chapter 4
The Cranial Nerves and Understanding the Brainstem
THE ‘RULE OF 4’
The first section of this chapter will describe the anatomy, the techniques for examining the individual cranial nerves and the more common abnormalities encountered. The second part will discuss the ‘Rule of 4’ to aid in localising the problem within the brainstem, in particular understanding brainstem vascular syndromes [1].
THE OPTIC NERVE, CHIASM, RADIATION AND THE OCCIPITAL CORTEX
The visual pathways together, with the visual field abnormalities produced by lesions at certain sites along the pathway, are illustrated in Figure 4.1. Note that the lateral retina radiates back to the occiput on the same side via the optic nerve, chiasm and optic radiation, while the fibres from the medial retina cross at the optic chiasm and radiate to the opposite occipital lobe. The left occipital lobe receives fibres from the left lateral retina and the right medial retina (i.e. the right visual field), while the opposite is the case for the right occipital lobe.
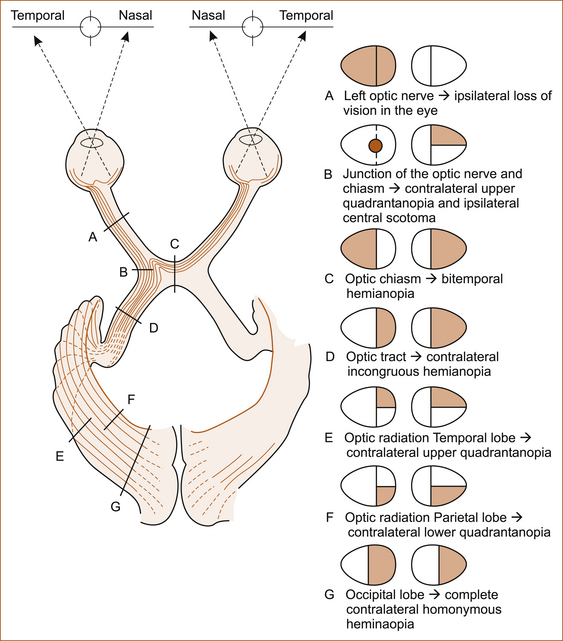
An optic nerve lesion will produce a visual field loss in one eye. The optic chiasm lies above the pituitary gland and beneath the hypothalamus and is subject to compression from pituitary and hypothalamic tumours. Lesions of the optic chiasm will produce a bitemporal field loss. An optic radiation or occipital lobe problem will result in a contralateral visual field loss, either a hemianopia (loss of one-half of the visual field) or a quadrantanopia (loss of one-quarter of the visual field).
Methods of testing
The visual acuity in each eye is assessed with glasses on (corrected) and glasses off (uncorrected) using a Snellen chart (see Figure 4.2). In patients with a neurological problem it is preferable to check the acuity corrected to remove any ocular refractive error contributing to visual impairment. In the absence of glasses, impaired vision due to a refractive error can be corrected by asking the patient to look through a small hole in a piece of cardboard or paper. This will improve the vision if impairment is related to a refractive error in the eye.
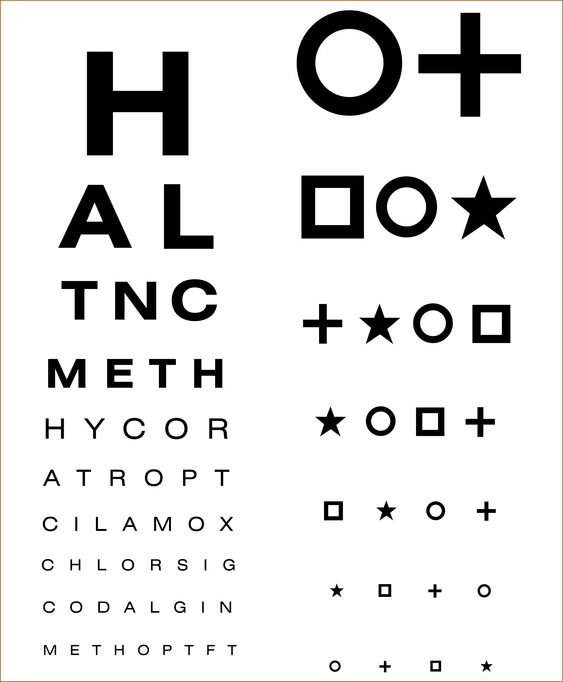
FIGURE 4.2 Snellen visual acuity chart
COLOUR VISION
The Ishihara charts (Figure 4.3) are used to check colour vision. Colour blindness is most often hereditary, and there are two distinct patterns of impairment:
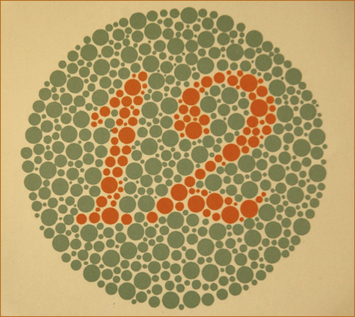
FIGURE 4.3 Ishihara sample chart
• If the patient is a protanope, colour blindness is characterised by defective perception of red and confusion of red with green or bluish green.
• If the patient is a deuteranope, color blindness is characterised by insensitivity to green.
Pathological colour blindness indicates disease in the optic nerves and can occur even in the absence of prior visual symptoms, typically with a demyelinating optic neuropathy associated with multiple sclerosis.
THE VISUAL FIELDS
Severe visual field loss: quadrantanopia, hemianopia, visual inattention
To differentiate between these two possibilities, the examiner’s finger is moved in one visual field at a time. If the visual disturbance is a loss of vision, the finger will not be seen until it reaches the midline. On the other hand, if the visual problem is inattention the single moving finger will be seen in the areas of vision where it could not initially be seen with double simultaneous stimuli. Once again, this is the principle of testing from the area of abnormality until normality is found to define the exact pattern of impairment.
CENTRAL SCOTOMA: To detect more subtle defects of the visual fields at the bedside a 4-mm red pin is used. In this test the examiner holds the pin at a distance midway between himself and the patient. The visual field of the examiner is used as a normal control. The visual fields are tested with the patient covering the left eye, for example, while the examiner covers the right eye, directly opposite the patient’s closed eye. The patient and the examiner look directly into each other’s eye and in this way the examiner can tell if the patient’s eye is moving during the test. Initially the 4-mm red pin is placed in the centre of the visual field to detect if there is a loss of central vision, a central scotoma. If there is a loss of vision in the centre, the pin is moved slowly away in each of the 4 quadrants in turn until it is visualised by the patient, establishing the size of the central scotoma. This indicates a lesion of the fovea in the eye.
ENLARGED BLIND SPOT: An enlarged blind spot occurs with a lesion of the optic discs (either optic neuritis or papilloedema). To detect an enlarged blind spot, the examiner slowly moves the 4-mm red pin out laterally from the centre at the level of the equator of the eye until the blind spot is detected. Once found, the examiner moves the pin up, down, medially and laterally until the size of the patient’s blind spot is established and compared with that of the examiner.
SUBTLE HEMIANOPIA, QUADRANTANOPIA OR BITEMPORAL HEMIANOPIA: To test the visual fields for a subtle hemianopia, quadrantanopia or bi-temporal hemianopia, the examiner moves the pin slowly from the periphery to the midline in each of the 4 quadrants asking the patient to indicate when the red pin is first noticed. If a loss is detected with this technique, the pin is then moved slowly from the area of abnormal vision to normal vision to establish the exact pattern of visual loss. Testing the visual fields individually with the 4-mm red pin will NOT detect visual inattention.
A Goldman Perimeter or Bjerum Screen is used to formally test the visual fields.
EXAMINATION OF THE OPTIC FUNDI
The patient is instructed to look straight ahead, preferably at a small dot or mark on the wall. The examiner approaches from the side at about 30–45° lateral to the midline until a retinal blood vessel is visualised and this is traced back to the optic disc (Figure 4.4). The blood vessels can be traced outwards from the optic disc to detect any abnormality. To examine the fovea (central vision), the patient looks directly at the ophthalmoscope with the intensity of the light reduced.
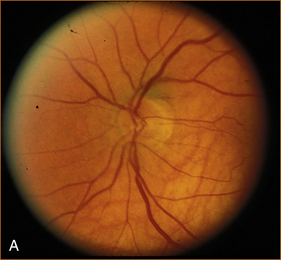
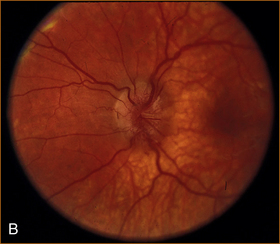
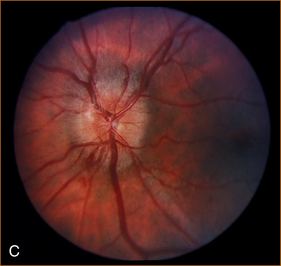
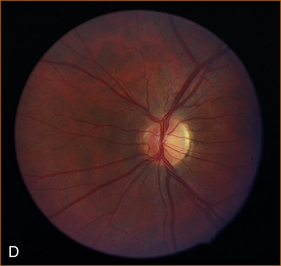
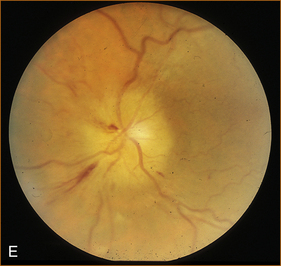
FIGURE 4.4 Normal optic disc and the more common abnormalities of the optic discs
A Normal optic disc
B Papilloedema
The visual acuity is normal unless the papilloedema is chronic, and the blind spot is enlarged. The visual fields are otherwise normal. The pupillary responses are normal.
C Acute optic neuritis
The visual acuity is markedly impaired; colour vision is abnormal if the patient can read the chart (severe visual impairment will prevent the patient from seeing the numbers on the chart). The blind spot is enlarged. The direct pupillary response is slow and there is a Marcus–Gunn pupillary phenomenon (the pupil contracts promptly when the light is shone in the normal eye and when the light is shone in the abnormal eye the pupil initially dilates and then slowly contracts). Retrobulbar neuritis is the term applied to an inflammatory optic nerve lesion within the optic nerve but not affecting the optic nerve head, the part of the optic nerve that is visualised on examination of the fundus. In this situation, the visual acuity and colour vision are impaired, the visual field defect is usually a central scotoma although it may be a diffuse, lateral, superior or inferior defect. The fundus looks normal [3].
D Long-standing optic neuritis with pallor of the optic disc
The visual acuity is reduced, colour vision is abnormal, and a Marcus–Gunn pupillary phenomenon is present (see 4C for an explanation of this abnormality).
E Anterior ischaemic optic neuropathy (AION)
AION is the most common cause of acute optic neuropathy among older persons. It can be non-arteritic (nonarteritic anterior ischaemic optic neuropathy [NAION]) or arteritic, the latter being associated with giant cell arteritis. Visual loss usually occurs suddenly, or over a few days at most, and it is usually permanent. The optic disc is pale and swollen and there are flame haemorrhages.
THE 3RD, 4TH AND 6TH CRANIAL NERVES
ANATOMY
The 3rd nerve nucleus is in the midbrain close to the midline, and the nerve exits the brainstem at the junction of the midbrain and pons just lateral to the midline (see Figure 1.6). It then crosses the subarachnoid space and, after traversing the cavernous sinus, it enters the orbit through the superior orbital fissure. The posterior communicating artery lies close to the nerve and this artery is a common site for berry aneurysm formation which can cause a 3rd nerve palsy.
The trochlear (4th) nerve
The 4th nerve nucleus is in the paramedian midbrain. The fibres of the 4th nerve cross the midline in the posterior aspect of the midbrain and emerge adjacent to the crus cerebri (see Figure 1.6). The 4th nerve passes through the cavernous sinus and enters the orbit via the superior orbital fissure. It supplies the superior oblique (SO) muscle that depresses the eye when it is in the adducted position and internally rotates the eye when it is looking laterally (abducted) and down. Fourth nerve palsies are commonly associated with lesions of the other oculomotor nerves due to their proximity in the cavernous sinus and orbit; an isolated 4th nerve palsy is rare but can be congenital in origin or the result of trauma.
The abducent (6th) nerve
The 6th nerve nucleus lies within the pons (encircled by the 7th cranial nerve). It exits the pons laterally at the junction of the pons and medulla (see Fig. 1.6). It crosses the subarachnoid space, passes through the cavernous sinus and enters the orbit via the superior orbital fissure to supply the lateral rectus (LR) muscle. The close proximity between the 6th nerve nucleus and the 7th nerve within the pons means it is very unusual to have an isolated 6th nerve lesion with disease within the pons. Most often a 6th nerve palsy indicates a lesion directly affecting the nerve, but occasionally it can be a false localising sign due to raised intracranial pressure. A 6th nerve palsy results in an inability to abduct (move the eye laterally within the orbit) the eye fully (see Figure 4.5).
METHOD OF TESTING
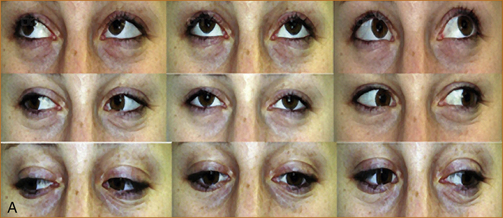
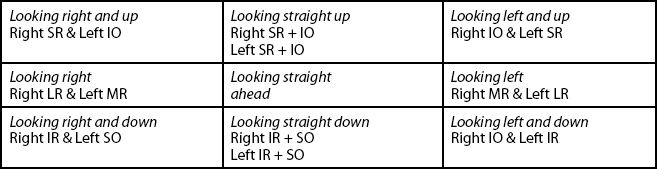
A Normal full ocular movements all directions
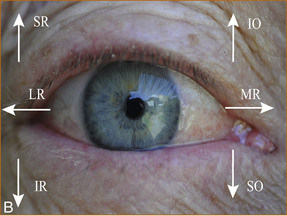
B The direction of action of the individual ocular muscles in the right eye
IO = inferior oblique, IR = inferior rectus, LR= lateral rectus, MR = medial rectus, SO = superior oblique, SR = superior rectus
Note: It is important to examine up gaze in the primary position (looking straight ahead) and also in the direction of action of each individual ocular muscle as shown.
CONTROL OF EYE MOVEMENTS, THE PUPIL AND EYELID OPENING: SYMPATHETIC AND PARASYMPATHETIC INNERVATION OF THE PUPIL AND EYELID
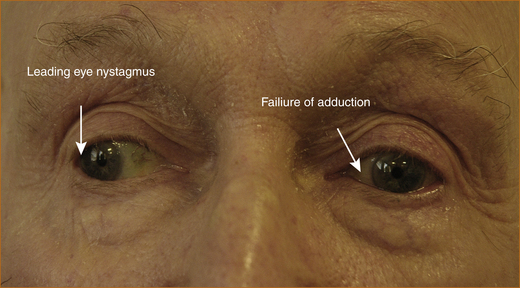
When a patient complains of diplopia it is important to clarify whether they actually are seeing double as some patients use the term ‘double vision’ to describe simple blurred vision. Once diplopia is confirmed, the next step is to enquire whether the diplopia is horizontal or vertical. Horizontal diplopia occurs with 6th nerve palsies and an internuclear ophthalmoplegia while vertical diplopia occurs with 3rd or 4th nerve palsies. An internuclear ophthalmoplegia occurs when the eye on the side of the brainstem where the pathology is fails to adduct and there is nystagmus in the contralateral eye as it looks outwards (refer to Figure 4.10).
Methods of examining eye movement
1. The examiner stands in front of the patient and observes the eye movements carefully.
2. The patient is requested to look up as a check for impairment of up gaze. This is a common finding in older patients but it may also represent a supranuclear gaze palsy, which refers to impairment of eye movements due to pathology above the cranial nerve nuclei that innervate the extraocular muscles.
3. The patient is asked to look to the right and then to the left while the examiner observes the eyes to see that there is a full range of horizontal eye movements.
4. The patient is instructed to look up and then down when the eye is fully abducted towards the lateral aspect of the eye and then when it is fully adducted towards the nose.
If the patient complains of double vision there are two methods of determining the cause.
1. Cover testing, where the patient is asked what image disappears when each eye is covered. The patient is asked to look towards an object and, if diplopia occurs, the eyes are covered one at a time and the patient is asked to say whether the image closest or furthest away from the midline disappears. The image that is furthest from the midline is the abnormal one. It is often difficult for the patient to be certain which image disappears.
2. An easier method is to use red–green glasses (see Figure 4.7) and a torch and ask the patient to identify what colour light is furthest from and what colour light is closest to the midline. The light that is furthest from the midline is the abnormal one and reflects the muscle that is affected. For example, in Figure 4.8 showing a left 3rd nerve palsy, when the patient is looking to the right the green image would be furthest to the right indicating weakness of the left medial rectus muscle. If the patient had a left 6th nerve palsy, the green image would be furthest from the midline when they look left.
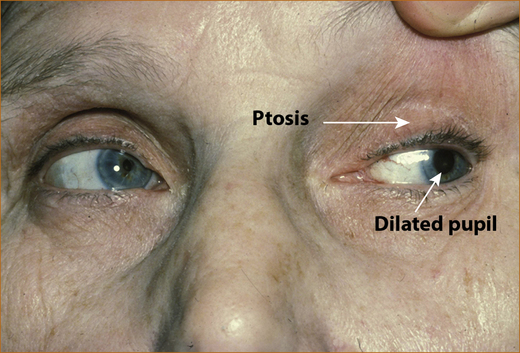
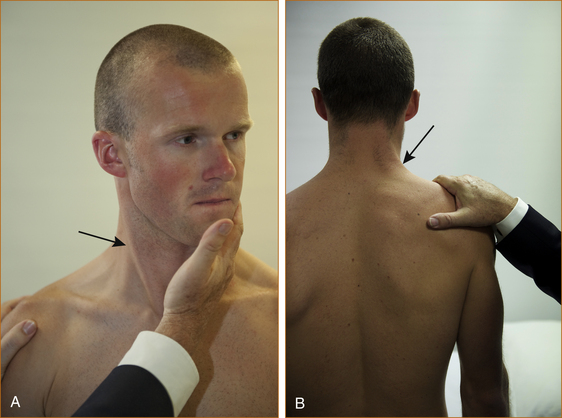
The pupillary reflex
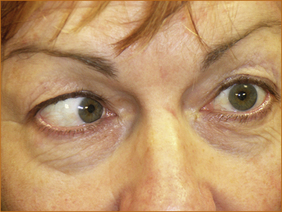
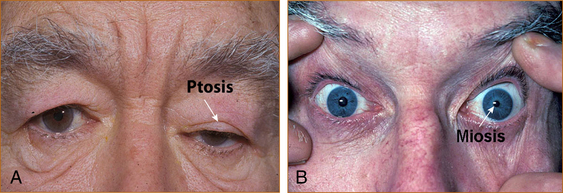
The pupil is innervated by parasympathetic fibres that constrict and sympathetic fibres that dilate the pupil. The parasympathetic fibres are on the surface of the 3rd nerve and a dilated pupil results when these are affected. A constricted pupil occurs when the sympathetic fibres are affected by a disease process. This may occur anywhere along the pathway from their origin in the sympathetic ganglion at the level of the 1st and 2nd thoracic nerve roots up through the neck, where the fibres are closely related to the internal carotid artery, into the cranium, where the fibres are adjacent to the carotid siphon of the internal carotid artery, into the orbit via the superior orbital fissure. Sympathetic fibres also innervate the eyelid. Impairment of the sympathetic pathway will result in mild ptosis and a constricted pupil, known as Horner’s syndrome (see Figure 4.9). Other signs of a Horner’s syndrome that are more subtle and more difficult to elicit are enophthalmos (the eye is partially withdrawn into the eye socket) and reduced or absent sweating (anhydrosis) on that side of the face.
Abnormalities of ocular movements and pupils
Figures 4.5,4.7, 4.9 and 4.10 illustrate the common abnormalities of ocular movements: a 6th and 3rd nerve palsy, a Horner’s syndrome and an internuclear ophthalmoplegia respectively.
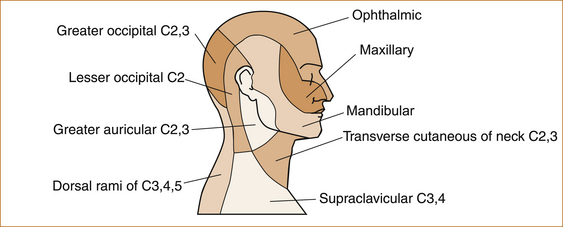
THE TRIGEMINAL (5TH) NERVE
The trigeminal nerve has motor fibres that supply the ipsilateral pterygoid and masseter muscles (the muscles that push open and pull closed the jaw, respectively) and sensory fibres that supply sensation to the anterior one-third to two-thirds of the scalp, forehead, cheek and jaw on the same side, but not the angle of the jaw (see Figure 4.11).The motor fibres are only rarely affected by disease whereas there are many causes of sensory loss on the face. It is important to differentiate between altered sensation on the face due to a trigeminal nerve lesion and a quintothalamic tract lesion (the pathway between the 5th cranial nerve nucleus and the thalamus). The angle of the jaw is spared and the sensory loss affects only the anterior one-third to two-thirds of the scalp with a trigeminal nerve (peripheral nervous system) sensory problem whereas, with a quintothalamic tract (central nervous system) lesion, the sensory loss will extend over the entire (contralateral) scalp and face including the angle of the jaw. As this is almost invariably associated with spinothalamic tract involvement, the sensory loss will also affect the neck, arm and leg on the same side.
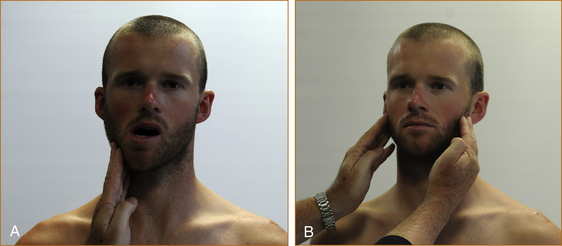
Method of testing
The motor component is tested by asking the patient to protrude the jaw (pterygoid muscles). If it is normal it will protrude in the midline; if there is an abnormal 5th motor nerve the jaw will deviate towards the side of the weak muscle – the side of the lesion. Another technique is to gently push the jaw to the right and then to the left; an inability to resist indicates a contralateral 5th motor nerve lesion. To test the masseter muscles the patient is requested to clench the jaw while the examiner places both hands over the muscles to feel for the contraction (see Figure 4.12). If there is an abnormality the muscle cannot be felt to contract beneath the fingers.
THE FACIAL (7TH) NERVE
The facial nerve nucleus is in the lateral pons of the brainstem. The nerve fibres hook around the 6th nerve nucleus and exit the pons laterally close to the 8th nerve (see Figure 1.6). The nerve then passes across the subarachnoid space and exits the skull through the facial canal and passes through the parotid gland to supply the facial muscles of the forehead, around the eyes (orbicularis oculi), the cheek and around the mouth (orbicularis oris). A branch leaves the nerve before the canal and supplies the stapedius muscle in the middle ear (the nerve to stapedius); if it is affected, for example in a patient with a Bell’s palsy, it causes hyperacusis (increased sensitivity to noise) in the ear. Another branch, the lingual nerve, supplies the sensation of taste to the anterior two-thirds of the tongue; if affected it causes altered taste on the ipsilateral side of the tongue.
Method of testing
Facial movements are tested by asking the patient to show their teeth, close their eyes tightly and then open them wide. This latter command will cause elevation of the eyebrows and differentiates a lower motor from an upper motor facial weakness. The frontalis muscle controls movement of the forehead and has bilateral innervation from the facial nerve. Thus, with an upper motor problem, the patient can still wrinkle the forehead and raise the eyebrows whereas, with a lower motor problem, they cannot (Figure 4.13 shows the difference between upper and lower motor problems).

FIGURE 4.13 A Upper motor neuron facial weakness (note the patient can elevate both sides of the forehead)
B, C Lower motor neuron 7th nerve palsy with an inability to smile, close the eye fully and wrinkle the ipsilateral forehead
The most common lesion affecting the facial nerve is a Bell’s palsy. This typically produces a LMN weakness on the same side of the face and is often, but not invariably, associated with ipsilateral hyperacusis (increased hearing in that ear) and altered taste.
THE AUDITORY/VESTIBULAR (8TH) NERVE
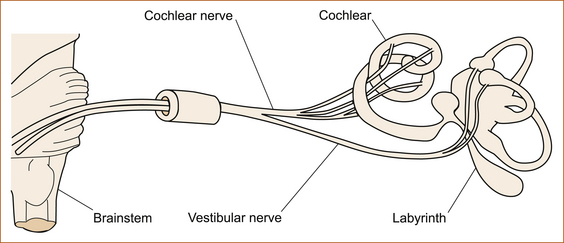
The 8th cranial nerve has two components, the auditory or cochlear (hearing) nerve and the vestibular (balance) nerve (see Figure 4.15). The nerve emerges from the ear canal in the cerebellar–pontine angle, pierces the dura mata (the thick membrane surrounding the brain, just beneath the bone) and transverses the subarachnoid space. It enters the brainstem in the lateral pons where the vestibular and auditory nuclei are situated.
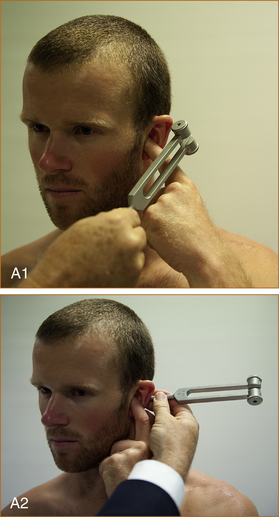
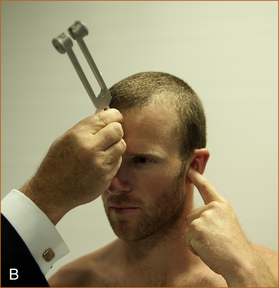
Methods of testing
1. Rustle the patient’s hair that is just above the ear between your fingers.
2. Hold a mechanical watch close to the ear.
3. Whisper numbers in one ear while occluding the opposite ear.
If there is hearing impairment, then it is useful to perform the Weber test and Rinne test using a 256-Hz tuning fork. In the Weber test, the ringing tuning fork is placed in the midline of the forehead. If there is a conduction defect (middle ear problem), the noise will be heard in that ear; on the other hand, if there is an 8th nerve deafness, the noise will be heard in the opposite ear. In the Rinne test, the tuning fork is placed next to the ear and subsequently on the mastoid process. Bone conduction (on the mastoid) is louder than air conduction (next to the ear) when deafness is due to a conduction problem. An easy way to remember the features of these two tests is for examiners to occlude their own external canal and test themselves. Occluding the external canal simulates a conduction defect (see Figure 4.14).
The vestibular pathway
If a patient has the sensation that the head or room is spinning (vertigo), the problem must affect the vestibular pathway (see Figure 4.15), which runs from the ear to the cerebellum or vestibular nuclei in the brainstem and up to the vestibular cortex in the temporal lobe. Practically speaking, most cases of vertigo relate to inner ear problems and, to a lesser extent, cerebellar or brainstem lesions; they are very rarely due to more central pathology. Associated deafness and tinnitus coinciding with the vertigo (and not preexisting, unrelated problems) indicate a problem in the ear while other neurological symptoms such as diplopia, dysarthria, dysphagia, weakness or sensory disturbance point to a problem in the brainstem. Vertigo due to problems in the ear or vestibular nerve is referred to as peripheral vertigo while vertigo related to brainstem or cerebellar problems is referred to as central vertigo. Vertigo is discussed in Chapter 7, ‘Episodic disturbances of neurological function’.
THE GLOSSOPHARYNGEAL (9TH) NERVE
The glossopharyngeal nerve nucleus lies in the lateral part of the medulla; the nerve emerges from the medulla, traverses the subarachnoid space and exits through the jugular foramen in the base of the skull. It supplies sensation to the soft palate and pharynx, together with taste to the posterior two-thirds of the tongue.
THE VAGUS (10TH) NERVE
Method of testing
The patient is requested to say ‘ah’ and movement of the soft palate is observed. If there is a problem with the vagas nerve, the palate will deviate to the opposite side as it is pulled upwards by the normal muscle (see Figure 4.16). This can also be observed with the gag reflex, described above.

FIGURE 4.16 Deviated palate
THE ACCESSORY (11TH) NERVE
THE HYPOGLOSSAL (12TH) NERVE
The hypoglossal nerve nucleus lies adjacent to the midline of the medulla and the nerve emerges from the anterior aspect of the medulla just laterally to the pyramids of the medulla and traverses the subarachnoid space to exit through the hypoglossal canal in the base of the skull to supply the muscle of the ipsilateral half of the tongue.
Method of testing
The patient is asked to protrude the tongue and, as the muscle pushes the tongue forward, the tongue will deviate towards the paralysed side (see Figure 4.18).
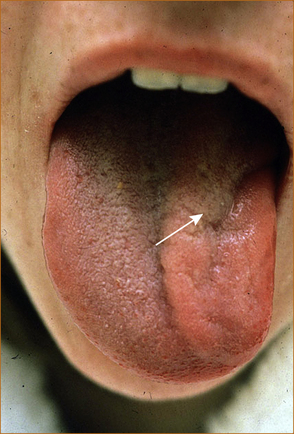
FIGURE 4.18 Wasting and deviation of the protruded tongue to the left due to a left 12th (hypoglossal) nerve palsy
The accompanying DVD demonstrates the techniques for examination of the cranial nerves. The most common disorder to affect the brainstem is cerebrovascular disease. The following discussion entitled the ‘Rule of 4’ is a simplified method for understanding the brainstem and the various vascular syndromes. This has been previously published in the Internal Medicine Journal [1].
THE ‘RULE OF 4’ OF THE BRAINSTEM
Medical students are taught detailed anatomy of the brainstem containing a bewildering number of structures with curious names such as superior colliculi, inferior olives, various cranial nerve nuclei and the median longitudinal fasciculus. In reality a neurological examination can only test a few of these structures. The ‘Rule of 4’ recognises this and describes only those parts of the brainstem that can be examined clinically. The blood supply of the brainstem is such that there are long circumferential branches (the anterior inferior cerebellar artery ‘AICA’, the posterior inferior cerebellar artery ‘PICA’ and the superior cerebellar artery ‘SCA’) and paramedian branches. Involvement of the paramedian branches results in paramedian brainstem syndromes and involvement of the circumferential branches results in lateral brainstem syndromes. Occasionally, medial or lateral brainstem syndromes occur with ipsilateral vertebral occlusion.
The 4 rules of the ‘Rule of 4’
1. There are 4 structures in the ‘midline’ (the paramedian aspect of the midbrain adjacent to the midline) beginning with M:
2. There are 4 structures to the side (lateral) beginning with S:
4. The 4 motor nuclei that are in the midline (actually paramedian) are those that divide (numerically) equally into 12, except for 1 and 2, (5, 7, 9, 10 and 11 are the cranial nerves that are in the lateral brainstem):
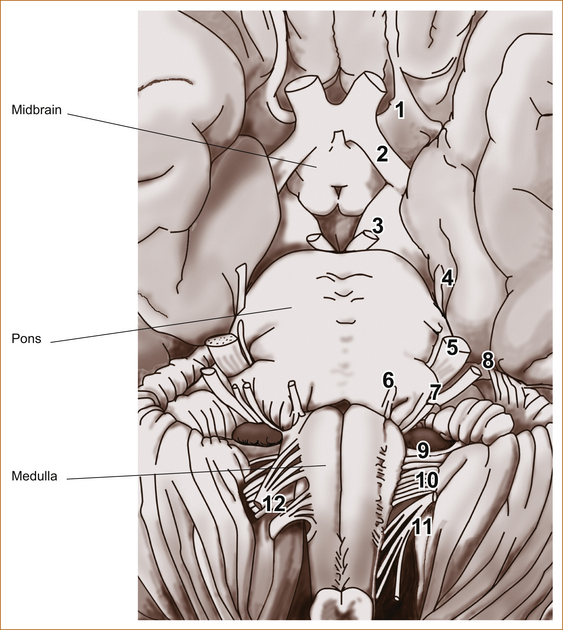
Figure 4.19 depicts a cross-section of the brainstem at the level of the medulla, but the concept of 4 lateral and 4 medial structures also applies to the pons; only the 4 medial structures relate to the midbrain. Figure 4.20 shows the ventral aspect of the brainstem showing the emerging cranial nerves from the midbrain, pons and medulla.
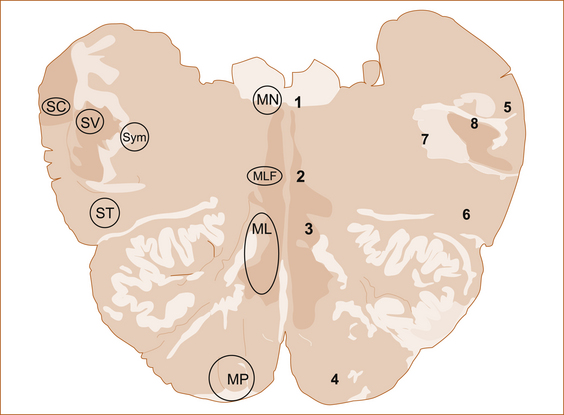
Adapted from Gray’s Anatomy, 34th edn, by E Davies et al, 1967, Longmans, Figure 813, p 1011 [6]
The sizes of the coloured areas do not represent the actual anatomical sizes, but have been made large enough to see and label.
1 MN = motor nucleus (3, 4, 6 or 12), 2 MLF = median longitudinal fasciculus, 3 ML = medial lemniscus, 4 MP = motor pathway (corticospinal tract), 5 SC = spinocerebellar, 6 ST = spinothalamic, 7 SY = sympathetic, 8 SV = sensory nucleus of Vth cranial nerve
The 4 medial structures and the associated deficit
1. The motor pathway (corticospinal tract): contralateral weakness of the arm and leg
2. The medial lemniscus: contralateral loss of vibration and proprioception affecting the arm and leg
3. The medial longitudinal fasciculus: ipsilateral internuclear ophthalmoplegia (failure of adduction of the ipsilateral eye towards the nose and nystagmus in the opposite eye as it looks laterally)
4. The motor nucleus and nerve: ipsilateral loss of the cranial nerve that is affected (3rd, 4th, 6th or 12th)
The 4 lateral structures and the associated deficit
1. The spinocerebellar pathways: ipsilateral ataxia of the arm and leg
2. The spinothalamic pathway: contralateral alteration of pain and temperature affecting the arm, leg and often the trunk
3. The sensory nucleus of the 5th cranial nerve (a long vertical structure that extends in the lateral aspect of the pons down into the medulla): ipsilateral alteration of pain and temperature on the face in the distribution of the 5th cranial nerve (see Figure 4.11)
4. The sympathetic pathway: ipsilateral Horner’s syndrome, i.e. partial ptosis and a small pupil (miosis)
The 4 cranial nerves in the pons and the associated deficit
The 4 cranial nerves above the pons and the associated deficit
1. 1st (olfactory): not in midbrain
2. 2nd (optic): not in midbrain
3. 3rd (oculomotor): impaired adduction, elevation and depression of the ipsilateral eye with or without a dilated pupil; the eye is turned out and slightly down
4. 4th (trochlear): eye unable to look down when looking in towards the nose
The 3rd and 4th cranial nerves are the motor nerves in the midbrain.
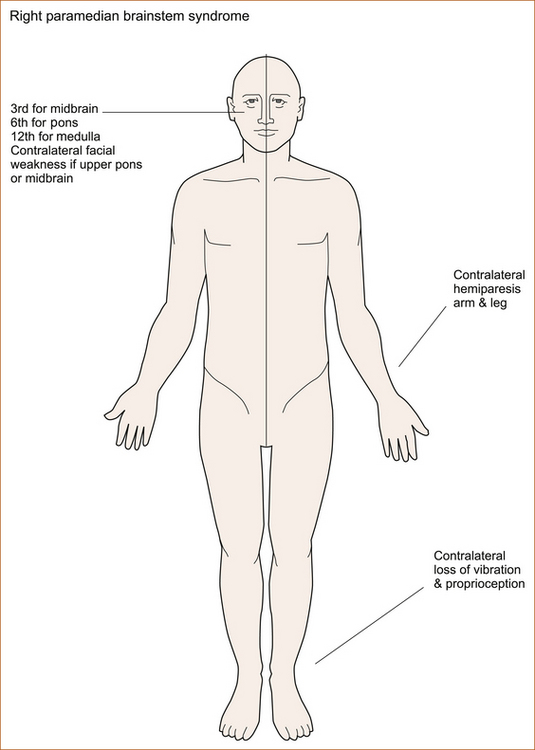
Medial (paramedian) brainstem syndromes
Let us assume that the patient you are examining has a brainstem problem (most often a stroke). If you find UMN signs in the arm and the leg on one side then you know the patient has a contralateral medial brainstem syndrome because the motor pathway is paramedian and crosses at the level of the foramen magnum (at the decussation of the pyramids, where the brainstem meets the spinal cord). The involvement of the motor pathway is the ‘meridian of longitude’. Refer to Figure 4.21 for a summary of the signs. So far the lesion could be anywhere in the medial aspect of the brainstem although, if the face is also affected, it has to be above the mid pons, the level of the 7th nerve nucleus.
The motor cranial nerve, ‘the parallel of latitude’, indicates whether the lesion is in the medulla (12th), pons (6th) or midbrain (3rd). Remember that cranial nerve palsy will be ipsilateral to the side of the lesion and contralateral to the hemiparesis. If the medial lemniscus is also affected, you will find a contralateral (the same side affected by the hemiparesis) loss of vibration and proprioception in the arm and leg as the posterior columns also cross at or just above the level of the foramen magnum.
Lateral brainstem syndromes
Once again we are assuming that the patient you are seeing has a brainstem problem, most likely a vascular lesion. The 4 Ss or ‘meridians of longitude’ will indicate that you are dealing with a lateral brainstem problem, and the cranial nerves or ‘parallels of latitude’ will indicate whether the problem is in the lateral medulla or lateral pons. Refer to Figure 4.22 for a summary of the signs.
A lateral brainstem infarct will result in:
• ipsilateral ataxia of the arm and leg due to involvement of the spinocerebellar pathways
• contralateral alteration of pain and temperature sensation due to involvement of the spinothalamic pathway
• ipsilateral loss of pain and temperature sensation affecting the face within the distribution of the sensory nucleus of the trigeminal nerve (light touch may also be affected with involvement of the spinothalamic pathway and/or sensory nucleus of the trigeminal nerve).
In summary, if one can remember that:
• there are 4 structures in the midline commencing with the letter M
• there are 4 structures in the lateral aspect of the brainstem commencing with the letter S
• the lower 4 cranial nerves are in the medulla
• the middle 4 cranial nerves are in the pons
• the first 4 cranial nerves are above the pons, with the 3rd and 4th in the midbrain
• the 4 motor nerves that are in the midline are the 4 that divide evenly into 12 (except for 1 and 2), i.e. the 3rd, 4th, 6th and 12th
it will be possible to diagnose with pinpoint accuracy brainstem vascular syndromes.
REFERENCES
1. Gates, P. The rule of 4 of the brainstem: A simplified method for understanding brainstem anatomy and brainstem vascular syndromes for the non-neurologist. Intern Med J. 2005;35(4):263–266.
2. Adams, R.D., Victor, M. Principles of neurology. New York: McGraw–Hill Book Company; 1985. [1186].
3. Gerling, J., Meyer, J.H., Kommerell, G. Visual field defects in optic neuritis and anterior ischemic optic neuropathy: Distinctive features. Graefes Arch Clin Exp Ophthalmol. 1998;236(3):188–192.
4. Williams, P.L., et al. Gray’s anatomy, 37th edn. London: Churchill Livingstone; 1989.
5. Moore, K.L., Dalley, A.F. Clinically oriented anatomy, 4th edn. Maryland: Lippincott Williams & Wilkins; 1999.
6. Davies, E., et al. Gray’s anatomy, 34th edn. Longmans; 1967. [1011, Figure 813].