows both antegrade and retrograde conduction, and commonly a delta wave or pre-excitation can be seen in the early QRS complex (Figure 4). This syndrome can present in early adulthood, and the initial presentation can be ventricular fibrillation. Management in these patients where conduction occurs antegrade through the accessory pathway varies from narrow complex AVRT as described previously. Adenosine will only be effective if the antegrade conduction occurs through the AV node. Otherwise it can precipitate atrial fibrillation, which can result in degeneration to ventricular fibrillation when an antegrade accessory pathway exists in these patients. Calcium channel blockers and digoxin are contraindicated, because they will slow conduction in the AV node and enhance conduction through the accessory pathway. Class I and class III antiarrhythmics, which include flecainide, procainamide, and ibutilide, are able to depress the conduction across the accessory pathway, decrease the ventricular rate, and likely terminate the wide QRS tachyarrythmia. Direct-current cardioversion is used with hemodynamic instability or if failure of antiarrhythmic therapy occurs.
Multifocal Atrial Tachycardia
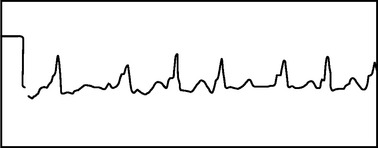
Multifocal atrial tachycardia is thought to be due to abnormal automaticity and is commonly associated with chronic respiratory disease, congestive heart failure, and pulmonary embolus. It has an irregular rate and rhythm that is characterized by the presence of three or more morphological different P waves on ECG, and rates of 110–140 beat/min (Figure 5). It can easily be confused with atrial fibrillation if P waves are not prominent on a rhythm strip. First-line therapy consists of treating the underlying condition, correction of hypercarbia or hypoxia, and electrolyte repletion. Calcium channel blockers typically can provide rate control but beta-blockers should be used with caution in those with obstructive pulmonary disease. Amiodarone can be helpful in patients refractory to first-line therapies.
Atrial Flutter
Atrial flutter is due to a re-entrant circuit from within atrial tissue and is associated with atrial enlargement. It is commonly grouped with atrial fibrillation due to similar associated causes and similar treatment regimens. Atrial rates of 250–350 beats/min are typical. The AV node refractory period allows only a proportion of these atrial beats to pass to the ventricle, typically in a 2:1 ratio. When a ventricular pulse rate is measured to be 150 beats per minute, atrial flutter should be considered. By increasing AV nodal delay with adenosine or beta-blockade, the atrial “flutter waves,” characterized by a saw-tooth appearance, can usually be seen on a rhythm strip (Figure 6). Adenosine may be useful for diagnosis, but as with atrial fibrillation, it rarely converts the rhythm back to sinus. Beta-blockers and calcium channel blockers allow ventricular rate control, but more commonly the use of antiarrythmic drug therapy and or electrical cardioversion is required if the rhythm remains persistent.
Atrial Fibrillation
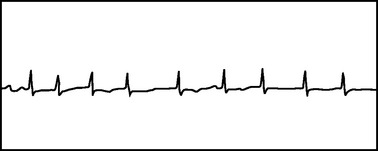
Atrial fibrillation (AF) is the most common supraventricular tachyarrhythmia with a concerning amount of possible detrimental consequences. Atrial fibrillation and flutter account for greater than 60% of the supraventricular tachyarrhythmias in noncardiac surgical patients and affect up to 40% of patients following cardiac surgery. It is commonly associated with left atrial distension, whether from acute fluid shifts or chronic dilatation secondary to structural heart disease. Other associations that must be ruled out include electrolyte imbalances, myocardial ischemia, hyperthyroidism, hypoxia/hypercarbia, pulmonary embolus, and pneumonia. It is an “irregularly irregular” rhythm with an absence of P waves on ECG (Figure 7). It is thought to arise from multiple shifting re-entrant circuits that bombard the AV node with a multitude of impulses, from which only a proportion initiate ventricular contraction, 110–190 beats/min. Patients without structural heart disease tolerate the loss of the atrial component of ventricular filling quite well, but in those with this history, hypotension, acute congestive failure, and myocardial ischemia can be precipitated. Another concerning consequence is the possibility of mural thrombus formation, and the associated embolic risk, from within the noncontracting left atrium. Thrombus can occur in up to 10% of patients, with new-onset AF lasting longer than 3 days.
The risk of atrial thrombus and emboli become more concerning over time in AF, and anticoagulation therapy should be considered if return to sinus rhythm has not occurred after 48–72 hours. The potential benefits of anticoagulation must be weighed against the risk of postoperative bleeding. The embolic risk is increased when transition occurs from AF to sinus rhythm and vice versa. Typically, anticoagulation is recommended for 3–4 weeks prior to elective electrical cardioversion. If earlier cardioversion is required, it can be performed safely with only 48 hours of anticoagulation if atrial thrombus is ruled out via transesophageal echocardiogram. If this test is positive for atrial thrombus, anticoagulation should be continued for 4–6 weeks, and resolution of thrombus should be proven prior to elective cardioversion.
Ventricular Tachyarrhythmias
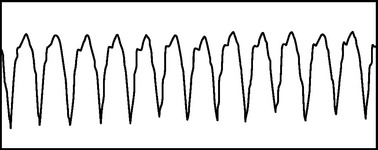
Ventricular tachycardia (VT) is classified into monomorphic and polymorphic subtypes. Monomorphic VT is thought to originate from a single ventricular focus and has a wide QRS pattern, each with similar morphology (Figure 8). Polymorphic VT, in contrast, is characterized by an irregular, undulating appearance, with significant variation in QRS morphology. Differentiation is important because polymorphic VT commonly degenerates to VF. Further classification is determined by the persistence of the rhythm. Compared with sustained VT, nonsustained VT typically lasts less than 30 seconds and spontaneously terminates.
Monomorphic Ventricular Tachycardia
The acute management for monomorphic VT is dependent on the hemodynamic status of the patient. Direct-current cardioversion is the mainstay of treatment for those symptomatic or unstable. Electric cardioversion is highly effective and is also recommended for hemodynamically stable VT in conjunction with adequate short-term anesthesia. In those patients who are stable, or where electric cardioversion is not appropriate or available, either intravenous procainamide, sotalol, or amiodarone are the current antiarrhythmic drug recommendations. Amiodarone is the drug of choice for those patients with impaired cardiac function. An important change from the most recent ACLS guidelines is that lidocaine is no longer recommended as a first-line treatment. Antitachycardia pacing is also an option in those with transvenous or an internal pacemaker already in place, although the potential for tachycardia acceleration exists and a defibrillator should be at the bedside if attempted.
Polymorphic Ventricular Tachycardia
Polymorphic VT in the setting of a prolonged QT interval (QT 460 milliseconds) is commonly referred to as the syndrome of torsades de pointes or “twisting of the points.” The ECG shows a wide QRS tachycardia that appears to twist around the ECG baseline. This syndrome requires a different management algorithm because the mechanism is attributed to triggered activity secondary to early after-depolarizations rather than re-entry. Acquired QT prolongation can result from many electrolyte abnormalities and a myriad of medications. Common causes seen in an ICU setting include hypokalemia, hypomagnesemia, specific antibiotics and psychoactive drugs, and, most importantly, class I and III antiarrhythmics (Table 2). The first priority in the management of torsades is identification and removal of the offending agent concurrent with correction of any electrolyte abnormalities. Direct-current cardioversion is used for the hemodynamically unstable, and it is important that any medication that could further prolong the QT interval not be given. Intravenous magnesium should be given to all patients with suspected torsades. Because the length of the QT interval is proportional to the R-R interval (time between each beat), patients benefit from overdrive pacing with isoproterenol or transvenous pacing. Isoproterenol should be used with caution in patients with coronary vascular disease. Antiarrythmic drugs that do not prolong the QT internal can be used and include lidocaine and phenytoin. Long-term management depends on avoiding the use of drugs that prolong the QT interval. The overall prognosis is good, and no long-term therapy is typically recommended.
Table 2 Common ICU Drugs That Can Promote Torsades de Pointes
| Drug Class | Examples |
|---|---|
| Antiarrhythmics | Procainamide, quinidine, amiodarone, sotalol, ibutilide |
| Antimicrobial | Erythromycin, trimethoprim-sulfamethoxazole |
| Psychoactive | Haloperidol, lithium, chloral hydrate, tricyclic antidepressants |
| Miscellaneous | Tacrolimus, vasopressin |
Adapted from Parrillo J, Dellinger R, editors: Critical Care Medicine: Principles of Diagnosis and Management in the Adult, 2nd ed. St. Louis, Mosby, 2001.
Bernard EO, et al. Ibutilide versus amiodarone in atrial fibrillation: a double-blinded, randomized study. Crit Care Med. 2003;31(4):1031-1034.
Blomstrom-Lundqvist C, et al. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias—executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients with Supraventricular Arrhythmias). Circulation. 2003;108(15):1871-1909.
Chung MK. Cardiac surgery: postoperative arrhythmias. Crit Care Med. 2000;28(Suppl 10):N136-N144.
Curtis AB, et al. Clinical factors that influence response to treatment strategies in atrial fibrillation: the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) study. Am Heart J. 2005;149(4):645-649.
Delle Karth G, et al. Amiodarone versus diltiazem for rate control in critically ill patients with atrial tachyarrhythmias. Crit Care Med. 2001;29(6):1149-1153.
European Resuscitation Council. Part 6: advanced cardiovascular life support. Section 5: pharmacology I: agents for arrhythmias. Resuscitation. 2000;46(1–3):135-153.
European Resuscitation Council. Part 6: advance cardiovascular life support. Section 7: algorithm approach to ACLS emergencies. 7A: principles and practice of ACLS. Resuscitation. 2000;46(1–3):163-166.
European Resuscitation Council. Part 6: advanced cardiovascular life support. Section 7: algorithm approach to ACLS. 7C: a guide to the international ACLS algorithms. Resuscitation. 2000;46(1–3):169-184.
European Resuscitation Council. Part 6: advanced cardiovascular life support. Section 7: algorithm approach to ACLS emergencies. 7D: the tachycardia algorithms. Resuscitation. 2000;46(1–3):185-193.
Fuster V, et al. ACC/AHA/ESC guidelines for the management of patients with atrial fibrillation: executive summary. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines and Policy Conferences (Committee to Develop Guidelines for the Management of Patients with Atrial Fibrillation): developed in collaboration with the North American Society of Pacing and Electrophysiology. J Am Coll Cardiol. 2001;38(4):1231-1266.
Hersi A, Wyse DG. Management of atrial fibrillation. Curr Probl Cardiol. 2005;30(4):175-233.
Hollenberg SM, Dellinger RP. Noncardiac surgery: postoperative arrhythmias. Crit Care Med. 2000;28(Suppl 10):N145-N150.
Kaushik V, et al. Bradyarrhythmias, temporary and permanent pacing. Crit Care Med. 2000;28(Suppl 10):N121-N128.
Mason PK, et al. Influence of the randomized trials, AFFIRM and RACE, on the management of atrial fibrillation in two university medical centers. Am J Cardiol. 2005;95(10):1248-1250.
McNamara RL, et al. Management of atrial fibrillation: review of the evidence for the role of pharmacologic therapy, electrical cardioversion, and echocardiography. Ann Intern Med. 2003;139(12):1018-1033.
Ramaswamy K, Hamdan MH. Ischemia, metabolic disturbances, and arrhythmogenesis: mechanisms and management. Crit Care Med. 2000;28(Suppl 10):N151-N157.
Reinelt P, et al. Incidence and type of cardiac arrhythmias in critically ill patients: a single center experience in a medical-cardiological ICU. Intensive Care Med. 2001;27(9):1466-1473.
Singh BN. Atrial fibrillation following investigation of rhythm management: AFFIRM trial outcomes. What might be their implications for arrhythmia control? J Cardiovasc Pharmacol Ther. 2002;7(3):131-133.
Trappe HJ, Brandts B, Weismueller P. Arrhythmias in the intensive care patient. Curr Opin Crit Care. 2003;9(5):345-355.
Trohman RG. Supraventricular tachycardia: implications for the intensivist. Crit Care Med. 2000;28(Suppl 10):N129-N135.