The american society of anesthesiologists closed claims project
Overview of adverse outcomes and their causes
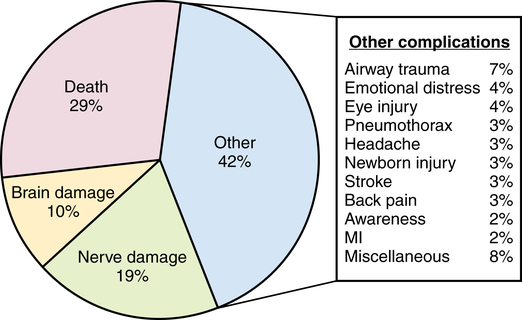
The database currently contains almost 10,000 claims. The three major adverse outcomes in the database are death (29%); nerve damage (peripheral nerve or spinal cord, 19%) or brain damage (10%); and all other complications (e.g., airway trauma, stroke, myocardial infarction), account for the remaining 42% of claims (Figure 238-1). Although various media outlets have given extensive coverage to the topic of awareness during anesthesia, awareness represents only 2% of the claims in the database and, hence, is not currently a major medicolegal risk in the United States.
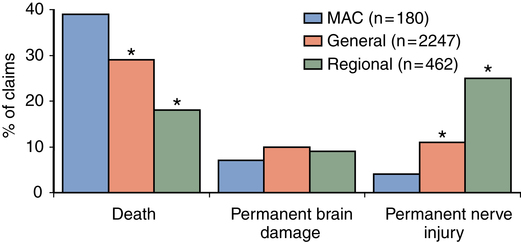
The types of complications that are listed in the database vary with the type of anesthesia used (Figure 238-2). A greater proportion of claims for death involve death occurring during monitored anesthesia care, as compared with during general or regional anesthesia. Permanent nerve injury is more often associated with the use of regional anesthesia (see Figure 238-2).
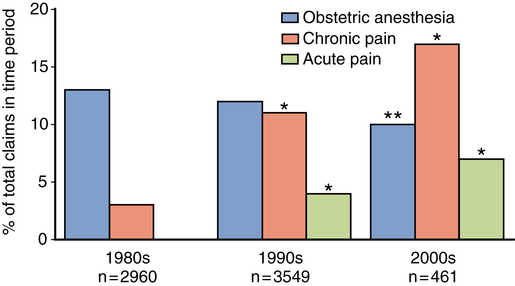
Claims associated with acute or chronic pain management have increased since the 1980s and represent more than 15% of all claims collected against anesthesiologists (Figure 238-3). The marked escalation in pain-related claims corresponds with the increasing use of acute and chronic pain therapy over the past decade. Claims associated with obstetric anesthesia make up approximately 10% of current claims (see Figure 238-3).