2 The cervical spine
Introduction
Cervicalgia, or neck pain, is a common condition that results in work absenteeism and alteration of daily activities for many adults.1,2 The course of neck pain may be episodic in nature and the condition often fails to resolve completely, resulting in chronic pain. Approximately 20% of patients presenting with musculoskeletal conditions do so with neck pain as their chief complaint3 and, at any one point in time, over 10% of the adult (>30 years) population complain of cervicalgia; it is more predominant in females than males (3:2).1
Radiographs of the cervical spine are often indicated, particularly in those cases that present with acute trauma, or persistent pain4; however, the contrast resolution of x-rays does not allow complete evaluation of the soft tissue structures or bone marrow. In cases where there is suspicion of a space-occupying lesion in the central spinal canal or intervertebral foramen, or concern for bone marrow pathology, magnetic resonance (MR) imaging may be indicated. It is important for clinicians to have an understanding of the appearance of normal cervical spine anatomy on MR imaging as well as an appreciation of the more common conditions that may present in an ambulatory care setting.
History and examination
When eliciting a history from a patient with a chief complaint of neck pain, the clinician should obtain a few important pieces of information, starting with the patient’s age and past history of similar complaint. It is important to ascertain the duration of pain and whether it was related to a traumatic event. With a history of trauma, the clinician should inquire not only about the mechanism of injury but also about the patient’s posture at the time of injury and the direction of the force. The location of the pain, whether diffuse or focal, may also provide an important clue. The presence of radicular symptoms, pain or paraesthesia, and the presence of systemic symptoms such as fever or weight loss are also highly significant.5
Physical examination should include vital signs; assessment of cervical range of motion, both active and passive; testing of all major muscle groups; orthopaedic evaluation, wherein foraminal compression tests and assessment of the thoracic outlet are of particular importance; and neurological examination, which should include a check of long tract signs – cervical myelopathy does not affect just the cervical nerve roots!6,7
Differential diagnosis
Radicular symptoms need to be carefully differentiated from referred or sclerodermal pain and paraesthesia. To this end, in the patient with brachial symptoms, it is important to test the thoracic outlet. Although entrapment by cervical ribs and apical tumours is rare, functional impingement on the cords of the brachial plexus by the anterior and medial scalenes, first rib and pectoralis minor will be a common presentation to the manual physician and can best be differentiated by simple orthopaedic tests such as Adson’s, Reverse Adson’s, Eden’s and Halstead’s manoeuvres.8
Detailed knowledge of upper limb neurology is also useful in differentiating distal from proximal entrapments: all of the major nerves can suffer functional compression syndromes in the elbow and wrist and a combination of history, neurological testing and compression tests can help refine the differential diagnosis without recourse to nerve conduction studies. MR imaging is often a great help in determining the precise cause – this is dealt with in the chapters dealing with the joints of the upper extremity.9,10
A final, and often overlooked, source of pseudoradicular symptoms is myofascial trigger points, which, of course, are radiographically and electromyographically occult. Although they are often a diagnosis of exclusion – or missed altogether – when sufficiently severe, digital pressure will recreate the patient’s symptoms, making the diagnosis easy for the experienced musculoskeletal expert; the deltoid and rotator cuff muscles are particular culprits in this regard and should always be routinely assessed in such cases.11
Clinical indications for diagnostic imaging
Although MR imaging is extremely useful in the evaluation of the osseous and soft tissue structures of the cervical spine, plain film radiography is often the initial imaging procedure. Radiographs are indicated with a history of significant trauma, including axial force to the vertex of the cranium; a fall from a height of 1 m or down five stairs; a high-speed (>110 km/h) motor vehicle accident; or a motorized recreation vehicle accident. The presence of paraesthesias and an inability to actively rotate the head to 45° are other criteria that justify the use of radiography.4
Standard radiographic views of the cervical spine consist of anterior to posterior (AP) open mouth, AP lower cervical and lateral cervical neutral views. Lateral cervical views taken in flexion and extension posture may be useful to evaluate ligamentous instability; however, it is important to first use the basic routine series to screen the patient for contraindications to these dynamic views. In addition, ligamentous laxity may not become radiographically detectable for several (up to 6) weeks owing to patient limitation and muscular guarding.12 MR imaging is indicated for evaluation following a high-speed motor vehicle accident, a fall from a height of 3 m, a closed head injury or in the presence of neurologic signs radiating from the cervical spine.4
There are many non-traumatic causes of cervical spine problems in which radiographs should be obtained; these are detailed in Box 2.01.4 If, ultimately, radiographs are inconclusive, advanced imaging may then be required.
Imaging protocol
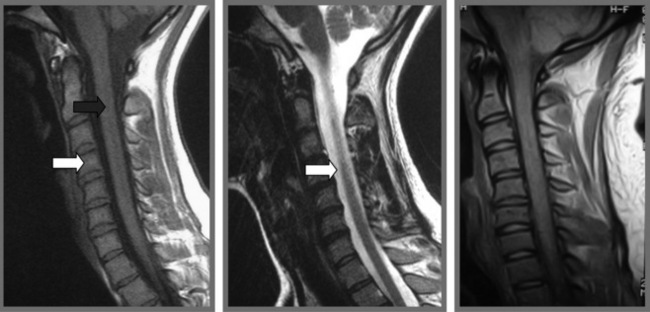
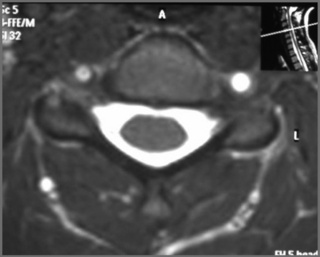
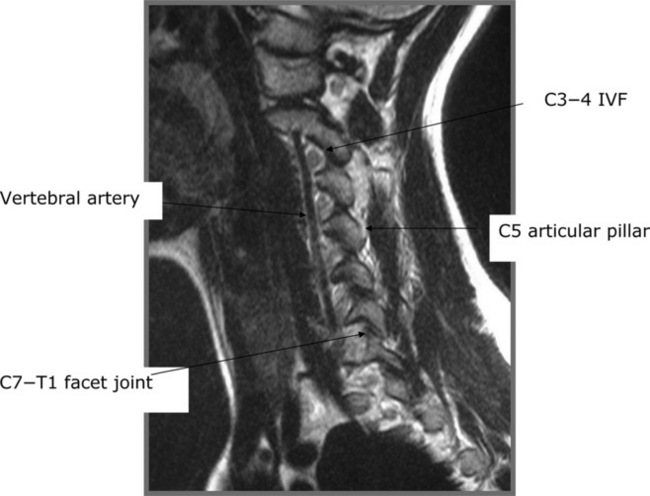
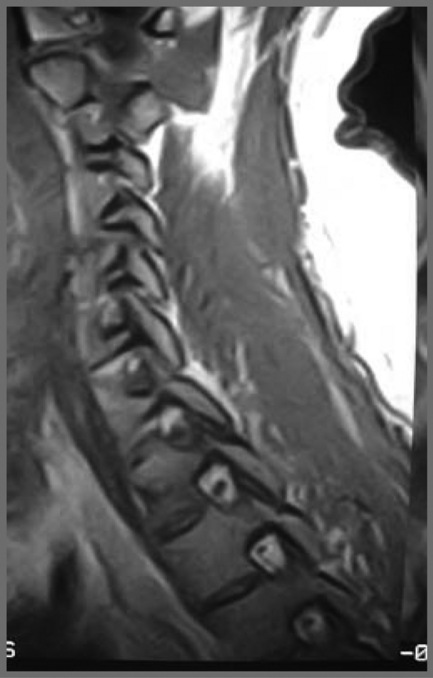
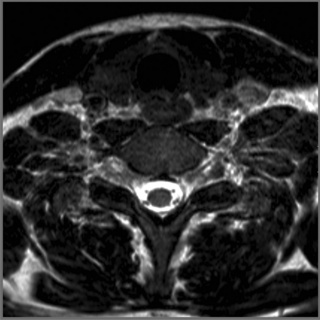
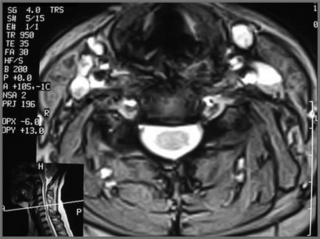
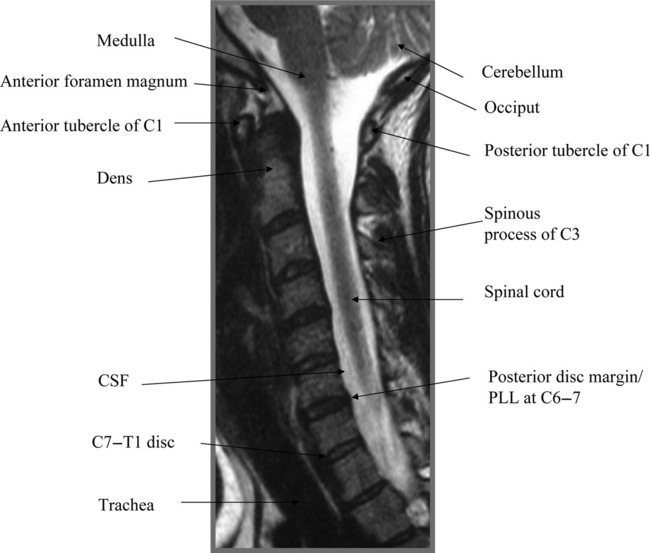
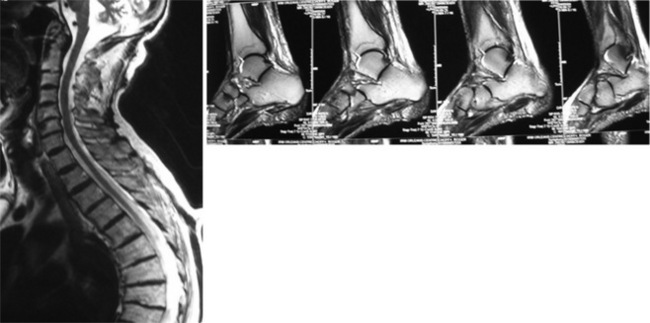
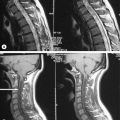
Though protocols vary slightly between facilities, the standard MR imaging protocol for the cervical spine consists of sagittal T1- and T2-weighted images (Figure 2.01) along with axial T2-weighted images (Figure 2.02). Additional short TI inversion recovery (STIR) images may be obtained to suppress the signal from fat (a normal marrow constituent) in order to highlight areas with high water content. Acute fractures, ligamentous injuries, and bony metastasis are all well visualized with STIR imaging (Figure 2.03). Contrast agents, typically chelates of gadolinium, may be utilized in cases where tumour is suspected.13,14
Normal anatomy and variants
Vertebral bodies
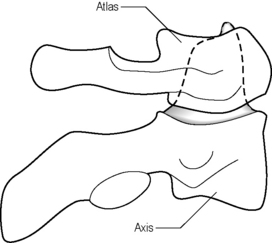
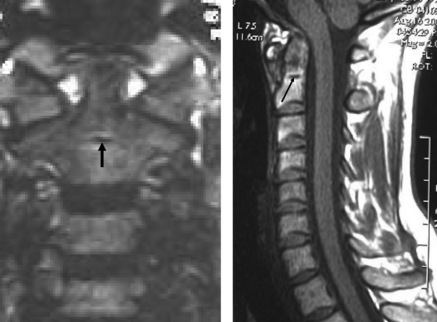
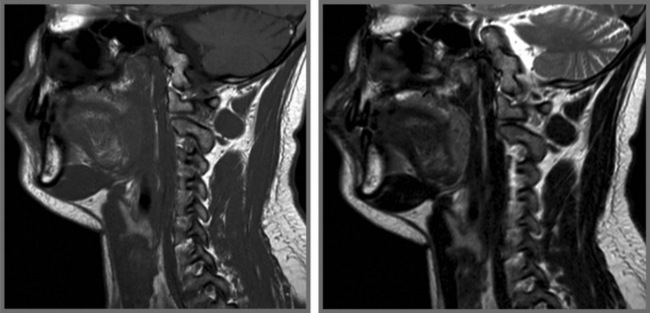
The vertebral bodies from C3–C7 are considered typical vertebral bodies and they share similar characteristics, in general increasing in size from C3 through C7. C1 and C2 are considered atypical as they each have unique characteristics. Their articulation uniquely has no disc; instead, there is an odontoid process, or dens, the cephalic extension of the C2 segment, which forms an articulation with the anterior arch of the ring-shaped C1 (Figure 2.04).15,16 At the base of the dens, a linear area of low signal represents a remnant of the synchondrosis; this is a common finding and should not be mistaken for fracture (Figures 2.05, 2.06).
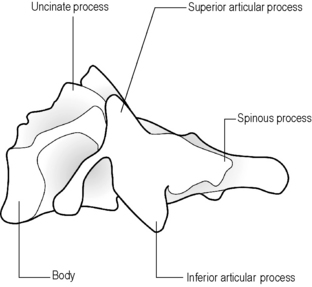
The basivertebral veins enter the posterior aspect of the vertebral bodies, midway between the endplates; although these are most obvious in the lumbar spine, they may be evident on cervical images as well (Figure 2.07). The uncinate processes project superiorly from the lateral aspect of the vertebral bodies from C3 to C7 and, on occasion, from T1, and form the uncovertebral joints, or joints of von Luschka, with the inferior bodies of C2 to C6 (Figures 2.08, 2.09).17,18
The gutter-shaped transverse processes act as guides for the spinal nerves as they exit the intervertebral foramen (IVF) at each level; they also transmit the vertebral arteries. Arising from the subclavian arteries, the vertebral arteries enter the C6 transverse process and ascend to C1. At C1, the vertebral arteries cross over the posterior arch and meet in the midline to form the basilar artery, which continues superiorly through the foramen magnum (Figure 2.10).19,20
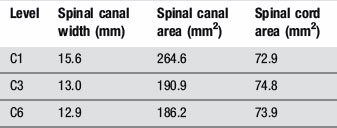
The spinal canal dimension is largest at C1, which allows for protection of the upper cervical cord. According to Steele’s Rule of Thirds, one-third of the spinal canal at C1 is occupied by the spinal cord, one-third by the odontoid process, and one-third comprises the subarachnoid space.21 (More detailed data regarding spinal canal dimensions are given in Table 2.01.22) This results in inherent safeguarding of the spinal cord in the event of transverse ligament rupture or odontoid fracture. This explains why some patients with atlantoaxial instability or subluxation may be relatively asymptomatic. The triangular canal decreases in size to C3 and remains approximately uniform in size from C3 to C7.
Facet joints
The articular processes arise from each side of the posterior arch at the junction of the pedicle and lamina. The superior and inferior articular processes from adjacent levels join to form a diarthrodial, plane facet (zygapophyseal) joint (Figures 2.08, 2.11, 2.12). The articular surfaces are lined by cartilage, the thickness of which varies depending on age, sex and the anatomical level; tiny menisci may also be present in each joint,23 which is surrounded by a synovial-lined, fibroelastic joint capsule.24 The primary role of the facet joint is not to bear weight, but rather to guide, and limit, movement. Because they are innervated by sensory and autonomic nerve fibres, the facet joints may represent a primary source of pain.24
Intervertebral discs
The strongest attachment between vertebral bodies is created by the intervertebral disc, whose main role is to bear weight. In the cervical spine, the lordosis is contributed to by the shape of the intervertebral discs, whose height is greater anteriorly than posteriorly.24 The three regions of the disc are the annulus fibrosus, the nucleus pulposus, and the vertebral body endplate. The annulus fibrosus is composed of fibrocartilage centrally and collagen fibres peripherally.25 The cervical annulus fibrosus is crescent-shaped fibrocartilage that becomes increasingly narrow as it extends laterally and posteriorly.24 The nucleus pulposus lies deep to the annulus and is bound superiorly and inferiorly by the cartilaginous endplates of the adjacent vertebral bodies. The nucleus is formed from glycoproteins and absorbs fluid through the endplates by imbibition, as only the outer region of the annulus fibrosus receives a vascular supply.24 As can be noted in Figure 2.01, the normal intervertebral disc appears as low signal intensity on T1-weighted images and high signal on T2-weighted images. Though these regions of the disc are anatomically distinct, it is not usually possible to distinguish the interface between the inner annulus and the nucleus pulposus with MR imaging.25,26
Spinal ligaments
The role of the spinal ligaments is to connect the vertebral bodies to adjacent segments and to provide smooth motion of the spine. At the same time, these ligaments provide protection for the spinal cord by limiting the amount of intersegmental motion and by acting as shock absorbers during trauma.24,27 Mechanoreceptor afferent fibres in the interspinous and supraspinous ligaments as well as the ligamentum flavum allow them to play an additional proprioceptive role.28 In the cervical spine, the anterior longitudinal ligament (ALL) provides anterior stability; this ligament, which extends from the anterior arch of C1 to the first sacral segment, is adherent to the anterior annulus and to the anterior periosteum of the vertebral bodies. Above C1, the anterior longitudinal ligament continues to the anterior margin of the foramen magnum as the anterior atlanto-occipital membrane (AAM) (Figures 2.13, 2.14). The function of the anterior longitudinal ligament is to limit extension of the cervical spine.17
The posterior longitudinal ligament (PLL) extends from C2 to the sacrum and acts to limit flexion of the spine. It is tightly adherent to the posterior disc and is indistinguishable from the posterior annulus on MR images.26 The PLL is narrower than its anterior counterpart and is attached firmly to the vertebral body edges but not to their bodies. Above C2, the PLL continues to the foramen magnum as the tectorial membrane, which can be injured in traumatic events such as whiplash, although the long-term effect of such damage is not currently established.29–31
Deep to the tectorial membrane, at the junction of the axis (C2) with the atlas (C1), the transverse ligament attaches to the posterior aspect of the C1 lateral masses and acts to hold the odontoid process to the anterior arch of C1. The transverse ligament is part of a cruciate ligament whose superior slip attaches to the anterior foramen magnum and inferior slip attaches to the posterior body of C2 (Figure 2.15).23 Synovial bursae are present between the odontoid process and the anterior arch of C1 and between the odontoid process and the transverse ligament. The odontoid process also attaches to the foramen magnum by the apical and alar ligaments. The apical ligament extends from the tip of the dens to the anterior foramen magnum; the alar ligaments run obliquely from the tip of the dens to the occipital condyles and lateral masses of the atlas.23
The ligamentum flavum connects the laminae at each level, covering the gaps in the posterior wall of the spinal canal and blending with the anterior and medial aspects of the facet joint capsule (Figure 2.16).24 Extending from the external occipital protuberance to the spinous process of C7 and connecting the spinous processes in the cervical spine is the ligamentum nuchae, the cephalic extension of the supraspinous ligament.
Spinal cord and spinal nerves
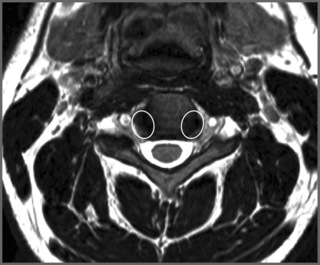
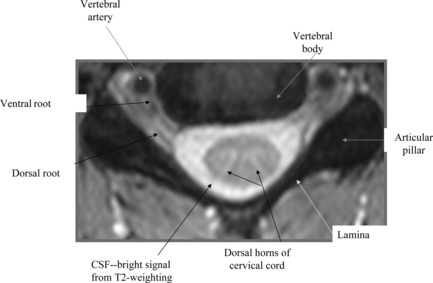
The spinal cord has a characteristic shape in each spinal region; in the cervical spine, it is slightly elliptical in cross-section and demonstrates slight enlargement from C3 to C6.23 It is best assessed on T2-weighted images, which create contrast between the cord and surrounding cerebrospinal fluid (CSF) (Figures 2.17, 2.18). T2-weighted images are also useful in screening for medullary signal abnormalities (Figure 2.19).
The cervical spine gives rise to eight spinal nerves, each composed of a dorsal sensory root and a ventral motor root. The nerves exit through the IVFs formed by adjacent vertebral bodies and are named by the inferior segment: thus, the first nerve exits between the occiput and C1; the second between C1 and C2 and so on. The eighth cervical nerve exits between C7 and T1; thereafter, the nerves are named for the superior segment. The dorsal root is the larger and contains the dorsal root ganglion before joining the ventral root and forming a spinal nerve.26 In the cervical spine, the dorsal root ganglion lies in the IVF at all levels except C1 and C2 (where there is no IVF), where the dorsal root ganglions lie instead on the respective posterior arch.26
The dorsal root of the nerve lies near the superior articular process whilst the ventral root lies adjacent to the uncovertebral joint and posterior to the intervertebral disc.23 On sagittal images, the nerve roots will be found in the inferior portion of the IVF. The cerebellar tonsils will be also visualized on the sagittal images and their relationship with the skull base should be assessed. The cerebellar tonsils should not project more than 5 mm below the foramen magnum in adults.32
Pathological conditions
Intervertebral disc herniation
Cervical disc herniations are a relatively common disorder, affecting 5.5 out of 100,000 people in the United States.33 Disc herniations are more common in adult populations, with males affected more often than females. The C6/7 and C5/6 levels are most commonly involved.32,33
On MR images, the disc should normally lie in line with the edge of adjacent vertebral bodies. A disc bulge is defined as extension of disc material beyond the adjacent vertebral body edges, involving over 50% of the circumference of the disc.34 A disc herniation is extension of disc material that involves less than 50% of the circumference of the disc. If the herniation is broader at its base than at any point distal to its base, it is considered a disc protrusion.
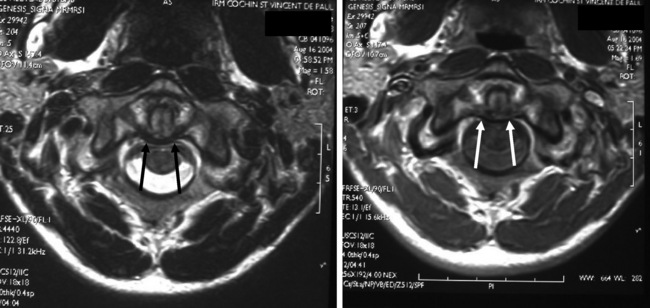
MR imaging is, however, the procedure of choice for evaluating a suspected disc herniation (Figures 2.20, 2.21). In addition to assessing the intervertebral discs, MR imaging allows for evaluation of the spinal cord to rule out other causes of neurologic compromise, such as cord tumour or syrinx (see Chapter 3).
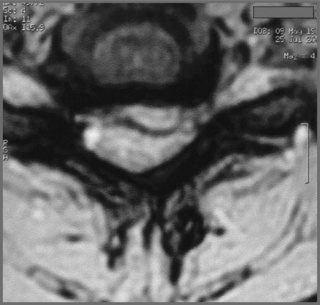
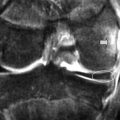
Figure 2.21 • MR imaging of the cervical spine at C4/5. This axial T2-weighted image demonstrates a large focal disc lesion, a sizeable disc extrusion occupying the central, predominantly left paracentral and left foraminal zones. This is the same patient as in Figure 2.20.
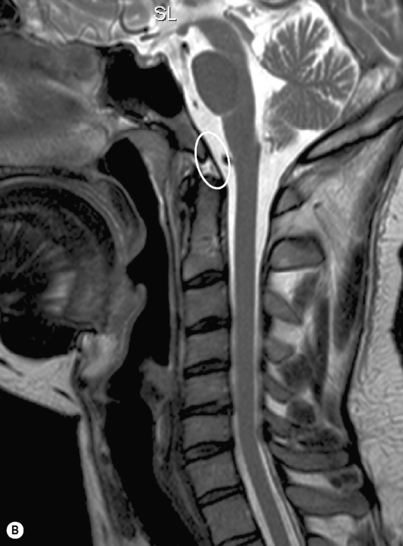
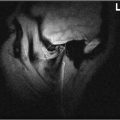
Myelomalacia of the cord, secondary to compromise, is also evident on MR images and will appear as high signal intensity on the T2-weighted sequences at the site of compression on both sagittal and axial slices. On T1-weighted imaging, the same zone will be seen as thinner and lower in signal compared to normal. The cause of the myelomalacia can be noted directly using dynamic MR imaging where, particularly on extension, buckling of the ligamentum flavum, the joint capsule and degenerative changes can be seen to indent or contact the dural sac and contents directly (Figure 2.22).
On MR imaging, the disc herniation will appear as a lesion, most commonly in the ventral aspect of the spinal canal. It is important to determine whether the herniation is contacting, displacing, or compressing the dural sac, as the nature of the neural compromise will inform treatment; the relationship of the herniation to the dural sac and contents is best evaluated on axial images. It is also necessary to evaluate the disc lesion with respect to the take-off sites of the ventral nerve root and its passage through the intervertebral foramen, either of which may result in discoradicular conflict. On T1-weighted images, the disc herniation will most often have signal characteristics that are isointense to the disc and the herniation will appear continuous with the disc. T2-weighted signals will vary depending upon the relative hydration of the disc. Typically, herniations do not enhance following the administration of contrast, though peripheral granulation tissue surrounding the herniation will show enhancement. This principle has important ramifications in patients with recurrent pain after surgery: scarring versus recurrent disc herniation is a common diagnostic dilemma as the signal intensity may be heterogeneous corresponding to a mixture of discal and haemorrhagic components. Gadolinium may also help in the detection of annular tears.35
Degenerative disease
Degenerative disc and joint disease in the cervical spine is a common condition with a multifactorial aetiology. Factors such as repetitive stress, familial predisposition, cigarette smoking, obesity, and diet can all contribute to degenerative joint disease.32,36 In the cervical spine, degenerative changes can occur at the intervertebral disc and adjacent vertebral body endplates, the facet joints, and the uncovertebral joints. Degenerative changes in each of these locations can contribute to central canal or IVF stenosis, resulting in symptoms of central or peripheral neurologic compromise.
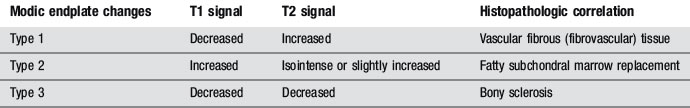
In addition to demonstrating the changes within the degenerative intervertebral disc, MR imaging is sensitive to physiological changes in the adjacent vertebral body endplates. Modic described three distinct types of endplate changes in the lumbar spine: these may also be applied to the cervical spine, although less evidence has been produced to discuss this (Table 2.02).37 The earliest change in the subchondral endplates is the replacement of normal marrow with fibrovascular marrow. This type 1 endplate change appears on T1-weighted images as hypointense to surrounding marrow. On T2-weighting, type 1 Modic changes appear hyperintense to marrow.
The type 3 changes can also be visualized on radiographs as subchondral sclerosis. In addition to endplate changes, the altered biomechanics produced by diminished disc height may result in anterior or posterior osteophytic formation from the vertebral body margins. The combination of decreased disc height and spondylophytes (osteophytes) may produce central canal stenosis. This will appear on T2-weighted images as a loss of CSF signal around the cord at the level of the intervertebral disc. T2-weighted images are also useful to evaluate for high signal within the cord, which would indicate myelomalacia.32
Inflammatory arthropathies
Inflammatory arthropathies share a common pathological feature of degradation of the synovial lining of affected joints. The synovial lining is replaced by vascular granulation tissue, called pannus, which progressively fills the joint. The pannus erodes adjacent articular cartilage, bone, and ligaments. Once the joint is filled with pannus, it becomes fibrous, and the joint may eventually fuse.38
MR imaging is useful to assess the relationship of C1 and C2 to the spinal cord and also allows visualization of the pannus, which may in itself be a cause of cord compression. On MR imaging, the pannus appears as low signal intensity on T1-weighted images. On T2-weighted images, pannus has a heterogeneous appearance, with areas of high and low signal intensity.25 The use of gadolinium contrast causes the pannus to enhance.38
Hydroxyapatite crystal deposition disease (HADD)
HADD, more colloquially known as calcific tendonitis, of the longus colli tendon may present as a sudden onset of neck pain and stiffness in an adult. The aetiology of HADD is not clear, but trauma, repetitive injury, and ischaemia have all been implicated as predisposing factors.39,40 HADD occurs most frequently around the shoulder, but may also affect the cervical spine, where longus colli is most commonly affected; this muscle extends from C1 through T3 and acts as a principal flexor of the cervical spine.41
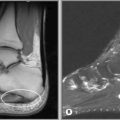
Deposition of hydroxyapatite crystals in the longus colli tendon following trauma results in non-specific neck pain and possibly difficulty swallowing. Though painful, this condition is self-limiting, often resolving in 1 to 2 weeks. Radiographs of the cervical spine will demonstrate a radiopacity in the retropharyngeal interspace, which is homogenous in density.42 Though MR imaging is not necessary to make the diagnosis, this condition may appear on scans obtained to evaluate the cause of the patient’s pain. Advanced imaging is especially useful when trying to exclude the presence of a retropharyngeal abscess or disc space infection. In addition, MR imaging may demonstrate the adjacent bone marrow oedema that may accompany the HADD of the longus colli, although this phenomenon has been more commonly described affecting the extremities.
On MR imaging, the calcific deposits will appear as low signal on both T1- and T2-weighted images. Adjacent prevertebral soft tissue swelling will appear as high signal intensity on T2-weighting. The presence of normal intervertebral discs and vertebral body marrow helps to rule out infection.39
Calcification of intervertebral discs is a common radiographic finding, typically associated with degenerative disc disease. This is more common in the thoracic and lumbar spine and is typically asymptomatic.35 Disc calcification in children and adolescents behaves differently from that in adults. In young patients, disc calcification is typically associated with neck pain, possibly torticollis in particular.43 It is more common in the cervical and upper thoracic spine, and it is considered as self-limiting in nature.
Cervical spine neoplasms
Aneurysmal bone cyst
Aneurysmal bone cysts are expansile lesions, containing thin-walled, blood-filled cavities. They are, in essence, intra-articular arteriovenous malformations that may occur in any bone, though 30% occur in the spine, where they have a particular affinity for the cervical spine, generally affecting the posterior elements. Patients are typically between the age of 10 and 30 years, with a peak incidence in the second decade; the gender prevalence is unclear.44–46 Symptoms are related to the expansile nature of the lesion and patients may present with neurological signs. Radiographs typically reveal a ‘soap-bubble’, expansile lesion of the posterior elements, similar to other expansile lesions; however, the MRI features of aneurysmal bone cysts are unique. The lobulated posterior arch lesions will often exhibit fluid levels on both T1- and T2-weighted images. The signal intensity will vary, depending upon the stage of breakdown of the blood products. The haemosiderin deposits at the periphery of the lesion will appear as a low signal rim on all sequences. Contrast administration may show enhancement at the periphery of the lesion. MR imaging is also very useful for determining the extent of cord compromise.
Osteoid osteoma and osteoblastoma
Differing only in size, osteoid osteomas and osteoblastomas are pathologically related benign tumours of bone. These lesions should be considered in the differential diagnosis of young patients who present with a painful scoliosis. Osteoid osteomas measure less than 1.5 cm in diameter and may incite extensive reactive sclerosis in the surrounding bone.47 Osteoid osteomas occur most often in patients 10 to 20 years of age, with osteoblastomas occurring in a slightly older population. In addition to affecting the long bones, such as the femur, approximately 10% of osteoid osteomas occur in the spine.48
On MR imaging, osteoid osteomas can be difficult to see, as the nidus is small and can lie between sequential slices. The tumour nidus is isointense to muscle on T1-weighted images and remains low signal on T2-weighted images. The surrounding oedema appears hyperintense to bone on T2-weighted images and both the nidus and the surrounding oedema will enhance with contrast.47
Osteoblastomas are giant osteoid osteomas and are given this designation if the lesion measures over 1.5 cm in size. They occur in patients under 30 years of age, with a peak incidence slightly greater than that of osteoid osteomas.47,48 Approximately one-third occur in the spine and one-third of those affect the cervical spine. Like osteoid osteomas, these lesions involve the posterior elements, though they may extend into the vertebral body. Because of their expansile nature, these lesions are more likely to produce neurologic symptoms than are osteoid osteomas.48 The symptomatic picture of night pain, relieved by salicylates, is also similar to osteoid osteomas although typically less intense.
Metastatic disease
Osseous metastasis is the most common malignancy of bone. Up to 40% of patients with non-osseous primary malignancies will develop metastasis to their viscera or bones. When metastatic disease involves the skeletal system, the vertebral column is most often affected. The thoracic spine is most often involved, followed by the lumbar and then cervical spine. Prostate, lung, and breast carcinoma represent the source of most spinal metastases. The most common mechanism of extension to the axial skeleton is through haematogenous spread; tumour cells seed to the vertebral bodies via Batson’s vertebral plexus.32
Patients with metastatic disease to their spine will typically present with unrelenting back pain without substantial objective findings. Radiographs may appear normal or reveal osteoblastic or lytic changes in the vertebral bodies. On MR images, lesions will appear as low signal on T1-weighted images and high signal on T2-weighted images. Contrast-enhanced images should be obtained using fat suppression techniques to avoid masking the inconsistently enhancing lesions.32 The differential diagnosis for multiple lesions in cancellous bone includes marrow disorders such as multiple myeloma, lymphoma, and leukaemia.
Disc space infection
Infection of the disc space is a serious, potentially life-threatening, condition that requires early detection and prompt treatment for the most favourable outcome. Approximately 2–4% of osteomyelitis affects the spine, with the cervical spine least commonly involved.49–51 The three mechanisms of spread are implantation through surgery or trauma, direct spread from an adjacent focus of infection, or haematogenous spread. Bloodborne pathogens arrive in the vertebral body through Batson’s venous plexus (retrograde flow) or the vertebral body arterioles.52
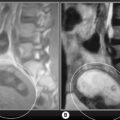
The infection starts in the anterior aspect of the vertebral body and spreads through the disc to the adjacent level. Patients with disc space infection are likely to present with back pain of insidious onset. The pain will appear non-mechanical, constant, and unaffected by rest.50 Additional constitutional symptoms such as fever, chills and weight loss may be present but are not necessary for the diagnosis. Laboratory evaluation may reveal elevated white blood cells, erythrocyte sedimentation rate, and C-reactive protein. Radiographic findings of early disc space infection are subtle and may consist only of disc space narrowing and subtle endplate irregularity.49 MR imaging is the imaging procedure of choice for the evaluation of suspected infection and clinical suspicion should prompt an immediate referral (Figure 2.23). Findings will include decreased marrow signal on T1-weighting and increased signal on T2-weighting in adjacent vertebral bodies and the intervening disc.49 MR imaging may also demonstrate endplate destruction in more advanced cases of infection. Administration of contrast will demonstrate enhancement of infected tissues.49 One of the biggest mimickers of disc space infection, and one that causes anxiety amongst clinicians on MR imaging, is the findings seen with Modic degenerative endplate changes.50 With Modic type 1 changes, there is increased marrow signal on T2-weighted images secondary to replacement of normal bone marrow by fibrovascular tissue. The presence of increased T2 signal within the disc in disc space infection is an important diagnostic clue that helps to distinguish between infection and degenerative disc disease, which produces a reduction in the disc signal on T2-weighted images.
Cervical spine trauma
Neck pain following cervical trauma is a common presenting complaint in primary care. A thorough history and physical examination, including neurological assessment, is crucial in arriving at a diagnosis and in guiding appropriate treatment or follow-up. Injury patterns vary depending upon the mechanism of injury and understanding the direction of force is helpful in narrowing the differential diagnosis (Table 2.03).53
| Axial compression |
The initial imaging work-up following cervical spine trauma typically consists of a three-view radiographic series. Often, flexion and extension views are also obtained, though in the acute setting the usefulness of these images to detect instability may be limited if the patient has a decreased ability to perform range of motion.54 In the evaluation of static or flexion/extension radiographs, the presence of more than 3.5 mm of motion at one level, compared to adjacent levels, constitutes instability and warrants a referral for neurosurgical evaluation.12
In an acute, post-traumatic situation, CT may be obtained to assess the spine for fracture. CT gives greater detail than MR imaging regarding the amount of cortical offset and is better in detecting displacement of small fragments. MR imaging is superior, however, for evaluating soft tissue injuries and for evaluating the spinal cord, intervertebral discs, and ligamentous structures.55 MR imaging is also highly sensitive for detecting fractures, and, in a patient with neurologic impairment following trauma, MR imaging is the imaging procedure of choice.
Cervical injuries are often occult on plain film and clinical suspicion should drive imaging decisions. On MR imaging, the oedema produced by fracture or ligamentous injury will appear as low signal on T1-weighted images and high signal on T2-weighted images. Injuries to the spinal cord can occur in the absence of fracture or dislocation and will also be best evaluated on MR imaging. During extension injuries, the ligamentum flavum buckles into the canal, reducing its cross-sectional diameter. In the presence of pre-existing degenerative disease, a physiologically narrow canal or momentary subluxation at the time of injury, the cord may be contused.53 The cord contusion will appear as a high signal focus within the cord on T2-weighted images. The advent of seated MR imaging allows patients to be imaged in a weight-bearing posture and in a position that recreates their pain. Patients can also be imaged in flexion and extension positions to evaluate stability. Upright imaging may reveal disc herniations and antero- or retro-listheses not present on recumbent studies; this may help inform prognosis and guide treatment decisions.56
1 Cote P., Cassidy D.J., Carroll L.J., Kristman V. The annual incidence and course of neck pain in the general population: a population-based cohort study. Pain. 2004;112:267-273.
2 Makela M., Heliovaara M., Sievers K., et al. Prevalence, determinants, and consequences of chronic neck pain in Finland. Am J Epidemiol. 1991;134(11):1356-1367.
3 Christensen M.G., Kollasch M.W. Job Analysis of Chiropractic 2005: A Project Report, Survey Analysis, and Summary of the Practice of Chiropractic within the United States. Greeley, CO: National Board of Chiropractic Examiners, 2005.
4 Bussieres A.E., Taylor J.A.M., Peterson C. Diagnostic imaging practice guidelines for musculoskeletal complaints in adults—an evidence-based approach—Part 3: Spinal disorders. J Manipulative Physiol Ther. 2008;31(1):33-88.
5 Berkow R. Neck, shoulder and upper limb pain. In Merck Manual of Diagnosis and Therapy, 16th ed, West Point, PA: Merck & Co; 1992:1362.
6 Bates B. The musculoskeletal system. In: Bates B., editor. A Guide to Physical Examination. 3rd ed. Philadelphia: JB Lippincott; 1983:324-370.
7 Lindsay K., Bone I., Callander R. Localised neurological disease and its management. Neurology and Neurosurgery Illustrated. Edinburgh: Elsevier, 1991.
8 Demirbag D., Unlu E., Ozdemir F., et al. The relationship between magnetic resonance imaging findings and postural maneuver and physical examination tests in patients with thoracic outlet syndrome: results of a double-blind, controlled study. Arch Phys Med Rehabil. 2007;88(7):844-851.
9 Wessely M., Grenier J.M. Elbow MRI. Part 2: The imaging of common disorders affecting the elbow region. Clinical Chiropractic. 2007;10(1):43-49.
10 Wessely M., Grenier J.-M. MR imaging of the wrist and hand—a review of the normal imaging appearance with an illustration of common disorders affecting the wrist and hand. Clinical Chiropractic. 2007;10(3):156-164.
11 Travell J., Simons D. Myofascial Pain and Dysfunction. Baltimore: Williams and Wilkins, 1992.
12 White A., Johnson R., Panjabi M., Southwick W. Biomechanical analysis of clinical stability in the cervical spine. Clin Orthop Rel Res. 1975;109:85-96.
13 Helms C. Trauma. In: Fundamentals of Skeletal Radiology. Philadelphia: Elsevier Saunders; 2005:78-112.
14 Helms C., Major N., Anderson M.W., et al. Basic principles of musculoskeletal MRI. In Musculoskeletal MRI, 2nd ed, Philadelphia PA: Elsevier Saunders; 2009:1-19.
15 Moore K. The back. In Clinically Oriented Anatomy, 2nd ed, Baltimore: Williams and Wilkins; 1985:565-625.
16 Green J., Silver P. The vertebral column and the back. In: An Introduction to Human Anatomy. Oxford: Oxford University Press; 1981:52-68.
17 Standring S., editor. Gray’s Anatomy – The back (Section 45). Edinburgh: Elsevier, 2009.
18 Rowe L., Yochum T. Radiograpic positioning and normal anatomy. In: Yochum T., Rowe L., editors. Essentials of Skeletal Radiology. Baltimore: Williams and Wilkins; 1987:1-93.
19 Standring S., editor. Gray’s Anatomy – Neuroanatomy: vascular supply of the brain (Section 17). Edinburgh: Elsevier, 2009.
20 Green J., Silver P. The blood supply to the head and neck. In: An Introduction to Human Anatomy. Oxford: Oxford University Press; 1981:253-267.
21 Steel H.H. Anatomical and mechanical considerations of the atlanto-axial articulations. J Bone Joint Surg Am. 1968;50:1481-1482.
22 Ulbrich E., Schraner C., Busato A., et al. Cervical spinal canal dimensions. In: 16th Annual Congress of the European Society of Musculoskeletal Radiology. Italy: Genoa; June 11–13, 2009.
23 Clark C. The Cervical Spine, 3rd ed. Philadelphia: Lippincott-Raven, 1998.
24 Cramer G.D., Darby S.A. Basic and Clinical Anatomy of the Spine, Spinal Cord, and ANS, 2nd ed. St. Louis: Mosby, 2005.
25 Kaplan P., Helms C.A., Dussault R., et al. Musculoskeletal MRI. Philadelphia: WB Saunders, 2001.
26 White M. Cervical spine: MR imaging techniques and anatomy. Magn Reson Imaging Clin N Am. 2000;8(3):453-469.
27 Teo E., Ng H. Evaluation of the role of ligaments, facets and disc nucleus in lower cervical spine under compression and sagittal moments using finite element method. Med Eng Phys. 2001;23:155-164.
28 Swinkels A., Dolan P. Spinal position sense is independent of the magnitude of movement. Spine. 2000;25(1):98-105.
29 Kaale B.R., Krakenes J., Albrektsen G., Wester K. Head position and impact direction in whiplash injuries: associations with MRI-verified lesions of ligaments and membranes in the upper cervical spine. J Neurotrauma. 2005;22(11):1294-1302.
30 Kaale B.R., Krakenes J., Albrektsen G., Wester K. Whiplash-associated disorders impairment rating: neck disability index score according to severity of MRI findings of ligaments and membranes in the upper cervical spine. J Neurotrauma. 2005;22(4):466-475.
31 Kaale B.R., Krakenes J., Albrektsen G., Wester K. Clinical assessment techniques for detecting ligament and membrane injuries in the upper cervical spine region—a comparison with MRI results. Man Ther. 2008;13(5):397-403.
32 Ross J.S., Brant-Zawadzki M., Chen M.Z. Diagnostic Imaging: Spine. Salt Lake City: Amirsys, 2007.
33 Braga-Baiak A., Shah A., Pietrobon R., et al. Intra- and inter-observer reliability of MRI examination of intervertebral disc abnormalities in patients with cervical myelopathy. Eur J Radiol. 2008;65:91-98.
34 Fardon D.F., Milette P.C. Nomenclature and classification of lumbar disc pathology. Spine. 2001;26(5):E93-E113.
35 Boutin R., Steinbach L., Finnesey K. MR imaging of degenerative diseases in the cervical spine. Magn Reson Imaging Clin N Am. 2000;8(3):471-490.
36 Sangha O. Epidemiology of rheumatic diseases. Rheumatology. 2000;39(suppl 2):3-12.
37 Modic M., Steinberg P., Ross J., et al. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166:193-199.
38 Imhof H., Nobauer-Huhmann I.-M., Gahleitner A., et al. Pathophysiology and imaging in inflammatory and blastomatous synovial diseases. Skeletal Radiol. 2002;31:313-333.
39 Feydy A., Liote F., Carlier R., et al. Cervical spine and crystal-associated diseases: imaging findings. Eur Radiol. 2006;16:459-468.
40 Hayes C., Conway W. Calcium hydroxyapatite deposition disease. Radiographics. 1990;10:1031-1048.
41 Chung T., Rebello R., Gooden E. Retropharyngeal calcific tendonitis: case report and review of the literature. Emerg Radiol. 2005;11:375-380.
42 Hviid C., Salomonsen M., Gelineck J., et al. Retropharyngeal tendinitis may be more common than we think: a report on 45 cases seen in Danish chiropractic clinics. J Manipulative Physiol Ther. 2009;32(4):315-320.
43 Donmez H., Mavili E., Ikizceli T., Koc R.K. Pediatric intervertebral disc calcification. Diagn Interv Radiol. 2008;14(4):225-227.
44 Zehetgruber H., Bittner B., Guber D., et al. Prevalence of aneurysmal and solitary bone cysts in young patients. Clin Orthop Rel Res. 2005;439:136-143.
45 Leithner A., Windhager R., Lang S., et al. Aneurysmal bone cyst: a population based epidemiologic study and literature review. Clin Orthop Rel Res. 1999;363:176-179.
46 Pennekamp W., Peters S., Schinkel C., et al. Aneurysmal bone cyst of the cervical spine (2008:7b). Eur Radiol. 2008;18(10):2356-2360.
47 Ozaki T., Liljenqvist U., Hillmann A., et al. Osteoid osteoma and osteoblastoma of the spine: experiences with 22 patients. Clin Orthop Rel Res. 2002;397:394-402.
48 Pettine K., KIassen R. Osteoid-osteoma and osteoblastoma of the spine. J Bone Joint Surg Am. 1986;68:354-361.
49 Maiuri F.I., Iaconetta G., Gallicchio B., et al. Spondylodiscitis: clinical and magnetic resonance diagnosis. Spine. 1997;22(15):1741-1746.
50 Hong S.H., Choi J.-Y., Lee J.W., et al. MRI imaging assessment of the spine: infection or an imitation. Radiographics. 2009;29(2):599-611.
51 Tins B.J., Cassar-Pullicino V.N., Lalam R.K. Magnetic resonance imaging of spinal infection. Top Magn Reson Imaging. 2007;18(3):213-222.
52 Dagirmanjiian A., Schils J., McHenry M. MR imaging of spinal infections. Magn Reson Imaging Clin N Am. 1999;7:525-538.
53 Cusick J.F., Yoganandan N. Biomechanics of the cervical spine 4: major injuries. Clin Biomech. 2002;17:1-20.
54 Insko E.K., Gracias V.H., Gupta R., et al. Utility of flexion and extension radiographs of the cervical spine in the acute evaluation of blunt trauma. J Trauma. 2002;53(3):426-429.
55 Wenger M., Adam P., Alareon F., Markwalder T.-M. Traumatic cervical instability associated with cord oedema and temporary quadriparesis. Spinal Cord. 2003;41:521-526.
56 Perez A.F., Isidro M.G., Ayerbe E., et al. Evaluation of intervertebral disc herniation and hypermobile intersegmental instability in symptomatic adult patients undergoing recumbent and upright MRI of the cervical or lumbosacral spines. Eur J Radiol. 2007;62(3):444-448.