Chapter 441 The Anemias
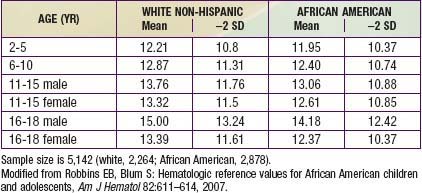
Anemia is defined as a reduction of the hemoglobin concentration or red blood cell (RBC) volume below the range of values occurring in healthy persons. “Normal” hemoglobin and hematocrit (packed red cell volume) vary substantially with age and sex (Table 441-1). There are also racial differences, with significantly lower hemoglobin levels in African-American children than in white non-Hispanic children of comparable age (Table 441-2).
Table 441-1 NORMAL MEAN AND LOWER LIMITS OF NORMAL FOR HEMOGLOBIN, HEMATOCRIT, AND MEAN CORPUSCULAR VOLUME
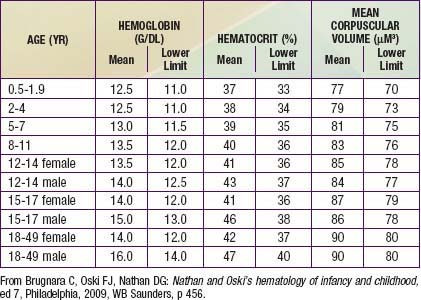
Table 441-2 NHANES III HEMOGLOBIN VALUES FOR NON-HISPANIC WHITES AND AFRICAN AMERICANS AGED 2-18 YEARS
Differential Diagnosis
Anemia is not a specific entity but rather can result from any of number of underlying pathologic processes. In order to narrow the diagnostic possibilities, anemias may be classified on the basis of their morphology and/or physiology (Fig. 441-1).
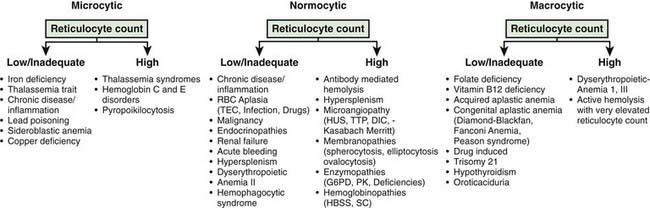
Figure 441-1 Use of the mean corpuscular volume (MCV) and reticulocyte count in the diagnosis of anemia.
(Adapted from From Brunetti M, Cohen J: The Harriet Lane handbook, ed 17, Philadelphia, 2005, Elsevier Mosby, p 338.)
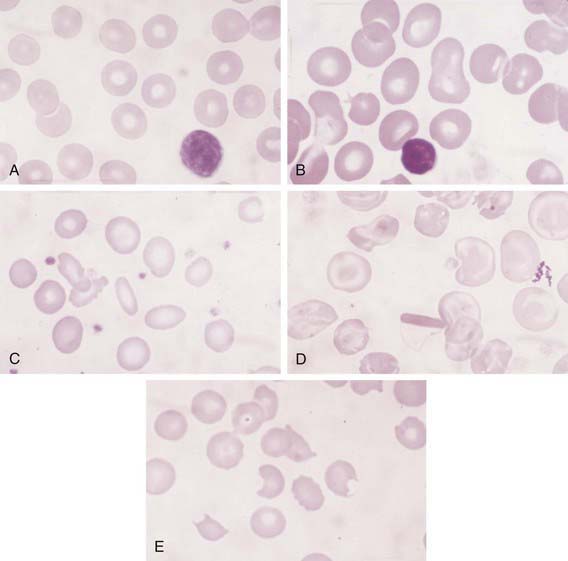
Anemias may be morphologically categorized on the basis of RBC size (mean corpuscular volume [MCV]), and microscopic appearance. They can be classified as microcytic, normocytic, or macrocytic based on whether the MCV is low, normal, or high, respectively. RBC size also changes with age, and normal developmental changes in MCV should be recognized before a designation is made (see Table 441-1). Examination of a peripheral blood smear often reveals changes in RBC appearance that will help to further narrow the diagnostic categories (Fig. 441-2). Details regarding morphologic changes associated with particular disorders are described in subsequent sections.
Figure 441-1 presents a useful approach to assessing the common causes of anemia in the pediatric age group. Children with microcytic anemia and low or normal reticulocyte counts most often have defects in erythroid maturation or ineffective erythropoiesis. Iron deficiency (Chapter 449) is the most common cause. Thalassemia trait (Chapter 456) constitutes the primary differential diagnosis when iron deficiency is suspected. Distinctions between these entities are presented in Table 449-1 (Chapter 449). Chronic disease or inflammation (more often normocytic), lead poisoning, and sideroblastic anemias should also be considered and are discussed in other chapters. Microcytosis and elevated reticulocyte counts are associated with thalassemia syndromes and hemoglobin C and E (Chapter 456). Notably, thalassemias and hemoglobinopathies are most commonly seen in patients of Mediterranean, Middle Eastern, African, or Asian background.
Normocytic anemia and low reticulocyte count characterize a large number of anemias. The anemia of chronic disease/inflammation (Chapter 445) is usually normocytic. The anemia associated with renal failure, caused by reduced erythropoietin production, will invariably be associated with clinical and laboratory evidence of significant kidney disease. Decreased or absent red cell production secondary to transient erythroblastopenia of childhood (TEC), infection, drugs, or endocrinopathy usually results in a normocytic anemia, as does bone marrow infiltration by malignancy. In the case of invading leukemia or malignancy, abnormal leukocytes or tumor cells in association with thrombocytopenia or reduced or elevated white cell counts may be seen. Acute bleeding, hypersplenism, and congenital dyserythropoietic anemia (CDA) type II (Chapter 446) are also normocytic.
The anemia seen in children with macrocytic blood cells is sometimes megaloblastic (Chapter 448), resulting from impaired DNA synthesis and nuclear development. The peripheral blood smear in megaloblastic anemias contains large macrovalocytes, and the neutrophils often show nuclear hypersegmentation. The major causes of megaloblastic anemia include folate deficiency, vitamin B12 deficiency, and rare inborn errors of metabolism. Other macrocytic anemias with low or normal reticuclocyte counts include acquired and congenital (Diamond-Blackfan and Fanconi) aplastic anemias and hypothyroidism. Patients with trisomy 21 have macrocytic cells, although an accompanying anemia is generally not present. High MCV and reticulocytosis is seen in CDA I and III and in situations wherein hemolysis results in such a large outpouring of young red cells that the mean MCV is abnormally high.
Brugnara C, Oski FJ, Nathan DG. Nathan and Oski’s hematology of infancy and childhood, ed 7. Philadelphia: WB Saunders; 2009.
Calis JCJ, Phiri KS, Faragher B, et al. Severe anemia in Malawian children. N Engl J Med. 2008;358:888-898.
Greer JP, Foerster J, Lukens J, et al. Wintrobe’s clinical hematology, ed 11. Baltimore: Williams & Wilkins; 2004.
Luby SP, Kazembe PN, Redd SC, et al. Using clinical signs to diagnose anaemia in African children. WHO Bulletin OMS. 1995;73:477-482.
May J, Evans JA, Timmann C, et al. Hemoglobin variants and disease manifestations in severe falciparum malaria. JAMA. 2007;297:2220-2226.
Morris CR, Singer ST, Walters MC. Clinical hemoglobinopathies: iron, lungs and new blood. Curr Opin Hematol. 2006;13(6):407-418.
Robbins EB, Blum S. Hematologic reference values for African American children and adolescents. Am J Hematol. 2007;82:611-614.
Yurdakök K, Guner SN, Yalçin S. Validity of using pallor to detect children with mild anemia. Pediatr Int. 2008;50:232-234.