7 The ankle and foot
Introduction
It is also necessary to appreciate the importance of accurate diagnosis and prompt treatment of conditions in this area; disorders affecting this region, such as Morton’s neuroma or intermetatarsal bursitis, can have a far-reaching effect on the patient due to the disruption of lower kinematic chain mechanics.1,2 Although orthopaedic testing can provide some information as to the range of diagnostic possibilities, further imaging, particularly MR imaging, can often prove key in identifying the pain-producing structure. Although ultrasonography is being increasingly utilized, this modality can be very operator-dependent, which makes it less reliable and prone to producing false negative results.3,4
History and examination
Much of what holds true for the knee also applies to the ankle and foot; this should not be surprising as they are directly connected elements in what, in standing posture, is a closed-loop kinematic chain.2 Because of this, the knee, ankle and foot often need to be assessed as a unit and the reader should direct themselves to Chapter 6 in order to review this material.
Differential diagnosis
The foot is susceptible to many conditions; these can mimic each other and exist as comorbidities. Although a thorough history will help to direct the clinician’s thinking, more than any other joint, the ‘V-I-N-D-I-C-A-T-E’ mnemonic will help to avoid the missed diagnosis (Table 7.01).
Table 7.01 Differential diagnostic considerations for the foot and ankle
| Vascular | Diabetes mellitus, thrombophlebitis, Raynaud’s syndrome |
| Infection/Inflammation | Osteomyeltis/gout, Reiter’s syndrome/ plantar fasciitis, bursitis, tendinitis, cellulitis |
| Neoplasm | Primary or secondary cancers |
| Dermatological | Complex regional pain syndrome (Sudek’s atrophy) |
| Iatrogenic | Drug interactions, postsurgical syndromes |
| Congenital | Morton’s toe, talipes |
| Anatomical | Accessory muscles, Morton’s neuroma, calcaneal spur |
| Trauma | Acute or chronic |
| Endocrine/Environmental | Syndromes related to footwear |
Clinical indications for imaging
The clinical indications for MR imaging of the ankle and foot are varied and may also depend on the clinical protocols established by the imaging centre and the availability of resources. Based on current evidence, MR imaging of the ankle and foot is considered the imaging modality of choice for conditions such as internal derangements (for example, impingement syndromes or tarsal tunnel syndrome) that commonly affect the distal lower extremity or for postoperative evaluation.5–7 MR imaging gives the anatomical detail needed to identify both the pathology and the effect on the surrounding structures; this is important to evaluate since it will affect both the clinical management of the patient and their prognosis.
Procedure and sequences
MR imaging of the ankle requires that the patient lies supine with the ankle perpendicular to the lower leg; however, if the course of a particular tendon requires analysis, the position of the ankle may need to be modified in order to avoid technical artifacts such as the magic angle effect (explained in detail in Chapter 8). A support may be used to immobilize the patient and maintain the position during the imaging study.
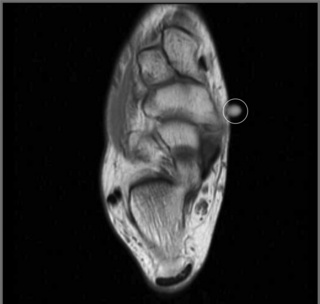
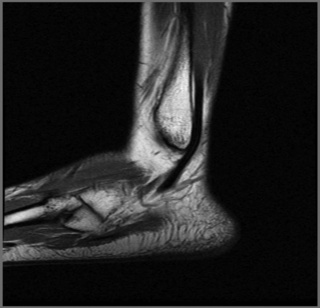
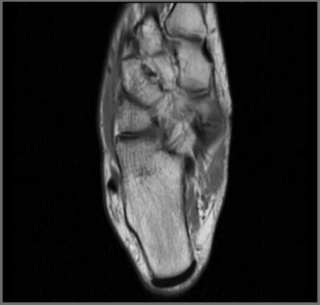
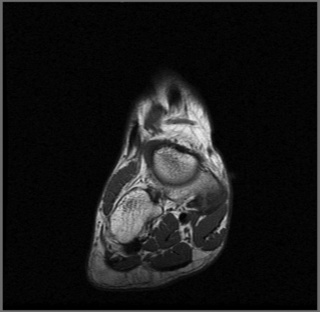
A surface coil is usually used to increase the signal capture; a skin marker may be added to signal to the person reading the image the region of clinical interest (Figure 7.01). The sequences usually consist of all three planes: sagittal (Figures 7.02–7.04), axial (Figures 7.05–7.07) and coronal (Figures 7.08–7.10), using a combination of T1- and T2-weighted (or STIR) sequences, depending on the clinical scenario.
Normal imaging appearance
Tendons
Posterior
The posterior tendons include the Achilles (calcaneal) and plantaris, both of which have associated bursae (Figure 7.11). The Achilles tendon has a broad insertion along the posterior aspect of the calcaneus, which is often irregular in this region due to the development of degenerative changes associated with soliciting the tendon during the activities of daily living. The tendon is best seen on the sagittal and axial cuts. Normally, on the sagittal imaging, it is noted as a long, relatively thick, low signal intensity structure that courses from the intermediate signal of the gastrocnemius muscle to its insertion on the calcaneus. It thickens somewhat just above this insertion; this should not be interpreted as a focal tendinosis. The tendon should be evaluated on both the T1- and T2-weighted images; on both sequences, it should be seen as a low signal intensity structure.
Medial
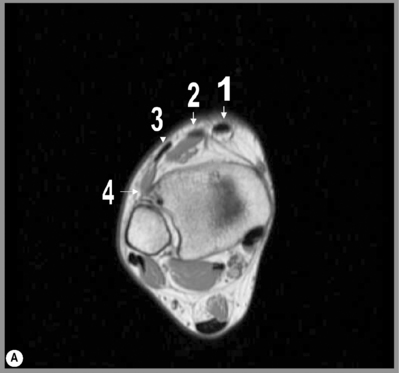
Medially, the flexor tendons descend under the flexor retinaculum; these comprise the tibialis posterior, flexor digitorum longus and flexor hallucis longus (mnemonically referred to as ‘Tom, Dick and Harry’). The tibialis posterior tendon is prone to rupture, though not as frequently as that of the Achilles tendon.8
As the tendon descends to its insertion on the navicular and metatarsals, the shape of the tendon changes on the axial slices from an oval structure to a flatter configuration as it courses past the medial aspect of the talus. As the tendon continues to descend, it divides into smaller bundles as it approaches the navicular and metatarsals.9 The appearance of this normal fibrous division may be confused with a distal tear; however, tears in the insertions of the tendon are rare and the normal appearance can be confirmed by the lack of high-signal oedema on the fluid-sensitive sequences (Figure 7.12).
The flexor digitorum longus tendon runs alongside and superficial to that of the tibialis posterior. It is rarely injured in isolation and is more commonly associated with a generalized regional tendinopathy. The flexor hallucis longus tendon has a rather unusual course that can render it susceptible to injury. As it passes behind the talus, in those patients who have an os trigonum, friction may be created between the tendon and the accessory ossicle; this can lead to symptoms of posterior impingement, including discomfort and pain on plantar flexion and perhaps focal swelling palpable behind the ankle joint. In the same region, the tendon changes its course from being a predominantly vertical to a more horizontal orientation; during this transition, it can be more prone to injury. The tendon of the flexor hallucis longus is well depicted in its proximal course in both the sagittal and axial planes; as it turns to become more horizontal, it is initially well visualized on the axial and then the sagittal/long axis images as it approaches its insertion.10
Lateral
The peroneus longus and brevis tendons are located laterally (Figure 7.13). Both these muscles share the action of eversion and dorsiflexion of the foot.11 As both tendons descend, they are located posterolaterally to the lateral malleolus. As the tendons pass this region, they are stabilized in part by the superior peroneal retinaculum, which, depending on the imaging quality, can be identified. At this level, the tendon of the peroneus longus is seen as a rounded structure in the axial plane; this helps distinguish it from the flatter appearance of the peroneus brevis tendon. As it passes further distally, the peroneus brevis is located anterior to the peroneal tubercle of the calcaneus. Both tendons may be surrounded by a thin layer of fluid on the fluid-sensitive sequences, which is normal. Although there is no formal measurement for the quantification of fluid, more than just a thin layer may be considered as tenosynovitis.
Anterior
The tendons in this region comprise the tibialis anterior, which lies most medially, then the extensor hallucis longus, extensor digitorum longus and peroneus tertius (Figure 7.14).12 The tendons pass inferiorly to the superior and inferior divisions of the extensor retinaculum, which may be identifiable on MR imaging. These structures are only occasionally affected by pathology; of the anterior tendons, the tibialis anterior tendon is most frequently involved. In particular, the tibialis anterior tendon course is straight with limited opportunity to be impinged by surrounding structures, unlike the posterior compartment structures. The appearance of the tendon on axial slices is that of a round or oval structure, which, as it approaches the insertion points on the first metatarsal and medial cuneiform, becomes flatter. The normal thickness of the tendon within 3 cm of these insertion points is that of no more than 5 mm.13 Injuries are usually either of a direct nature, which may occur at any age and which may be associated with fractures of soft tissue lesions, or as a result of degenerative processes, in which case the patient is often 60 to 70 years old with chronic symptoms.14
Ligaments
The ankle and foot ligaments may also be well visualized using MR imaging; this modality is particularly useful in evaluation of complex or refractory ankle sprains or in those patients who solicit their ankles regularly.15 However, for routine ankle sprains, clinical examination alone, augmented if necessary by diagnostic ultrasound, is usually sufficient. The ligaments most frequently involved in clinical syndromes are the medial ligament complex (deltoid ligament) and lateral ligament complex. These ligaments are best evaluated using axial MR images, although the sagittal and coronal planes complement these sequences. Generally, ligaments are thin, low signal intensity structures; their identification is relatively straightforward if their anatomical relations are familiar to the examiner.
The ankle ligaments can be divided in to three regions: the lateral ligamentous complex, which is the most prone to injury; the medial group, consisting of the deltoid complex; and the central syndesmosis, or tibiofibular complex, which is important for retaining the stability of the ankle and which may be injured in high-grade ankle traumas, resulting in instability of the ankle.16 Often, there is a predominant group of ligaments involved with a secondary or tertiary group affected by means of the ‘contre coup’ mechanism, so, as the patient rolls over the ankle into inversion, often, a rapid eversion will occur following this, thereby resulting in lateral and medial involvement. The physical examination and diagnostic imaging should take this into consideration.
Normal variants and developmental anomalies
Osseous variants and paediatric considerations
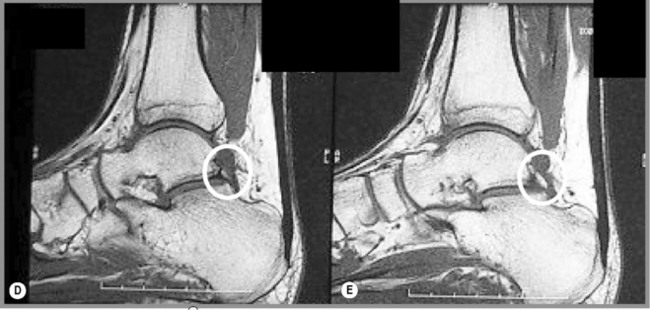
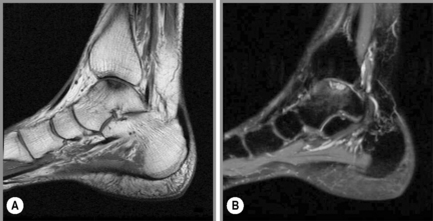
A frequent cause of foot and ankle pain is the development of accessory ossicles. In the ankle, the two most common accessory ossicles are the os trigonum and the accessory navicular (or os tibiale externum) bone (Figure 7.15). An os trigonum will be found immediately posterior to the talus and is not usually palpable; therefore, its existence can only be determined by diagnostic imaging. It arises from the failure to fuse of an accessory ossification centre located just posterior to the lateral talar tubercle ossification centre. Normally, this will occur at around 13 years of age; however, in about 10% of the population it remains separated and forms a separate bone (Figure 7.15). In some patients, a pseudoarticulation with the talus may occur.
Although many patients with an os trigonum will be asymptomatic, some will complain of pain in the posterior aspect of the ankle that is worsened by plantar flexion, thus those who dance, run downhill or play football are particularly affected, although even activities of general daily living may be enough to provoke the development of pain. Pain may develop with onset of the condition or remain dormant until later life when altered regional biomechanics create stress between the bony structure and the surrounding soft tissues, most significantly the adjacent tendon of the flexor hallucis longus muscle; this is termed os trigonum syndrome or posterior impingement syndrome.17,18
In the case of an accessory navicular, the patient may complain of discomfort and pain on the medial side of the midfoot and exhibit swelling in the region. With larger accessory navicular bones, the patient may even remark on the presence of a hard mass on the inside of the midfoot, which may cause pressure on the inside of their shoes. On radiographs, a prominent or accessory navicular may be demonstrated just medial to the parent navicular bone. Although an accessory navicular is considered by some to be a post-traumatic lesion – an avulsive fracture of the cartilaginous growth plate – the fact that it is so frequently found bilaterally suggests otherwise.19
With MR imaging, the relationship of the accessory bone with the surrounding soft tissue structures can again be appreciated to a fuller extent; in particular, the posterior tibialis tendon is particularly vulnerable to tears in the presence of an accessory navicular. Other pathologies that may arise include the development of a painful bursa, or the development of bone marrow oedema in either the accessory navicular or parent navicular bone.20
Pathological conditions
Osseous conditions
Trauma
Trauma to the ankle and foot constitutes a major proportion of injuries to the musculoskeletal system as a whole; which of us has not, at some time, turned our ankle or stubbed our toe, even if the consequences are usually no more than a few days’ discomfort? Although radiography is useful in identifying the basic injury in many cases, further imaging may be necessary if symptoms persist or complications develop or, in the case of an athlete, to determine exactly the degree of injury sustained.14 MR imaging is ideal to assess such injuries, being able to determine the osseous and soft tissue relationships, aiding in the development of clinical management strategies and in establishing the patient’s prognosis.
Acute trauma
Acute trauma represents a common presenting complaint, such as that relating to a sporting activity whereby an acute twisting injury results in impaction between the osseous structures (particularly of the ankle) and tears of the soft tissue structures surrounding the region. In such cases, regions of high signal intensity within the osseous structures may be detected soon after the injury; this represents bone marrow oedema. The pattern of this oedema may assist in determining the direction of injury and therefore help to identify the associated soft tissue structures that may be implicated.14
A common complication of such an injury is fragmentation of a piece of articular cartilage, which may be attached to the underlying bone, forming a chondral or osteochondral defect respectively. The talar dome is a particularly common site for such injuries to occur. In addition to a history of recent ankle trauma, the patient may also report a sensation of the articulation being ‘blocked’ during normal activity or, at times, sudden immobility or ‘locking’ following simple movement. The patient may also notice that the joint becomes intermittently swollen; the physical examination will often confirm this through visual observation or a related reduction in the joint’s range of motion.21,22
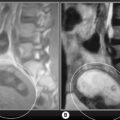
Whilst routine radiography is often used in the first instance to assess the osseous and articular aspects of the ankle, avascular necrosis in its early stages is usually negative on these studies. MR imaging allows identification of such injuries at a much earlier stage and can give much more detail regarding the level of the articular cartilage damage, the extent of displacement of the fragment and the viability of the donor site. Osteochondral defects are particularly well demonstrated using MR imaging and intra-articular contrast is not normally required (Figure 7.17).15
This makes the acquisition of images non-invasive, as compared with computed tomography (CT), wherein iodinated contrast is normally necessary to evaluate the articular cartilage, carrying a risk of complications and potential discomfort for a patient who is already in pain. MR imaging is also superior in providing an overall view of the articulation, identifying other factors that may affect the clinical management of the patient, such as bone marrow oedema or injury to surrounding soft tissue structures.23
If there is less than 10 mm of fragment displacement and no rotation of the fragment with respect to the donor site, treatment may simply involve partial or complete immobilization; however, surgery may be required to return the fragment to the donor site if there is significant displacement or an awkward positioning of the fragment. If there is an associated chondral injury (for example fibrillation), grafting, autologous or otherwise, may be considered.24,25
On MR imaging, the view that is particularly useful in determining the presence of an intra-articular fragment and assessing cartilage damage is the STIR or T2-weighted coronal images; the sagittal and axial images will provide the dimensions of the donor site and, therefore, the extent of the lesion. MR imaging can also provide further information regarding associated injuries. These lesions are often associated with ankle sprains; consequently, a careful evaluation of the ligaments about the ankle is an important part of the evaluation routine.17,26
Chronic trauma
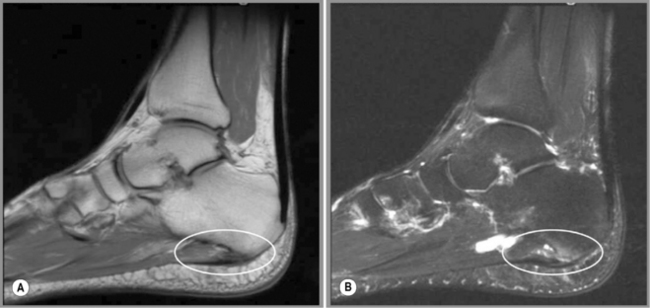
Chronic trauma may also be well visualized on MR imaging and may result from repeated injuries such as those sustained in consecutive ankle sprains, or be related to abnormal biomechanics. This may be intrinsic (congenital, developmental or acquired) or extrinsic, for example from ill-fitting footwear (Figure 7.18).
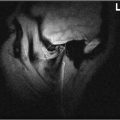
An example of a clinical syndrome related to inappropriate shoes is Haglund’s syndrome (or deformity), whereby wearing high heels or poorly fitting ‘basketball shoes’ causes chronic irritation to the posterior aspect of the ankle. The patient, often a woman, will complain of pain and swelling around the posterosuperior aspect of the calcaneus and demonstrate a noticeable lump in the same region. The condition is often complicated by retrocalcaneal bursitis, retro-Achilles bursitis and thickening of the distal Achilles tendon (Figure 7.19).27,28
Although a number of treatment options are available, first and foremost to correct the precipitating cause, surgery is often required to modify the surrounding bony structures and to reduce the thickening of the tendon. Similar effects may occur in the other bones of the ankle and of the foot, either due to poor-fitting footwear or in those who place a high demand on their feet, such as long-distance runners.29,30
Such patients are also at risk of developing stress fractures, which usually present with diffuse pain that is difficult to localize. Eventually, particularly if the precipitating activity is not curtailed, the pain will focus over the affected region, most commonly the diaphysis of the second or third metatarsal. Although routine radiography may demonstrate a local periosteal response and a bone scan may demonstrate focal increased uptake corresponding to a local increase in bone metabolic activity, the MR images will be able to grade the stress fracture from a simple local periostitis to a complete, though often radiographically subtle, fracture.3
Avascular necrosis
Both the foot and ankle can be affected by avascular necrosis, although the condition has a predilection for the head of the second or third metatarsal and for the talus. In the foot, the major predisposing factor appears to be increased biomechanical stress, often associated with footwear; in particular, high heels. By contrast, the condition when seen in the ankle, usually follows specific, identifiable trauma.31
Routine radiography can demonstrate the classic changes of avascular necrosis: increased density in the subarticular region, subchondral fracture and, eventually, articular surface collapse; however, MR imaging will show these findings at a significantly earlier stage. It can also be used to detect any associated bone marrow oedema, which may perpetuate the patient’s symptoms, and evaluate the local structures for any associated injury. MR imaging will normally demonstrate avascular necrosis of the heads of the metatarsals as a high signal on the fluid-sensitive sequences in all planes, with focal low signal intensity just under the head of the metatarsal involved.32,33
Ligaments
Radiographs are useful in identifying coalition, which tends to occur between the calcaneus and navicular or calcaneus and talus. Although MR imaging is not necessarily systematically used in those patients with coalition, if the patient has a clinical history of repeated ankle sprains and pain or limitation of activity, MR imaging can be useful to determine the presence of a fibrous synchondrosis, and associated bone marrow oedema that may accompany this, as well as for the evaluation of the effects of the coalition, in determining the most appropriate management of the patient.34,35
In cases of a partial or complete rupture, this ligament is most easily assessed using the axial images. By placing the patient’s foot in slight dorsiflexion, the whole ligament will be included in a single slice, making the interpretation easier. If this is not possible, it is important to trace the ligament in its entirety as it courses obliquely from its origin on the medial aspect of the lateral malleolus to its insertion on the lateral aspect of the talus. If this ligament is torn, either partial or complete disruption of the fibres will be noted on MR images; in addition, on the fluid-sensitive sequences, the high-signal synovial fluid will be seen tracking out anterior to the normal position of the ligament, indicating that the synovial capsule has been broached.34,35
Although the PTIF ligament is rarely injured in isolation, when damaged, as may be the case following a severe trauma to the ankle, which may be accompanied by fractures affecting the ankle complex, loss of the normally well-defined low signal intensity linear ligament as well as noting surrounding high signal owing to the leakage of the synovial fluid is useful to determine injury.10,36
Both the Lisfranc and Chopart ligaments may be involved in disruption following a direct or indirect trauma and may be associated with fracture/dislocations of the articulations contributing to the region in question. This is the case particularly with patients affected by diabetes where the Lisfranc fracture/dislocation injury may occur, causing either an adduction or abduction injury as well as dorsal subluxation of the base of the second metatarsal.37,38
Tendons
Tears of the tendons about the ankle and foot may also be evaluated well with MR imaging, especially when associated bony injuries and additional soft tissue structures need to be evaluated. If small foci of high signal are noted within tendons on T2-weighted images, a diagnosis of tendinosis should be considered. This appearance is caused by small micro-tears in the tendon, arising from degenerative changes or overuse. Partial or complete ruptures of the tendon may also occur; however, owing to the relative ease of clinical differentiation and the importance of rapid surgical intervention, MR imaging is not routinely performed. In cases where the diagnosis is unclear, where the presence of a partial, high-grade rupture is being considered, MR imaging will demonstrate the tendon as being irregular and frayed, with small or moderate regions of high signal on the T2-weighted sequence.5
In the Achilles tendon, which is particularly prone to rupture, these regions are usually found 4–6 cm proximal to the insertion of the tendon into the calcaneus, thought to be a less vascular region, thus rendering the tendon more susceptible to injury (Figure 7.20). They need to be differentiated from the small regions of slightly brighter signal arising from the internal architecture of the tendons, which are seen on both the T1- and T2-weighted sequences rather than the fluid-sensitive sequences alone.
As the descending tendon passes the navicular, normal variants may occur; these may, on occasion, cause irritation and tendinopathy. Such normal variants can include a large accessory navicular bone, located medial to the parent navicular. In certain populations, such as dancers and athletes, such large accessory navicular bones can produce a friction effect with the posterior tibialis tendon and also create irritation, and an inflammatory reaction with the parent bone via the partially formed synchondrosis.39,40
The posterior tibial artery, nerve and vein are located between flexor digitorum longus and flexor hallucis longus (Figure 7.12). Occasionally, vascular lesions such as varices can be detected on MR imaging, usually after the clinical examination. MR imaging would not be the imaging modality of choice to detect the varicosities, being detectable following the clinical examination with ultrasound; however, on occasion, large tortuous varicosities may irritate surrounding soft tissue structures such as the tendons and ligaments about the ankle, leading to the development of symptoms of pain, swelling and limitation of movement about the ankle joint.
The peronei can also develop tendinoses: the peroneus longus tendon is more prone to tendinopathy; the peroneus brevis tendon is more prone to acute tears, either partial or complete. Such tears may be associated with bony lesions, such as the Dancer’s or Jones’ fracture, an avulsion fracture located at the styloid process of the base of the fifth metatarsal. With such an injury, the patient will normally have focal pain, swelling and a sense of lack of stability about the lateral aspect of the midfoot (it is important to determine whether this sensation is from the ankle or, as in this case, more distally located).31,41
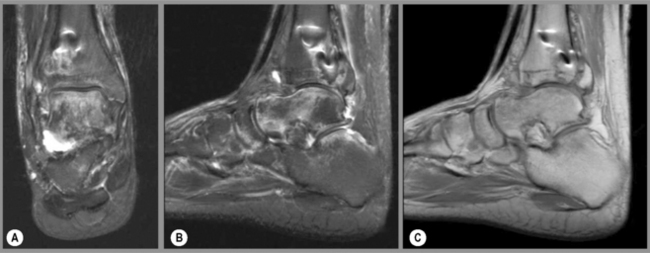
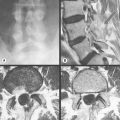
Infection
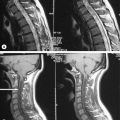
In predisposed populations, such as those with diabetes mellitus, infection of the distal lower extremity is relatively common and carries with it high morbidity and mortality; therefore, astute diagnosis and management of the patient is essential. Despite other techniques being available for the detection of infection, MR imaging remains the most cost-effective and accurate examination modality in differentiating osteomyelitis from soft tissue infection and visualizing associated complications such as abscess formation (Figure 7.21).5
On routine imaging, osteomyelitis may not become visible for up to 10 days post-implantation, the radiographic latent period. However, it is clearly important to make the diagnosis as early as possible to instigate the appropriate management protocols, namely antibiotics and control of associated comorbidity; therefore, where clinical suspicion exists, further imaging is appropriate. This may involve a bone scan but, to best determine the presence of osteomyelitis and the effect that it has on the surrounding osseous and soft tissue architecture, MR imaging is the modality of choice, using a normal series with, if possible, the addition of gadolinium to detect subtle foci of active infection that may otherwise remain occult.42
Within the bone marrow, osteomyelitis will provoke a high signal intensity on the fluid-sensitive sequences; by contrast, the signal on the T1-weighted sequences will appear as hypointense compared to the normal marrow. Regions of osseous destruction will be well defined on these images. Any involvement of the surrounding soft tissue can also be demonstrated well with MR imaging: the development of a periperiosteal inflammatory response, abscess formation and eventually sinus tract development can all be evaluated, as can the response to medical management. Where surgical debridement has been employed, the results can be monitored non-invasively to confirm resolution of the osteomyelitis and the development of possible complications. This is particularly useful for patients such as diabetics, who may need to be evaluated over many years, and allows comparisons to be made with previous studies, which helps to determine subtle changes suggestive of new infective foci.43,44
Morton’s neuroma
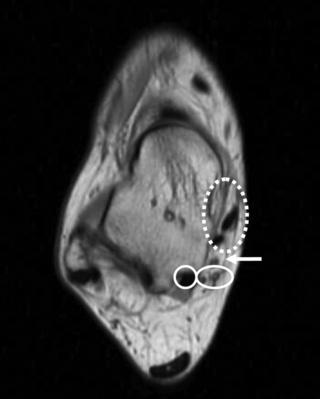
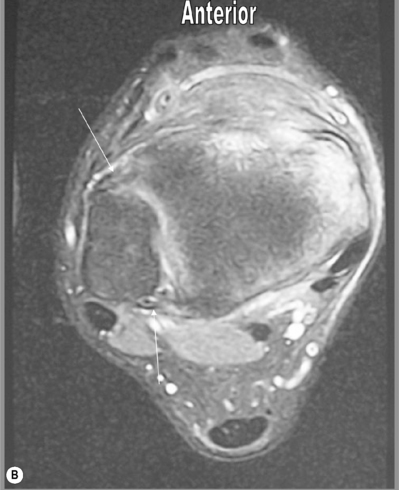
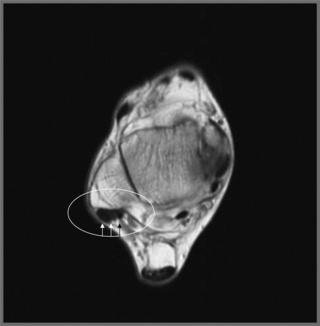
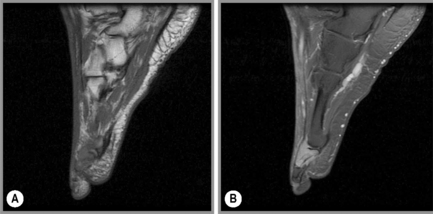
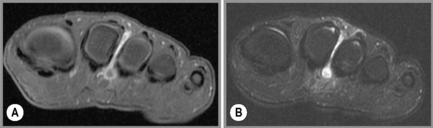
Most commonly occurring in between the third and fourth rays, Morton’s neuroma is an enlargement of a nerve, usually at the point where the lateral plantar nerve combines with part of the medial plantar nerve. The nerve lies in subcutaneous tissue, just above the fat pad of the foot, close to an artery and vein and superficial to the deep transverse metatarsal ligament.9,16 In patients predisposed by pes planus or by unsuitable footwear, the nerve is compressed between the contact point of a shoe and the strong, relatively inflexible ligament.42,45
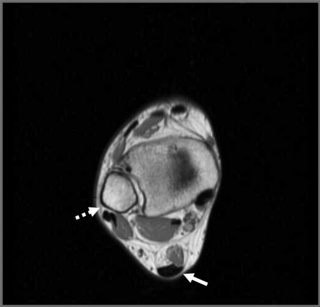
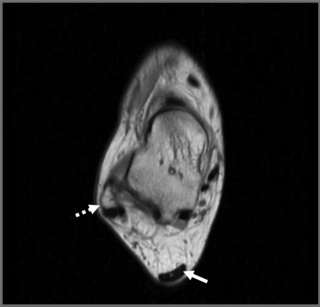
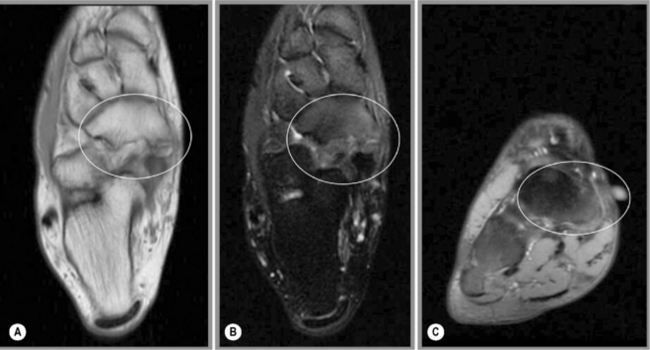
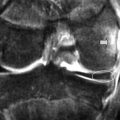
The condition, which is not a true neuroma and is more accurately termed Morton’s metatarsalgia, needs to be differentiated from intermetatarsal bursitis (Figure 7.22). It can be extremely disabling, not just causing local, sometimes exquisite, pain but also altering lower limb biomechanics, limiting the choice of footwear and activities of daily living, such as shopping. Often, the patients are middle-aged women who have progressively developed pain in the second and third metatarsal spaces, either unilaterally or, at times, bilaterally.46
Although observation of the region does not usually reveal a great deal, palpation will often recreate the exquisite pain associated with the conditions. The standard orthopaedic test is the squeeze test, whereby pressure is applied in a superficial to deep direction from the first and fifth metatarsals, thereby compressing the inter-metatarsal structures and recreating pain in patients with either pathology.47
Routine radiography will normally provide no useful information. Ultrasonography, in the hands of an experienced operator, can be extremely helpful both in diagnosis and for guiding hydrocortisone injection into the site; however, despite the requirement in this instance for contrast, MR imaging is still widely used for evaluation of this region, partly because it is easier to interpret but also because it offers better scope for differentiating Morton’s neuroma from soft tissue tumours. The lesion will be intermediate signal on T1-weighted imaging and low signal on T2-weighted imaging. If contrast is used, the lesion is well demonstrated with intense uptake; contrast can also help with patients who redevelop symptoms after surgical resection in differentiating the development of a new neuroma from scar tissue.42,45
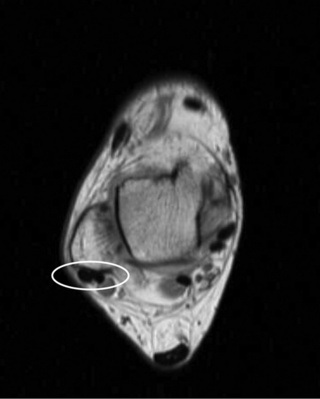
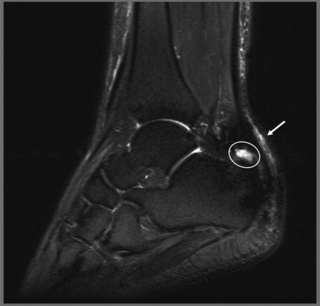
Plantar fasciitis
Whilst MR imaging is not warranted for simple cases of plantar fasciitis, for those patients with persistent pain, or where surgery is being considered, MR imaging may provide additional clinical information to determine the origin of the pain and identify which anatomical structures are involved (Figure 7.23).48 The plantar fascia and involved muscles are well visualized on the sagittal, fluid-sensitive images, which will demonstrate regions of increased signal in and about the tendinous insertions into the calcaneus as well as thickening of the plantar fascia to more than 5 mm in thickness. MR imaging is important in those patients who are resistant to conservative management, to determine the extent of inflammation, identify the muscle origins that are the cause of the pain, provide a visual guide to any intervention for pain relief, and indicate the presence and extent of the commonly associated plantar enthesophyte, which may require surgical excision. It can also differentiate the condition from osteomyelitis in the underlying calcaneus, which can mimic the symptoms.49
1 Haukka E., Leino-Arjas P., Solovieva S., et al. Co-occurrence of musculoskeletal pain among female kitchen workers. Int Arch Occup Environ Health. 2006;80(2):141-148.
2 Young M.F. The physics of anatomy. In: Essential Physics for Muscloskeletal Medicine. Edinburgh: Elsevier; 2009.
3 Moran D.S., Evans R.K., Hadad E. Imaging of lower extremity stress fracture injuries. Sports Med. 2008;38(4):345-356.
4 O’Connor P.J., Rankine J., Gibbon W.W., et al. Interobserver variation in sonography of the painful shoulder. J Clin Ultrasound. 2005;33(2):53-56.
5 Kaplan P., Helms C., Dussault R., Anderson M. Foot and ankle. In: Musculoskeletal MRI. Philadelphia: WB Saunders; 2001:384-430.
6 Beltran J., Shankman S. MR imaging of bone lesions of the ankle and foot. Magn Reson Imaging Clin N Am. 2001;9(3):553-566., xi
7 Bergin D., Morrison W.B. Postoperative imaging of the ankle and foot. Radiol Clin North Am. 2006;44(3):391-406.
8 Moore K. The upper limb. In Clinically Oriented Anatomy, 2nd ed, Baltimore: Williams and Wilkins; 1985:626-793.
9 Standring S., editor. Gray’s Anatomy – Pelvic girdle and lower limb – foot and ankle (Section 115). Edinburgh: Elsevier, 2009.
10 Kaplan P., Helms C., Dussault R., Anderson M. Musculoskeletal MRI. Philadelphia: WB Saunders, 2001.
11 Joseph J. Muscles and fascia of the lower limb. In: Hamilton W., editor. Textbook of Human Anatomy. 2nd ed. London: Macmillan; 1976:179-195.
12 Lee M.H., Chung C.B., Cho J.H., et al. Tibialis anterior tendon and extensor retinaculum: imaging in cadavers and patients with tendon tear. Am J Roentgenol. 2006;187(2):W161-W168.
13 Mengiardi B., Pfirrmann C.W., Vienne P., et al. Anterior tibial tendon abnormalities: MR imaging findings. Radiology. 2005;235(3):977-984.
14 Morrison W.B. Magnetic resonance imaging of sports injuries of the ankle. Top Magn Reson Imaging. 2003;14(2):179-197.
15 Pontell D., Hallivis R., Dollard M.D. Sports injuries in the pediatric and adolescent foot and ankle: common overuse and acute presentations. Clin Podiatr Med Surg. 2006;23(1):209-231. x
16 Moore K. The lower limb. In Clinically Oriented Anatomy, 2nd ed, Baltimore: Williams and Wilkins; 1985:396-564.
17 Cortes Z.E., Harris A.M., Baumhauer J.F. Posterior ankle pain diagnosed by positional MRI of the ankle: a unique case of posterior ankle impingement and osteonecrosis of the talus. Foot Ankle Int. 2006;27(4):293-295.
18 Messiou C., Robinson P., O’Connor P.J., Grainger A. Subacute posteromedial impingement of the ankle in athletes: MR imaging evaluation and ultrasound guided therapy. Skeletal Radiol. 2006;35(2):88-94.
19 Rowe L., Yochum T., editors. Essentials of Skeletal Radiology, 2nd ed, Baltimore: Williams and Wilkins, 2004.
20 Kaplan P., Helms C., Dussault R., Anderson M. Temporomandibular joint. In: Musculoskeletal MRI. Philadelphia: WB Saunders; 2001:169-173.
21 Wischer T.K., Bredella M.A., Genant H.K., et al. Perthes lesion (a variant of the Bankart lesion): MR imaging and MR arthrographic findings with surgical correlation. AJR Am J Roentgenol. 2002;178(1):233-237.
22 Kennedy J. What are osteochondral defects? Available from http://www.osteochondraldefects.com Accessed 02.03.09
23 Malfair D. Therapeutic and diagnostic joint injections. Radiol Clin North Am. 2008;46(3):439-453. v
24 Bhosale A.M., Richardson J.B. Articular cartilage: structure, injuries and review of management. Br Med Bull. 2008;87:77-95.
25 Fritz R.C. MR imaging of osteochondral and articular lesions. Magn Reson Imaging Clin N Am. 1997;5(3):579-602.
26 De Smet A.A., Fisher D.R., Burnstein M.I., et al. Value of MR imaging in staging osteochondral lesions of the talus (osteochondritis dissecans): results in 14 patients. Am J Roentgenol. 1990;154(3):555-558.
27 Sella E.J., Caminear D.S., McLarney E.A. Haglund’s syndrome. J Foot Ankle Surg. 1998;37(2):110-114. discussion 73
28 Lee J.C., Calder J.D., Healy J.C. Posterior impingement syndromes of the ankle. Semin Musculoskelet Radiol. 2008;12(2):154-169.
29 Sofka C.M., Adler R.S., Positano R., et al. Haglund’s syndrome: diagnosis and treatment using sonography. HSS J. 2006;2(1):27-29.
30 Jerosch J., Schunck J., Sokkar S.H. Endoscopic calcaneoplasty (ECP) as a surgical treatment of Haglund’s syndrome. Knee Surg Sports Traumatol Arthrosc. 2007;15(7):927-934.
31 Rowe L., Yochum T. Trauma. In: Yochum T., Rowe L., editors. Essentials of Skeletal Radiology. 2nd ed. Baltimore: Williams and Wilkins; 1996:653-794.
32 Leduc S., Clare M.P., Laflamme G.Y., Walling A.K. Posttraumatic avascular necrosis of the talus. Foot Ankle Clin. 2008;13(4):753-765.
33 Love J.N., O’Mara S. Freiberg’s Disease in the Emergency Department. J Emerg Med. 2008;38(4):e23-5.
34 Patel C.V. The foot and ankle: MR imaging of uniquely pediatric disorders. Magn Reson Imaging Clin N Am. 2009;17(3):539-547. vii
35 Staser J., Karmazyn B., Lubicky J. Radiographic diagnosis of posterior facet talocalcaneal coalition. Pediatr Radiol. 2007;37(1):79-81.
36 Stoller D. Magnetic Resonance Imaging in Orthopaedics and Sports Medicine, 2nd ed. Philadelphia: Lippincott Williams and Wilkins, 1996.
37 Kavanagh E.C., Zoga A.C. MRI of trauma to the foot and ankle. Semin Musculoskelet Radiol. 2006;10(4):308-327.
38 Chilvers M., Donahue M., Nassar L., Manoli A.2nd. Foot and ankle injuries in elite female gymnasts. Foot Ankle Int. 2007;28(2):214-218.
39 Fredrick L.A., Beall D.P., Ly J.Q., Fish J.R. The symptomatic accessory navicular bone: a report and discussion of the clinical presentation. Curr Probl Diagn Radiol. 2005;34(2):47-50.
40 Omey M.L., Micheli L.J. Foot and ankle problems in the young athlete. Med Sci Sports Exerc. 1999;31(suppl 7):S470-S486.
41 Beers M., Berkow R. The Merck Manual, 17th ed. West Point, PA: Merck & Co, 1999.
42 Masala S., Fiori R., Marinetti A., et al. Imaging the ankle and foot and using magnetic resonance imaging. Int J Low Extrem Wounds. 2003;2(4):217-232.
43 Stoller D.W., Tirman P.F., Bredella M.A. Diagnostic Imaging Orthopaedics. Salt Lake City: Amirsys Inc, 2003.
44 Berquist T. MRI of the Musculoskeletal System 4th ed. Philadelphia: Lippincott Williams and Wilkins, 2000.
45 Bancroft L.W., Peterson J.J., Kransdorf M.J. Imaging of soft tissue lesions of the foot and ankle. Radiol Clin North Am. 2008;46(6):1093-1103. vii
46 Hassouna H., Singh D. Morton’s metatarsalgia: pathogenesis, aetiology and current management. Acta Orthop Belg. 2005;71(6):646-655.
47 Eustace S., Johnston C., O’Neill P., O’Byrne J. The foot and ankle. In: Sports Injuries: Examination, Imaging and Management. Edinburgh: Elsevier Churchill Livingstone; 2007:19-86.
48 Osborne H.R., Breidahl W.H., Allison G.T. Critical differences in lateral X-rays with and without a diagnosis of plantar fasciitis. J Sci Med Sport. 2006;9(3):231-237.
49 Recht M.P., Donley B.G. Magnetic resonance imaging of the foot and ankle. J Am Acad Orthop Surg. 2001;9(3):187-199.