Chapter 12 The Ankle and Foot
The ankle and foot perform two major roles: they support the body and propel it forward. In the process of performing these functions, several painful conditions may develop. Many of these develop in the forefoot and are often the result of poorly fitted shoes.
Anatomy
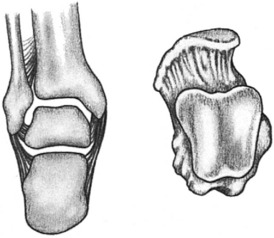
The ankle is a hinge joint composed of the articular surfaces of the lower portion of the tibia, talus, and medial and lateral malleoli (Fig. 12-1). The stability of this joint or “mortise” is maintained by the malleoli and their ligaments, which grasp the talus and prevent medial and lateral displacement. The talus and socket are both broader in front, an arrangement that provides maximum stability when the ankle is in dorsiflexion or neutral, and this prevents posterior displacement. Only movements of dorsiflexion and plantar flexion occur at the ankle.
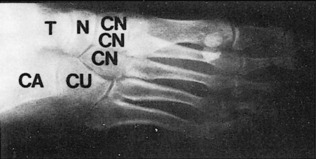
The foot is composed of 26 bones, 12 of which are components of the medial and lateral longitudinal arches (Fig. 12-2). Strong fascial supports maintain these arches and prevent collapse (Fig. 12-3). Eversion and inversion movements of the foot take place in the hindfoot at the subtalar joint. Injury or disease that affects this joint will cause pain in the region of the heel when walking on uneven or irregular surfaces. Abduction and adduction movements occur in the midfoot or midtarsal joints.
Flatfoot
ClINICAL FEATURES
Symptoms are rare but may consist of pain, burning, and easy fatigability. With weight bearing, the heels are everted, and the forefoot appears pronated and abducted (Fig. 12-4). The child often “breaks down” the medial counter of the shoe. When it is not bearing weight, the foot often looks normal. Absence of the medial arch is apparent, and the foot is mobile without any fixed deformity. The child with flatfoot can usually form a good arch when asked to stand on tiptoe. The heel rolls into its usual varus position, and normal strength is apparent. A mild genu valgum (knock-knee) or internal tibial torsion may be present. With the heel inverted, passive dorsiflexion of the ankle will be limited if the heel cord is tight.
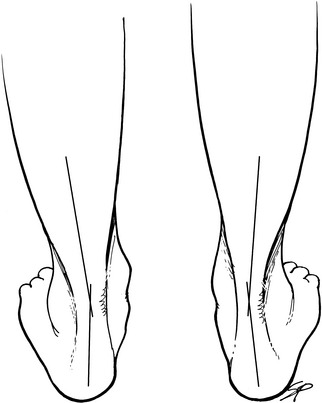
Fig. 12-4 Flatfoot deformity with eversion (valgus) of the heels and loss of the normal longitudinal arch.
A lateral roentgenogram taken with the foot bearing weight may reveal a loss of the normal arch and plantar flexion of the talus (Fig. 12-5). Some secondary bony changes may be present in the adult.
TREATMENT
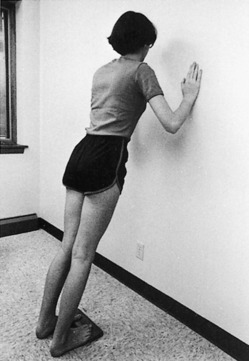
The treatment of flexible flatfoot in the child is controversial. The disorder is considered a normal variant in most cases, and only reassurance is needed. The natural history is spontaneous correction in the majority of cases with maturity. Symptoms are rare during childhood and uncommon even in the adult with moderately severe deformity. Actually, most foot pain in young adults is caused by an abnormally high rather than an abnormally low arch. Shoe corrections and orthotics used for this condition are of uncertain benefit. An arch cannot be “created” by supporting it. Exercises are of doubtful value, except for those that stretch the tight heel cords (Fig. 12-6). These exercises cure many cases associated with heel cord contractures. A soft arch support may be tried if symptoms are present. Surgery is reserved for symptomatic cases but is rarely necessary. No treatment is needed in most cases.
RIGID FLATFOOT
CLINICAL FEATURES
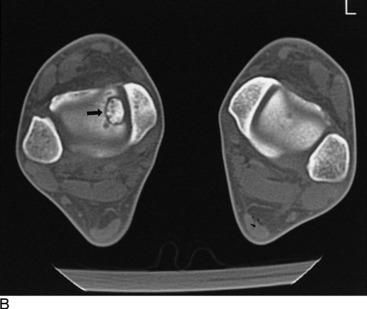
The onset of the disorder is usually gradual and begins in early adolescence if it is caused by a coalition. This may be because of the more solid ossification of the bar that occurs at this age. Stiffness and a painful limp are the most common initial symptoms. Tenderness and pain may be present over the peroneal tendons or in the hindfoot. The heel is frequently everted, and subtalar motion is limited and painful. The forefoot may be abducted. Passive stretching of the peroneal tendons by forefoot adduction and inversion frequently reproduces the pain. Swelling will be present if the disorder is secondary to a rheumatoid process. Roentgenograms may reveal arthritic changes in the hindfoot or the presence of a coalition (Fig. 12-7). Computed tomography (CT) and magnetic resonance imaging (MRI) are valuable in determining the extent of the condition.
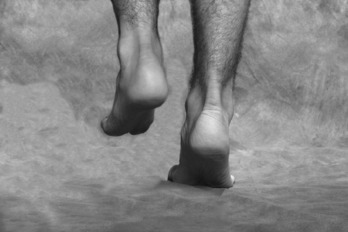
POSTERIOR TIBIAL TENDINOPATHY/RUPTURE
Further deterioration of the tendon could lead to rupture and the development of an acquired flatfoot deformity. Overuse, attrition, and failure are the cause. (Acute rupture of healthy tendon is unusual.) The condition is common, but the diagnosis can be difficult and is often missed until the patient discovers the loss of the arch. Usually, there is a history of previous pain, and the patient may have even had treatment for “tendinitis” in the same area. There is often only minimal pain after rupture, probably because the tendon is no longer attached and is no longer subject to stretch. Normally, the posterior tibial tendon locks the heel in varus, but without it, the heel does not move into inversion with push-off, and the gait is thus weakened. Clinically, the tendon sheath may be empty, and the heel everts with weight bearing. The medial arch is lower, and swelling and mild tenderness may be present. Inversion of the heel and forefoot against resistance is weak. There is also difficulty in performing the single heel rise test, in which the patient tries to rise on the ball of the foot on the affected side (Fig. 12-8). Heel valgus and forefoot abduction also increase gradually, and, as a result, when looking from behind, “too many toes” are visible with the patient standing (Fig. 12-9).
Clubfoot
CLINICAL FEATURES
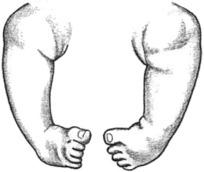
The deformity consists of three major components, none of which is passively correctable. This lack of correctability distinguishes clubfoot from other common foot deformities (which may be caused by intrauterine molding and usually resolve without treatment). The three components are equinus of the ankle and forefoot, varus of the heel, and adduction of the forefoot (Fig. 12-10). The medial border of the foot is concave, and the lateral border is convex.
Calcaneovalgus
CLINICAL FEATURES
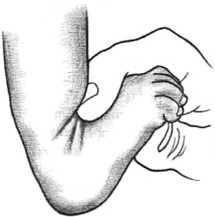
The deformity is easily diagnosed shortly after birth. Marked laxity of the ligaments of the foot and ankle is obvious, and the foot can often be dorsiflexed so that the toes touch the anterior aspect of the tibia (Fig. 12-11). The heel cord may appear to be severely stretched.
Kohler’s Disease (Osteonecrosis of the Tarsal Navicular)
The roentgenographic appearance is usually characteristic. Flattening, sclerosis, and irregularity of the navicular are usually present (Fig. 12-12).
Ankle Sprains
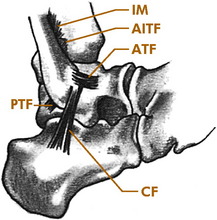
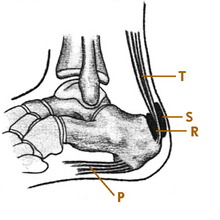
The sprain is the most common of all ankle injuries and may be the most common injury in sports. Most of these (85%) involve the lateral ligament complex as a result of excessive inversion. Medial sprains involving the deltoid ligament are rare. The anterior talofibular (ATF) ligament is usually injured first in the typical lateral sprain (Fig. 12-13). More severe injuries involve the calcaneofibular (CF) ligament. Only rarely is the posterior talofibular ligament involved. The injuries are often graded I, II, and III, with I being mild and II being moderate. Grade III injuries are more severe, with instability resulting from rupture of the ATF and CF ligaments. Inversion (varus) sprains may also cause marked hemorrhage of the peroneal muscles and even peroneal nerve damage. The subtalar joint may also be injured.
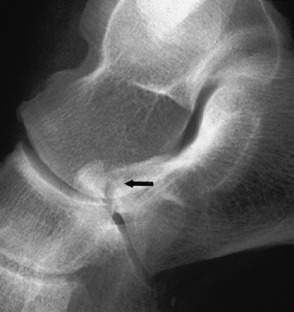
CLINICAL FEATURES
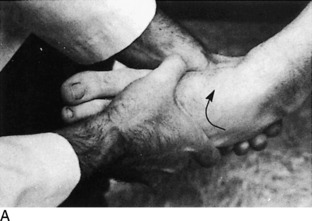
Physical examination is important. Hemorrhage and local tenderness are present at the site of injury. Careful palpation can localize the site of damage. Tendon function should be assessed, and any bony tenderness should be noted. The clinical evaluation of stability is sometimes helpful since it may determine the course of treatment, although this part of the examination may need to be deferred because of pain. Stability of lateral injuries can be assessed by the anterior drawer and talar tilt tests (Fig. 12-14). The anterior drawer is the most reliable test and least painful in the acute stage. Positive test results indicate complete rupture of the ATF and CF ligaments and a grade III injury. Motor function should always be evaluated.
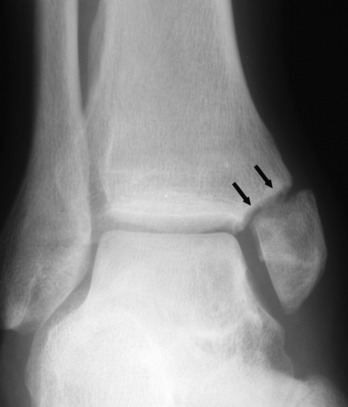
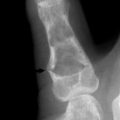
Roentgenographic evaluation is always performed, and because the mechanism of injury that causes a lateral sprain is the same as that which causes an avulsion fracture of the base of the fifth toe, the film should include the fifth metatarsal base to rule out fracture of the small toe. If the injury is in a child or adolescent with open growth plates, tenderness over the fibular malleolus (even with normal roentgenographic findings) implies the more likely growth plate fracture rather than a lateral sprain, and a cast is usually necessary. Opinions vary on the usefulness of arthrograms, tenograms, and stress films (Fig. 12-15). A good clinical examination is usually sufficient to determine stability.
TREATMENT
Regardless of the severity, almost all sprains are treated nonoperatively. At first, all injuries are elevated, and a soft compression dressing is applied for comfort and to help control swelling. Ice (1 hour on, 1 hour off) is applied, and crutches are used for ambulation. Rest, ice, compression, and elevation (RICE) are continued for 1 to 2 days. Anti-inflammatory medication has been recommended in the past for these injuries because it was thought that suppressing the local inflammation could allow faster recovery from sprains and other similar soft tissue injuries. The use of these drugs under these circumstances has been the source of considerable debate, mainly because prostaglandins play important roles in the healing process and these medications block their production. The effects of NSAIDs on soft tissue healing are not clear, and any apparent benefits may only be because of their analgesic effects. Whether these drugs are helpful or harmful in these cases has not been determined. Crutches are frequently needed for 2 to 3 days. Heat is never used.
The next phase of treatment is rehabilitation, which includes early active range-of-motion exercises (circumduction) and weight bearing as tolerated (Fig. 12-16). “Alphabet” exercises (writing the alphabet in capital letters with the great toe) are begun, and in 4 to 5 days, exercise against resistance is added. Wrapping or bracing with a stabilizing orthosis may also be helpful. Static bicycling may be added after 1 week, along with fast walking.
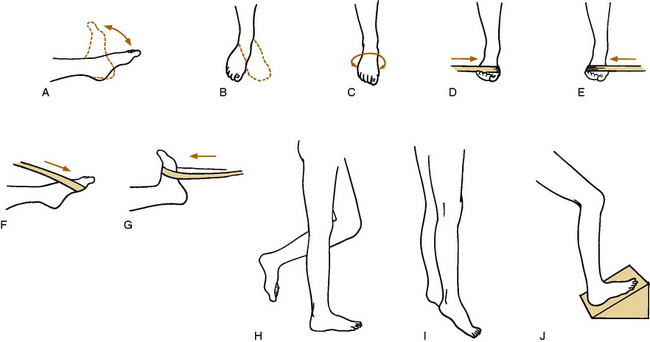
Fig. 12-16 Ankle exercises. A-C, Range of motion (dorsiflexion, plantar flexion, circumduction, and writing the alphabet with the great toe). D-G, Strengthening exercises using a rubber strap (invertors, evertors, plantar flexors, and dorsiflexors). H, Static one-leg standing with eyes closed. I, Toe raises. J, Heel cord stretches. Each exercise is performed 10 to 15 times. Ice is applied for a few minutes before and after each exercise period, and the exercises are performed 3 times each day.
NOTE: Lateral sprains of any severity may also cause lingering symptoms for weeks and months. Some syndesmotic sprains take even longer to heal (55 days vs 35 days for lateral sprains), and heterotopic ossification may even develop in the interosseous membrane. (Unless symptoms occur, long-term results are not usually affected by such ossification.) If healing seems delayed, the following conditions should be considered: (1) talar dome fracture, (2) reflex sympathetic dystrophy, (3) chronic tendinitis, (4) peroneal tendon subluxation, (5) another occult fracture—such as that involving the anterior superior process of the calcaneus or the lateral process of the talus, (6) poor rehabilitation, and (7) the high sprain. Evaluation at this point should start by another clinical examination and simply repeating the plain roentgenograms (Fig. 12-17). CT, bone scan, or MRI may be indicated at a later time.
Ankles that are chronically unstable because of lateral ligamentous laxity may benefit from the application of a 0.3-cm lateral heel and sole wedge to prevent inversion. Taping or bracing during vigorous activities is also helpful, as are strengthening exercises. Continuing symptoms may require surgical reconstruction of the lateral ligaments to relieve symptoms of instability, although late traumatic arthritis or chronic instability is rare regardless of treatment.
Tarsal Tunnel Syndrome
Nerve entrapment rarely may occur in the foot by compression of the posterior tibial nerve beneath the flexor retinaculum at the ankle. This retinaculum arises from the medial malleolus and inserts into the medial aspect of the calcaneus (Fig. 12-18). Space-occupying lesions, local tendinitis, traction injuries, fibrosis secondary to fractures, or deformities of the heel and foot can all compromise the tunnel and cause pressure on the posterior tibial nerve. The disorder is controversial, and there are many unanswered questions regarding its diagnosis and incidence.
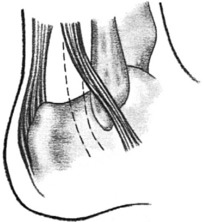
Subluxation of Peroneal Tendons
Sudden, forceful dorsiflexion of the foot accompanied by contraction of the peroneal muscles may cause a tear in the retinaculum that holds these tendons in their groove behind the lateral malleolus. This may allow the tendons to acutely or chronically sublux over the lateral malleolus (Fig. 12-19). The condition can also follow a severe lateral ankle sprain.
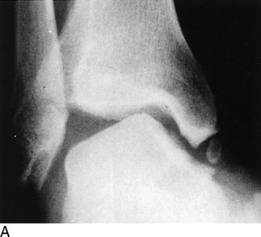
Osteochondritis Dissecans of the Talus (Talar Dome Fracture)
Disorders of the Hindfoot
PLANTAR FASCIITIS (“PAINFUL HEEL SYNDROME”)
CLINICAL FEATURES
The pain is usually felt directly beneath the calcaneus but may be present in the area of the medial arch. The discomfort is characteristically worse with the first steps in the morning or after periods of prolonged sitting and later in the day after weight-bearing activities. Morning pain usually lessens as the foot “warms up.” Examination reveals local point tenderness in the area of involvement, usually the medial tubercle of the calcaneous. The pain may be aggravated by direct pressure or by maneuvers that place the fascia under a strain, such as dorsiflexing the toes and ankle. Some patients have a tight heel cord.
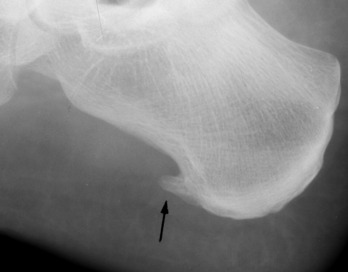
Roentgenographic findings are usually normal but may reveal a traction spur on the os calcis that is directed distally (Fig. 12-21). The significance of this osteophyte in the etiology of symptoms is unknown. It may be a response to muscle tension and is frequently found in the asymptomatic foot. It is not considered the cause of pain. A stress fracture or other bony disorder may need to be ruled out in some cases (Fig. 12-22).
TREATMENT
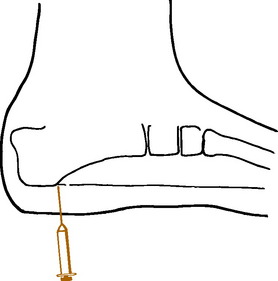
Taping, relief pads, heel cups, cushions, and various orthoses have all been used with only modest success. Over-the-counter pads and cups are as effective as more expensive orthoses. No treatment designed to cushion the heel seems to help, probably because heel strike may not be the cause of the problem. Exercises that stretch the heel cord and plantar fascia may help, but they should not be performed in the acutely painful foot. Only a gentle pulling sensation should be felt. Cold or ice as counterirritants may promote temporary relief. A heel lift or high-heeled shoe may relieve pain in some cases. Oral anti-inflammatory medication is used as necessary. Many patients will benefit from local infiltration of the tender area with a steroid/lidocaine mixture (Fig. 12-23). The injection may be repeated three to four times. (Avoid injecting the superficial tissue, which could cause fat pad necrosis.) Application of a short leg walking cast or removable cast-boot for 6 weeks is often very beneficial. Custom-fitted tension night splints that hold the foot in slight dorsiflexion are used in some resistant cases. Physical therapy is not usually recommended. Extracorporeal shock wave therapy has even been tried, but the results are inconclusive.
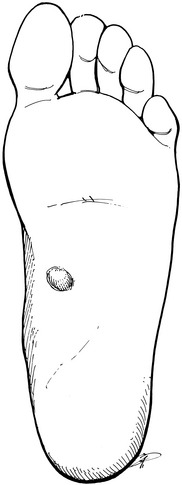
PLANTAR FIBROMATOSIS
This disorder is a fibrous tissue proliferation of the plantar fascia similar to Dupuytren’s contracture in the palm. Clinically, the plantar lesion usually involves the medial half of the middle of the plantar fascia but rarely causes a contracture, in contrast to Dupuytren’s disease of the hand. The lesion generally begins as a painless subcutaneous nodule that slowly enlarges and eventually becomes tender (Fig. 12-24). Treatment with a molded orthotic may allow transfer of the weight away from the nodule. Surgery is often indicated when weight bearing becomes painful. Recurrence after excision is common.
ACHILLES TENDINITIS
Overuse of the calf muscles may result in inflammatory pathologic changes (tendinosis) in the Achilles tendon, either acute or chronic. This disorder is frequently seen in the athlete. Pain, local tenderness, swelling, and a dry crepitus may be present. The tendon is often thickened in chronic cases. Passive stretching of the tendon by dorsiflexion of the ankle typically aggravates the pain. Calcification of the tendon may even occur.
BURSITIS
Two bursae are consistently present near the insertion of the Achilles tendon (Fig. 12-25). The superficial bursa may be irritated by the constant rubbing of the counter of the shoe. The retrocalcaneal bursa may be irritated by a prominent posterosuperior angle of the calcaneus (Haglund’s disease). The treatment of both conditions is similar. Relief pads, heat, and elevation of the heel of the shoe with a soft cushion are usually sufficient. Deep bursitis may respond to steroid injection, avoiding the tendon. Occasionally, the bursa and any underlying bony prominence may have to be resected.
CALCANEAL APOPHYSITIS
A low-grade inflammatory reaction at the insertion of the Achilles tendon is frequently seen in boys between the ages of 8 and 14 years in association with irregular ossification and sclerosis of the calcaneal apophysis (Fig. 12-26). This disorder, sometimes referred to as Sever’s disease, is similar in nature to Osgood–Schlatter disease of the knee. The condition is often bilateral. Local pain, tenderness, and swelling that are aggravated by activity are common. Passive stretching of the heel cord may reproduce the pain.
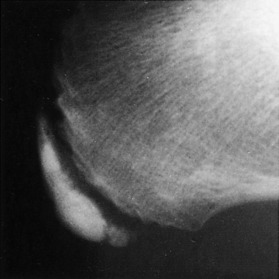
Fig. 12-26 Roentgenogram of the heel in Sever’s disease. Sclerosis of the apophysis is a normal finding.
Treatment includes NSAIDs, local heat, and the avoidance of activity. A 1.25-cm heel lift may diminish the stress on the heel cord. Stretching exercises may help. A short leg walking cast applied with the foot in slight equinus may be necessary in the rare resistant case. The disease is always self-limited.
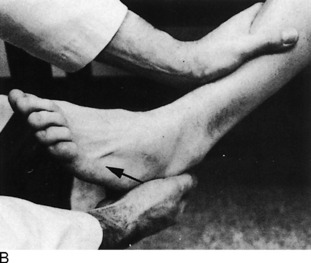
ACHILLES TENDON RUPTURE
CLINICAL FEATURES
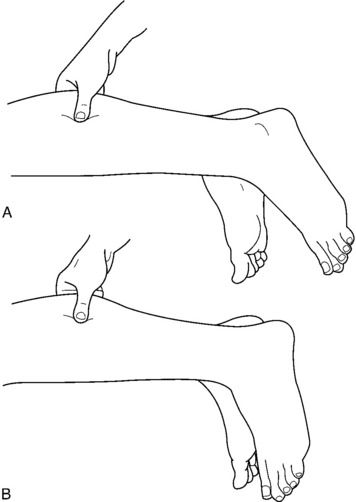
Rupture frequently occurs during an activity that puts stress on the tendon, such as jumping or pushing off with the weight on the forefoot. The acute injury is often associated with a “pop,” and the patient often describes the feeling that the heel was shot or kicked by someone. After the injury, the patient walks flatfooted and is unable to stand on the ball of the foot. Tenderness and hemorrhage are present, and a sulcus is usually palpable at the site of the rupture. However, this sulcus may be obscured by an organizing clot if the examination is delayed (a fact that may explain the difficulty in early diagnosis). Although active plantar flexion is usually lost, some flexion occasionally remains because of the activity of the other posterior compartment muscles. Thompson’s squeeze test is usually abnormal (Fig. 12-27). Excessive passive dorsiflexion of the ankle will also be present and with the feet hanging, the injured side may also rest in more dorsiflexion.
Disorders of the Forefoot
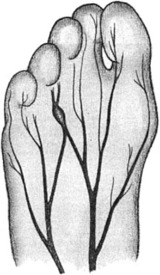
MORTON’S NEUROMA
A common cause of pain in the forefoot is the interdigital neuroma. This lesion results from perineural fibrosis of the plantar nerve where the medial and lateral plantar branches communicate (Fig. 12-28). It may represent an entrapment neuropathy similar to carpal tunnel syndrome. The condition is probably secondary to repetitive trauma, and the fibrosis results in a painful fusiform swelling of the nerve. Females are more commonly affected. Tight shoe wear may be a cause.
TREATMENT
A pad that separates the heads of the third and fourth metatarsals may be helpful. NSAIDs may be tried, and a local injection of a steroid/lidocaine mixture into the tender web area from a dorsal approach may give some relief (Fig. 12-29). The patient should avoid tight-fitting shoes. Surgical removal of the neuroma is often necessary.
METATARSALGIA
Pain beneath the metatarsal head is referred to loosely as metatarsalgia. The term is used to describe a nonspecific symptom usually involving the lesser toes. Often, no obvious cause is found, but a variety of abnormalities may be responsible for the pain, including an abnormally high arch, Morton’s neuroma, synovitis of the second metatarsophalangeal (MTP) joint, improper shoe selection (especially a high-heeled shoe), and a tight Achilles tendon. The disorder is frequently associated with hammertoes, clawed toes, and a hallux valgus deformity.
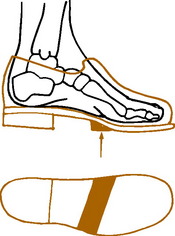
TREATMENT
The object of treatment is to transfer the weight-bearing pressure away from the affected metatarsal heads onto the metatarsal neck and shaft. The calluses that form secondary to the abnormal pressure usually disappear with time. A low-heeled shoe with sufficient room in the forefoot is recommended. An extra-depth shoe is prescribed when contracture or clawing is present. A metatarsal bar may be added to transfer the weight behind the metatarsal heads (Fig. 12-30). Relief donut pads may be applied around any tender callous. Warm soaks followed by pumice stone abrasion to decrease callous volume are helpful. Surgery is reserved for those cases that fail to respond to conservative treatment in those patients who have a clearly defined cause.
FREIBERG’S DISEASE
Freiberg’s disease is a disorder of unknown cause in which aseptic necrosis occurs in one of the metatarsal heads, usually the second. The condition is most common in adolescence, and girls are more often affected. The disorder is usually unilateral.
Hallux Valgus
CLINICAL FEATURES
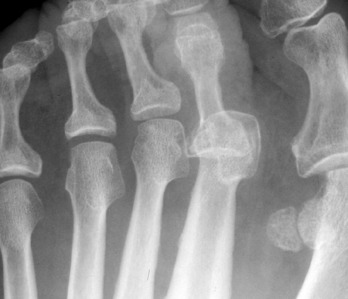
Roentgenographic findings include lateral displacement of the proximal phalanx and the presence of a medial exostosis (Fig. 12-33). Degenerative changes may also be present in the MTP joint.
TREATMENT
Conservative treatment is directed at relieving the pressure over the painful bunion prominence. Properly fitted, low-heeled shoes fitted to accommodate the bunion are effective. Sometimes, the toe portion needs to be stretched. An “extra-depth” shoe may be required to accommodate a dorsiflexed second toe. A splint that separates the first and second toes may also be beneficial. Even tight hose that pull the phalanges together should be avoided. Local measures, such as rest and moist heat, are indicated when acute pain is present. More than half of the cases respond to nonsurgical care, but this often means a permanent lifestyle change in the type of shoe the patient wears. Disabling pain with deformity is the indication for surgery. Excision of the exostosis and realignment of the great toe are usually performed.
Hallux Rigidus
CLINICAL FEATURES
The roentgenogram usually reveals typical findings of degenerative arthritis with joint narrowing and spur formation (Fig. 12-34).
TREATMENT
Symptomatic relief can be obtained by rest, moist heat, and anti-inflammatory medication. An intraarticular injection of steroid may provide additional relief (Fig. 12-35). A shoe with sufficient room in the forefoot is worn, and an anterior metatarsal bar is applied to the shoe. A rockerbottom shoe may also be tried. It allows the foot to roll over without dorsiflexion of the toes, but it is awkward in appearance. Arthroplasty or arthrodesis of the MTP joint is indicated in resistant cases.
Hallux Varus
Hallux varus is a deformity, usually seen in children, in which medial angulation of the great toe occurs at the MTP joint. It is usually congenital and associated with other foot deformities, but it may be seen in adults following surgical overcorrection of a hallux valgus deformity. Mild cases in children may respond to passive stretching exercises and proper shoe wear. More severe cases in both adults and children usually require surgical correction.
Congenital Overlapping Fifth Toe
This is a common familial deformity, frequently bilateral, in which the small toe is dorsiflexed and may come to lie on the top of the fourth toe (Fig. 12-36). The capsule and extensor tendon on the dorsum of the metatarsophalangeal joint are shortened and do not allow passive correction of the deformity. Calluses may develop on the dorsum of the toe secondary to chronic irritation by the shoe. Passive stretching of mild deformities is indicated but usually does not completely correct the problem. Surgical realignment or even amputation may be necessary in symptomatic cases.
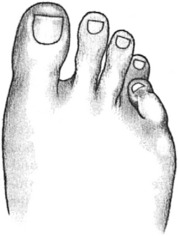
Hammertoe
A hammertoe is one in which a flexion deformity develops at the proximal interphalangeal joint and causes the tip of the toe to be depressed downward (Fig. 12-37). A mild hyperextension deformity at the MTP joint may be present. Painful calluses develop over the tip of the toe, over the dorsum of the proximal interphalangeal joint, and under the metatarsal heads. The second toe is most commonly affected, and the disorder is frequently seen in association with a hallux valgus deformity of the great toe. The cause is often improperly fitted, tight shoes that crowd the toes.
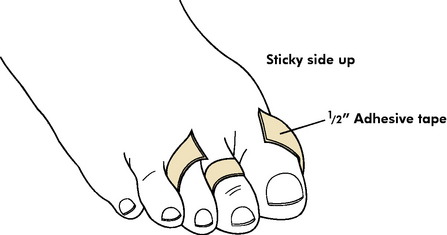
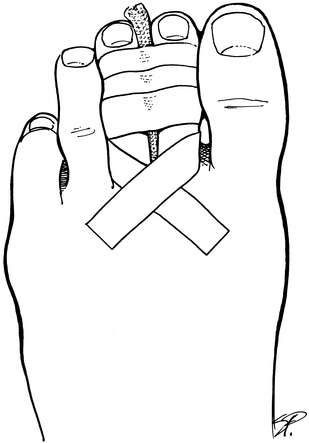
Mild flexible deformities may be corrected by stretching exercises and “over-and-under” taping to adjacent toes (Fig. 12-38). Toe caps or pads may also be helpful. Properly fitted or shoes are a must. Extra-depth shoes may be needed. Resistant cases usually require surgical correction.
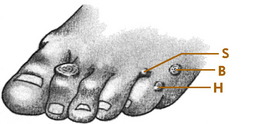
Corns and Calluses
Removal of the external pressure is essential in the conservative management of all of these soft tissue lesions in the forefoot. A low-heeled shoe with adequate width in the forefoot is recommended. Donut relief pads and metatarsal bars are usually helpful. Warm soaks in soapy water followed by the application of a keratolytic medication, such as salicylic acid salve, will help eliminate the callus or corn. The normal skin should be avoided when applying the salve. The salve should remain in place for 3 to 5 days and be covered by adhesive tape. The patient should watch for skin maceration. After the tape is removed, the hard callus or corn may be shaved in layers. After warm soaks, a pumice stone may also be used to pare down the callus. This procedure is frequently helpful, but deep excision of any corn or callus should be avoided because an infected ulcer may result. Soft corns may be eliminated in 1 to 2 weeks, but hard calluses may take longer. A cotton pad or lamb’s wool may be placed between the toes if a soft corn is present, and a doughnut-shaped pad is always worn around a hard corn or callus to shift weight from the lesion to the adjacent normal skin. The toes should be kept as dry as possible at all times.
Surgical correction may be advised in resistant cases to eliminate the bony prominence.
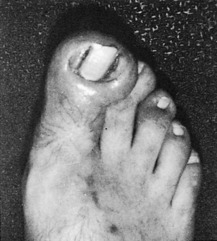
Disorders of the Toenail
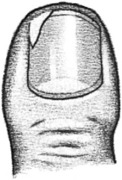
A common condition that affects mainly the great toe is the ingrown nail. In this disorder, the nail does not actually grow into the soft tissue, but instead, the soft tissue overgrows and obliterates the nail sulcus (Fig. 12-39). The nail itself is usually normal, although some older patients have incurved nails. The causes are probably multiple, but incorrect nail trimming, cleaning the nail gutters with sharp tools that penetrate the skin, improperly fitted tight shoes and stockings, and bony deformities have all been implicated. A simple break in the skin can create a portal of entry for bacteria. Because of improper trimming, a small nail spike may even be formed that continues to grow and irritate the soft tissue (Fig. 12-40). A chronic infection is usually the end result. Unusual bony lesions such as subungual exostosis should be ruled out with routine radiographs.
In most mild early cases, soaks, antibiotics, and proper shoes and stockings may be curative. The nail edge should be kept elevated with a soft cotton wad or metal shield until it grows out beyond the soft tissue reaction. Unfortunately, this can be a slow process, because the nail takes approximately 3 months to grow 1 cm. Patience is required. Proper transverse trimming of the nail should prevent recurrences.
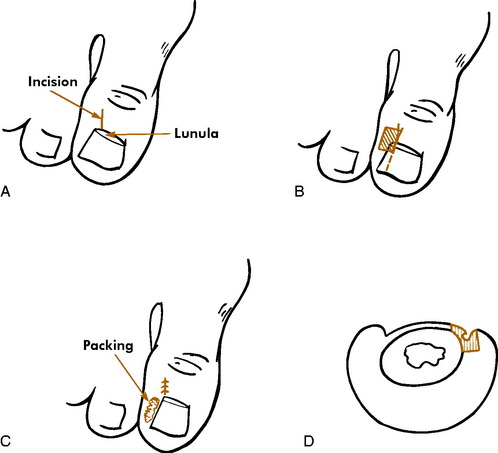
Surgery for nail margin removal is as follows (Fig. 12-41):
ONYCHOMYCOSIS
TREATMENT
Topical and systemic therapy are both available, although local treatment alone has a low success rate. Ciclopirox nail lacquer applied twice a day may help in mild cases but may need to be used longer than a year. Systemic therapy is usually required in most cases. The newer antifungals, such as itraconazole and terbinafine, are better than older medications (such as griseofulvin), although they are somewhat costly. A 25% to 50% cure rate has been reported with these drugs. Oral agents require periodic medical monitoring. Treatment with most of the oral medications is usually for 3 months.
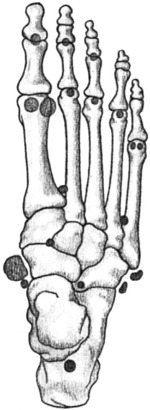
Accessory Bones
Many accessory and sesamoid bones are present in the normal foot (Fig. 12-42). They are occasionally confused with fractures. Most are asymptomatic. However, an unusually large accessory navicular bone may cause pain from local pressure where the prominence protrudes against the shoe (Fig. 12-43). It is usually bilateral and is frequently associated with weakness in the longitudinal arch and a mild flatfoot deformity. Relief pads or shoe modifications may eliminate symptoms, but surgical excision of the bony prominence is sometimes necessary to completely relieve the pain.
Fractures of the Ankle
The ankle joint or “mortise” is an inverted U with the dome of the talus fitting between the medial and lateral malleoli. The posterior margin of the tibia is often called the third or posterior malleolus.
TREATMENT
The two most important clinical and roentgenographic assessments that determine the treatment of ankle fractures are: (1) the position of the talus in the mortise and (2) the stability of the fracture. If the talus is already displaced, referral is indicated because reduction is required, sometimes by surgical means, to restore the ankle mortise (Fig. 12-44). Any deviation of the position of the talus in the joint could lead to traumatic arthritis.

Fig. 12-46 Minimally displaced fracture of the lateral malleolus (arrow) with no widening of the ankle mortise.
Fractures with dislocation of the talus should be reduced as rapidly as possible (Fig. 12-49). If the dislocation is not promptly reduced, severe soft tissue injury with blistering and skin breakdown may result. Definitive surgical treatment of the fractures may also have to be delayed. The dislocation is reduced by traction and manipulation with the patient under local anesthesia. After reduction, the ankle is placed in a soft “Jones” bulky compression dressing reinforced with plaster splints. Any necessary surgery can then be performed on an elective basis.
Fractures of the Foot
FRACTURES OF THE CALCANEUS
Fracture of the calcaneus usually results from a fall on the heel; 10% of such injuries are associated with a compression fracture of the lumbar spine. (The heel is usually so painful that the back pain may not be noticed until much later.) The os calcis is usually crushed, and the fragments are displaced in varying amounts (Fig. 12-50).
FRACTURES OF THE TALUS
Fractures of the neck of the talus can be more problematic (Fig. 12-51). Outcomes depend greatly on the amount of initial displacement. Undisplaced fractures have a favorable prognosis in most instances. Displacement carries a worse prognosis. Osteonecrosis, malunion, and nonunion are common complications, and operative treatment is often required to prevent them.
FRACTURES OF THE METATARSALS
Displaced fractures of the necks of the metatarsals may need reduction to prevent pain from developing under the metatarsal heads (Fig. 12-52). Manipulation is sometimes effective, but maintenance of the reduction is frequently difficult. Open reduction with internal fixation is sometimes necessary.
Fractures of the base or styloid of the fifth metatarsal are common and result from an inversion injury to the foot (Fig. 12-53). They are usually undisplaced and require little treatment. A light compression dressing and hard-soled sandal are usually sufficient. Crutches may be necessary for 7 to 10 days, and healing is usually complete in 5 to 6 weeks. Nonunion is unusual, and even when it occurs it is rarely symptomatic.
Fractures of the shaft of the fifth metatarsal, especially proximal ones, heal slowly and may require a short leg walking cast for 6 to 8 weeks (Fig. 12-54). The cortex of the proximal diaphysis is normally thick and often relatively avascular, especially in long-distance runners, due to high stresses. The relatively poor circulation in this area may lead to delayed union and even nonunion. Surgical intervention may even be required.
LISFRANC’S INJURY
Radiographic findings in subtle injuries may be missed. An important key is the alignment of the second metatarsal with the middle cuneiform. A line drawn along the medial aspect of the metatarsal should be continuous with a line along the medial aspect of the cuneiform. Comparison views with the normal foot may be needed. A shift of the base of the second metatarsal may be noted, and a small avulsion fracture, sometimes called a fleck sign or Lisfranc’s fragment, may be seen (Fig. 12-55).
Undisplaced fractures are treated with immobilization, but if there is any indication of displacement, orthopedic referral is needed to determine whether surgery may be indicated to avoid the late complication of posttraumatic arthritis.
FRACTURES OF THE PHALANGES
Fractures of the toes are common and usually require little treatment. Undisplaced fractures may be treated by taping the injured toe to the adjacent toe for 3 to 4 weeks (Fig. 12-56). Displaced fractures can usually be reduced without anesthesia. Open reduction is rarely necessary. However, fractures of the proximal phalanx of the great toe should be reduced accurately.
Foot Care
When ulcers do develop, they are most common on the weight-bearing surface of the foot or on the medial aspect of the great toe. These are often referred to as mal-perforans (Fig. 12-57). At this stage, vigorous local care, minor debridement, and control of infection are indicated. Excessive heat, which places a great demand on the soft tissue, should be avoided. The previously mentioned metatarsal bars and insoles are used to relieve the pressure on the ulcer. If the foot is warm and has pulses, amputation is usually not necessary, and healing of these ulcers commonly occurs with proper care.
SHOES
The same pragmatic approach may be taken regarding children’s shoes. Only rarely are special shoes ever needed, and there are absolutely no advantages for children to wear the traditional, expensive, high-topped leather shoe. (Societies in which shoes are not worn actually have fewer foot deformities.) Children may outgrow 2 to 4 pairs each year, and the total cost of such shoes would be considerable even if they were of some benefit. Children wear shoes to keep the feet warm and prevent harm from sharp objects. Otherwise, they may go barefooted as much as they like or wear any inexpensive brand as long as the shoes are comfortable.
Aldridge T. Diagnosing heel pain in adults. Am Fam Physician. 2004;700:332-338.
Beskin JL. Nerve entrapment syndromes of the foot and ankle. J Am Acad Orthop Surg. 1997;5:261-269.
Bleck EE. The shoeing of children: sham or science? Dev Med Child Neurol. 1971;13:188-195.
Buchbinder R. Clinical practice. Plantar fasciitis. N Engl J Med. 2004;350:2159-2166.
DeMaio M, Paine R, Manginer E, et al. Plantar fasciitis. Orthopedics. 1993;16:1153-1163.
DuVries HL. Surgery of the foot, ed 2, St Louis: CV Mosby Co, 1965.
Furey JG. Plantar fasciitis. The painful heel syndrome. J Bone Joint Surg Am. 1975;57:672-673.
Greenfield GB. Radiology of bone diseases. Philadelphia: JB Lippincott, 1969.
Greig JD. Results of surgery for ingrowing toenails. J Bone Joint Surg Br. 1989;71:859.
Heifitz CJ. Ingrown toenail: a clinical study. Am J Surg. 1937;37:298.
Helfet AJ. A new way of treating flat feet in children. Lancet. 1956;1:262-264.
Johnson KA. Surgery of the foot and ankle. New York: Raven Press, 1989.
Lawrence SJ, Grau GF. Management of acute Achilles tendon ruptures. Orthopedics. 2004;27:579-581.
Lee TH, Wapner KL, Hecht PJ. Plantar fibromatosis. J Bone Joint Surg Am. 1993;75:1080-1084.
Maffulli N, Kader D. Tendinopathy of tendo achillis. J Bone Joint Surg Br. 2002;84:1-8.
Mann RA. Disorders of the first metatarsophalangeal joint. J Am Acad Orthop Surg. 1995;3:340-343.
Mazzone MF, McCue T. Common conditions of the achilles tendon. Am Fam Physician. 2002;65:1805-1810.
Michelson JD. Fractures about the ankle, J Bone Joint Surg Am. 1995;77:142-152.
Milgram JE. Office measures for relief of the painful foot. J Bone Joint Surg Am. 1964;46:1095-1116.
Paley D, Hall H. Intra-articular fractures of the calcaneus. J Bone Joint Surg Am. 1993;75:342-355.
Pecina M. Diagnostic tests for tarsal tunnel syndrome. J Bone Joint Surg Am. 2002;84-A:1714-1715.
Pedowitz WJ, Kovatis P. Flatfoot in the adult. J Am Acad Orthop Surg. 1995;3:293-302.
Prichasuk S. The heel pad in plantar heel pain. J Bone Joint Surg Br. 1994;76:140-142.
Roberts C, Deliss L. Acute rupture of tendo Achillis. J Bone Joint Surg Br. 2002;84:620.
Rockwood CA, Green DP. Fractures in adults, ed 2, Philadelphia: JB Lippincott, 1984.
Saltzman CL, Tearse DS. Achilles tendon injuries. J Am Acad Orthop Surg. 1998;6:316-325.
Schwend RM, Drennen JC. Cavus foot deformity in children. J Am Acad Orthop Surg. 2003;11:201-211.
Stone JW. Osteochondral lesions of the talar dome. J Am Acad Orthop Surg. 1996;4:63-73.
Sullivan JA. Pediatric flatfoot: evaluation and management. J Am Acad Orthop Surg. 1999;7:44-53.
Sykes PA. Ingrowing toenails: time for critical appraisal? J R Coll Surg Edinb. 1986;31:300-304.
Tachdjian MO. Pediatric orthopedics. Philadelphia: WB Saunders Co, 1972.
Vincent KA. Tarsal coalition and painful flatfoot. J Am Acad Orthop Surg. 1998;6:274-281.
Wuest TK. Injuries to the lower extremity syndesmosis. J Am Acad Orthop Surg. 1997;5:172-181.