Chapter 96 The critically ill child
The chapters on paediatric intensive care are intended to help intensivists outside specialised paediatric centres manage common paediatric emergencies. They should be read in conjunction with relevant adult chapters, as there are areas of common interest. Some common neonatal emergencies are also presented.
The major differences between paediatric and adult patients are described below.
PAEDIATRIC INTENSIVE CARE
CARDIORESPIRATORY EVENTS AT BIRTH
During intrauterine life, 60% of blood returning to the right atrium passes directly through the foramen ovale into the left ventricle and ascending aorta. As most of this blood is from the umbilical arteries, the heart and brain are perfused with better-oxygenated blood. Pulmonary vascular resistance (PVR) is high and most of the blood reaching the right ventricle passes through the ductus arteriosus to the descending aorta. Only 10% of right ventricle output passes to the lungs which, although non-functional, require a blood supply for nutrition, growth and development of the lung vasculature.
TRANSITIONAL CIRCULATION
TREATMENT
Many centres successfully employ extracorporeal membrane oxygenation (ECMO) in this situation.
THERMOREGULATION IN THE NEWBORN
Human body temperature is maintained within narrow limits. This is achieved most easily in the thermoneutral zone – the range of ambient temperature within which the metabolic rate is at a minimum. Once ambient temperature is outside the thermoneutral zone, heat production (shivering or non-shivering thermogenesis) or evaporative heat loss processes are required to maintain body temperature within normal limits. Regulatory mechanisms are less effective in the neonate (there is no shivering or sweating), who is otherwise disadvantaged by a high surface area to body weight ratio and lack of subcutaneous tissue.
IMMUNOLOGY OF THE INFANT
The immunological system consists of:
RESUSCITATION OF THE NEWBORN
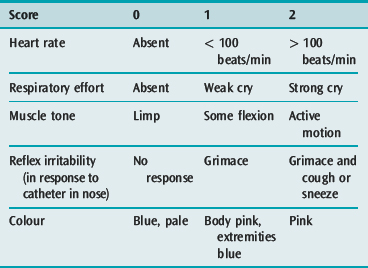
Some newborn infants fail to adapt from fetal to extrauterine life and require immediate cardiopulmonary and cerebral resuscitation. The Apgar scoring system (Table 96.1) scored after 1 minute, remains the most widely accepted method of assessment. The best Apgar score is 10 and the worst is 0. There is an inverse relationship between the Apgar score and the degree of hypoxia and acidosis. It has been suggested that the 5-minute score is a guide to ultimate prognosis but this is questioned. Collection of sequential scores must not delay the institution of resuscitation.
BIRTH ASPHYXIA
MANAGEMENT
Babies suffering mild asphyxia immediately before birth with Apgar scores between 5 and 7 usually respond to stimulation and gentle suction to the nose, mouth and pharynx although oxygen therapy is occasionally required. Babies with moderate asphyxia (Apgar 3–4) usually respond to bag-and-mask ventilation with oxygen. Acid–base status should be determined and sodium bicarbonate administered to restore pH > 7.25. Severely asphyxiated infants (Apgar 0–2) need urgent cardiopulmonary resuscitation (CPR). After airway suction, bag-and-mask ventilation should be followed by rapid orotracheal intubation and positive-pressure ventilation with oxygen. Fear of complications of oxygen therapy must not mitigate against the administration of 100% oxygen at this stage. If the liquor contains thick meconium, it is vital that the pharynx and trachea be suctioned prior to the onset of respiration or application of positive pressure. Meconium aspiration syndrome is a preventable condition that is often difficult to manage.
CARDIORESPIRATORY ARREST IN CHILDREN
Ventricular fibrillation (VF) may be anticipated in the following situations:
The International Liaison Committee on Resuscitation (ILCOR) has developed a consensus statement detailing the science underpinning paediatric and neonatal basic and advanced life support.2 The management of paediatric cardiopulmonary resuscitation is discussed in detail elsewhere in this volume.
VASCULAR ACCESS
INTRAOSSEOUS ACCESS3
Intraosseous infusion has been successfully used in CPR.4
CENTRAL VENOUS CANNULATION AND PRESSURE MONITORING
All routes of central venous cannulation are applicable to infants and children and must be within the skills of paediatric intensivists. The femoral route is sometimes the safest in emergency situations. Catheters utilising the Seldinger technique have greatly increased successful placement. Ultrasonography is useful to determine the exact location of veins. Multilumen catheters are recommended when infusing multiple drugs and for parental nutrition. Complications including catheter-related sepsis are the same as in adults. This risk can be reduced by adherence to a bundle of measures.6 The need for prolonged venous access may warrant regular catheter changes, or surgical implantation of a central venous device (e.g. Infusaport, Broviac or Hickman catheter). Umbilical venous cannulation and passage of the catheter through the sinus venosus to the right atrium is useful in neonatal emergencies.
CARDIAC OUTPUT MEASUREMENT
Cardiac output determination can be performed in small children by dye dilution, thermodilution or Doppler techniques. Unfortunately, errors have been substantial, and the first two techniques are invasive, intermittent and only repeatable within finite limits. Interpretation of results is made difficult or impossible in the presence of intracardiac shunts or valvular incompetence. The dye curve may, in fact, be useful in demonstrating residual intracardiac shunts. Calculation of derived variables is only as accurate as the flow measurement.
A recently developed system (PiCCO, Pulsion Medical Systems AG, Munich, Germany) provides continuous cardiac monitoring even in small infants. Cardiac output is determined both intermittently by transpulmonary thermodilution7 and continuously through arterial pulse contour analysis.8 The system also derives cardiac preload volume, an index of left ventricular contractility, and an estimate of intrathoracic blood volume and extravascular lung water.
PULSE OXIMETRY
DRUG INFUSIONS
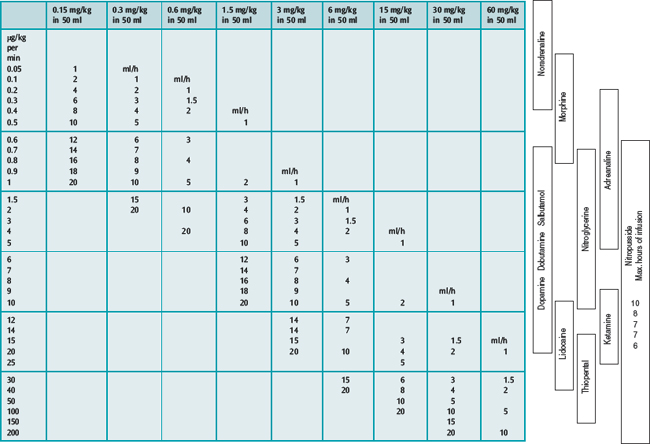
All drugs used in cardiovascular and respiratory support are administered according to body weight; accurate delivery is crucial. Accurate drug infusions require accurate devices, of which syringe pumps are the most useful. Potentially lethal errors in calculating drug dilutions are minimised by the use of dose/dilution/infusion rate guidelines (Table 96.2).9
Table 96.2 Calculation of drug infusion dilutions:
1. Select desired drug dosage to be delivered in μg/kg per min
2. Select infusion rate of syringe pump in ml/h (from centre of table)
3. Calculate number of milligrams of drug to be mixed in 50-ml syringe e.g.: 10-kg child, 0.1–2 μg/kg per min, infusion 1–20 ml/h: put 0.3 ml/kg (= 3 mg) in 50 ml
PAIN RELIEF AND SEDATION IN CHILDREN
Management of pain and agitation in children has received inadequate attention and has tended to be underestimated and underrated. Infants and children are often unable or unwilling to complain of pain. In the past, some believed that the neonate could not perceive pain. It is now clear that even neonates possess all the anatomical and neurochemical systems necessary for pain perception and exhibit physiological and behavioural responses to pain.10 Stress responses associated with pain and agitation may increase morbidity and mortality in critically ill patients. Analgesia can be provided by narcotic infusions, local blocks and regional techniques in children of all ages. Painful procedures in the ICU must always be accompanied by appropriate analgesia. The addition of sedative agents such as benzodiazepines can reduce agitation, minimise harmful stress responses and result in narcotic sparing.
NEONATAL AND PAEDIATRIC EMERGENCY TRANSPORT
Care of critically ill neonates and children necessitates the use of specialised retrieval services linked to neonatal and paediatric ICUs. Retrieval services should offer facilities for specialist consultation in addition to secondary transport. Careful audit of such services is necessary to improve patient outcome.11 The aim of retrieval services is to extend the intensive care facility to peripheral hospitals, allowing stabilisation by experienced personnel prior to rapid transport to a regional centre in the most appropriate vehicle (see Chapter 4). Special considerations such as thermoregulation and oxygen monitoring must be provided for in neonatal transport. Well-designed neonatal emergency transport services have resulted in significant reductions in morbidity and mortality.
OUTCOME OF PAEDIATRIC INTENSIVE CARE
Depending on admission criteria, mortality in paediatric ICUs ranges from 5 to 15%. If patients with pre-existing severe disabilities are excluded, the majority of survivors have a normal or near-normal life expectancy. A number of scoring systems have been developed or modified for paediatric application to predict ICU mortality. These scoring systems allow comparison between different ICUs, internal audits, stratification of patients for research purposes and analysis of cost benefit. The paediatric risk of mortality (PRISM) score12,13 and the paediatric index of mortality (PIM) score14 are applicable to a wide range of critically ill infants and children. Although PRISM performs marginally better, PIM is easier to collect and hence less prone to errors in data collection. PIM also has the advantage that it predicts mortality based on admission parameters whereas PRISM is based on the worst variables in the first 24hours. As many paediatric ICU deaths occur in the first 24hours, PRISM is often recording the dying process rather than predicting it. Specialised scores have been developed for specific problems, e.g. the modified injury severity scale (MISS) and paediatric trauma score (PTS) for paediatric trauma, and the modified Glasgow Coma Scale (GCS) for neurological insults. Numerous scoring systems have been developed for meningococcaemia, the best validated being the Glasgow meningococcal septicaemia prognostic score (GMSPS).15
Compared with adult intensive care, children with equivalent therapeutic intervention scores (TISS) have a lower in-hospital and 1-month mortality.16 In addition, non-survivors do not consume a disproportionate amount of resources. While multiple organ failure increases mortality, the prognosis is considerably better than for adults.17 There is evidence that mortality is lower in specialist paediatric ICUs,18 and that paediatric ICUs with a larger workload have better outcomes than those looking after fewer children.19 General hospitals should therefore have facilities for urgent resuscitation of children prior to early transport to a specialised paediatric ICU. Unless unavoidable, critically ill children, particularly those requiring mechanical intervention, should not be cared for in an adult ICU for longer than 24 hours. The American Academy of Pediatrics, the Society of Critical Care Medicine, the British Paediatric Association and the Australian National Health and Medical Research Council have all stated that children should receive intensive care in specialist paediatric units.
1 Kinsella JP, Neish SR, Dunbar ID, et al. Clinical responses to prolonged treatment of persistent pulmonary hypertension of the newborn with low doses of inhaled nitric oxide. J Pediatr. 1993;123:103-108.
2 The International Liaison Committee on Resuscitation. The International Liaison Committee on Resuscitation (ILCOR) Consensus on Science with treatment recommendations for pediatric and neonatal patients: pediatric basic and advanced life support. Pediatrics. 2006;117:955-977.
3 Rosetti VA, Thompson BM, Miller J, et al. Intraosseous infusion: an alternative route of pediatric intravascular access. Ann Emerg Med. 1985;14:885-888.
4 Saccheti AD, Linkenheimer R, Liberman M, et al. Intraosseous drug administration: successful resuscitation from asystole. Pediatr Emerg Care. 1989;5:97-98.
5 Moscati R, Moore GP. Compartment syndrome with resultant amputation following intraosseous infusion. Am J Emerg Med. 1990;8:470-471.
6 Bernholtz SM, Pronovost PJ, Lipsett PA, et al. Eliminating catheter-related bloodstream infection in the intensive care unit. Crit Care Med. 2004;32:2014-2020.
7 McLuckie A, Murdoch IA, Marsh MJ, et al. A comparison of pulmonary and femoral artery thermodilution cardiac indices in paediatric intensive care patients. Acta Paediatr. 1996;85:336-338.
8 Goedje O, Hoeke K, Lichtwarek-Aschoff M, et al. Continuous cardiac output by femoral arterial thermodilution calibrated pulse contour analysis: comparison with pulmonary arterial thermodilution. Crit Care Med. 1999;27:2407-2412.
9 Shann F. Continuous drug infusions in children: a table for simplifying calculations. Crit Care Med. 1983;11:462-463.
10 Anand KJS, Hickey PR. Pain and its effects in the human neonate and fetus. N Engl J Med. 1987;317:1321-1329.
11 Henning R, McNamara V. Difficulties encountered in transport of the critically ill child. Pediatr Emerg Care. 1991;7:133-137.
12 Pollack MM, Ruttimann UE, Getson PR. Pediatric risk of mortality (PRISM) score. Crit Care Med. 1988;16:1110-1116.
13 Pollack MM, Patel KM, Ruttimann UE. PRISM III: an updated pediatric risk of mortality score. Crit Care Med. 1996;24:743-752.
14 Shann F, Pearson G, Slater A, et al. Paediatric index of mortality (PIM): a mortality prediction model for children in intensive care. Intensive Care Med. 1997;23:201-207.
15 Thompson APJ, Sills JA, Hart A. Validation of the Glasgow meningococcal septicaemia prognostic score: a 10 year retrospective survey. Crit Care Med. 1991;19:26-30.
16 Yeh TS, Pollack MM, Holbrook PR, et al. Assessment of pediatric intensive care – application of the Therapeutic Intervention Scoring System. Crit Care Med. 1982;10:497-500.
17 Wilkinson JD, Pollack MM, Ruttimann UE, et al. Outcome of pediatric patients with multiple organ system failure. Crit Care Med. 1986;14:271-274.
18 Pollack MM, Alexander SR, Clarke N, et al. Improved outcomes from tertiary center pediatric intensive care: a statewide comparison of tertiary and nontertiary care facilities. Crit Care Med. 1991;19:150-159.
19 Pearson G, Shann F, Barry P, et al. Should paediatric intensive care be centralized? Trent versus Victoria. Lancet. 1997;349:1214-1217.