Chapter 62 Telescreening for Retinopathy of Prematurity
Limitations of traditional care
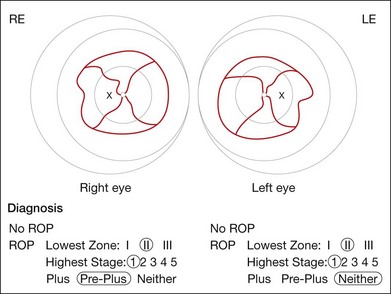
Traditional screening for retinopathy of prematurity (ROP) involves indirect ophthalmoscopy at the bedside in the neonatal intensive care unit (NICU). Although this has been effective at identifying infants with severe treatment-requiring disease,1–3 there are important limitations. Ophthalmoscopic examinations are logistically difficult, require significant travel time and coordination, and are physiologically stressful for infants.4 Findings are documented using hand-drawn sketches, which are subjective and qualitative (Fig. 62.1). In addition, there may be variability in diagnosis of critical features such as zone I and plus disease, even among experts,5,6 and there is enormous medicolegal liability. Surveys have found that the number of retinal specialists and pediatric ophthalmologists willing to manage ROP is decreasing for these reasons.7 Meanwhile, more infants are at risk for disease because of increasing premature birth rates and improved neonatal survival throughout the world.
Telemedicine as an emerging approach
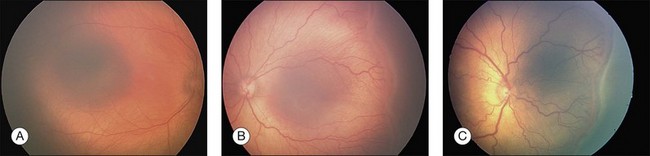
Telemedicine is an emerging approach with potential to improve the quality, delivery, and cost of care compared to traditional strategies. This may be particularly important in developing nations and other areas with limited accessibility to care. In this approach, clinical data and images are captured from the infant’s eyes by trained personnel in the NICU. Data are transmitted for review by a remote ophthalmologist, who sends management recommendations to the consulting physician. Examples of wide-angle images taken with a commercially available camera (RetCam; Clarity Medical Systems, Pleasanton, CA) are shown in Fig. 62.2. It has been shown that trained neonatal nurses can capture high-quality retinal images,8,9 and that imaging may cause less physiological stress to infants than ophthalmoscopy with scleral depression.10
In a telemedicine approach, the availability of archived retinal images would provide other advantages. Infant photographs could be directly compared to references such as the published standard photograph for plus disease,1 and may be transmitted securely to experts for second opinions. Images provide objective documentation of clinical findings, improve recognition of disease progression, enhance communication, and create infrastructure for education and research.11
Evaluation studies
Accuracy
Diagnostic accuracy of telemedicine for ROP has been evaluated since the late 1990s. Virtually all studies have used wide-angle digital images captured by a neonatal nurse, ophthalmologist, or ophthalmic photographer. Although these studies have varied in design and outcome measure, most have compared the diagnostic performance of telemedicine to a reference standard of dilated ophthalmoscopy. Schwartz et al. (19 eyes from 10 infants) examined the accuacy of telemedicine in a selected group of infants at 30–32 weeks postmenstrual age (PMA), all of whom had moderate or severe ROP. The sensitivity and specificity of telemedicine for detecting prethreshold or worse ROP were 89% and 100%, respectively.12
Since that time, research has involved larger and broader cohorts of consecutively enrolled infants. For diagnosis of any ROP regardless of severity, studies have demonstrated sensitivity of 46%–97% and specificity 49%–100% compared to a reference standard of indirect ophthalmoscopy8,13,14 (Table 62.1). Generally, lower accuracy has been found while examining infants at lower PMA, and when detecting presence of mild ROP (e.g. peripheral stage 1). This is presumably because younger infants have milder disease with more subtle diagnostic features, and because it may be technically more difficult to image smaller eyes with increased media opacities.15
Table 62.1 Diagnostic accuracy of telescreening for detection of any ROP using images captured by wide-angle camera.* Reference standard was standard indirect ophthalmoscopy
| Study | Outcome measures | Sensitivity/specificity |
|---|---|---|
| Roth et al., 200114 | Any ROP | 0.82/0.94 |
| Yen et al., 200215 | Any ROP at 32–34 wks PMA | 0.46/1.00 |
| Any ROP at 38–40 wks PMA | 0.76/1.00 | |
| Chiang et al., 200613 | Any ROP | 0.82–0.86/0.49–0.96 |
| Shah et al., 200616 | Any ROP | 0.86/0.92 |
| Chiang et al., 20078 | Any ROP at 31–33 wks PMA | 0.73–0.94/0.89–0.97 |
| Any ROP at 35–37 wks PMA | 0.91–0.97/0.98–1.00 | |
| Dhaliwal et al., 200917 | Any ROP at 34 wks PMA or 4–6 wks CA | 0.60/0.91 |
PMA, postmenstrual age; CA, chronological age.
* RetCam; Clarity Medical Systems, Pleasanton, CA.
Other studies have examined accuracy of telemedicine for detecting clinically significant ROP (Table 62.2). Ells et al. (371 exams from 36 infants) found sensitivity 100% and specificity 96% for diagnosis of “referral-warranted ROP”* during serial examinations throughout an infant’s hospital course.18 Wu et al. (serial exams from 43 infants) performed telemedicine screening for prethreshold or worse ROP, and found sensitivity 100% and specificity 98%.19 Chiang et al. (163 exams from 64 infants) reported sensitivity 72%–83% and specificity 90%–99% for detection of type 2 or worse ROP, and sensitivity 85%–90% and specificity 95%–97% for detection of treatment-requiring ROP.13 The multicenter prospective Photo-ROP Study (300 exams from 51 infants) found sensitivity 92% and specificity 37% for detection of “clinically significant ROP”† during weekly examinations throughout an infant’s hospital course.20
Table 62.2 Diagnostic accuracy of telescreening for detection of clinically significant ROP using images captured by wide-angle camera.* Reference standard was standard indirect ophthalmoscopy
| Study | Outcome measures | Sensitivity/specificity |
|---|---|---|
| Ells et al., 200318 | Any ROP zone I, presence of plus disease, or presence of any stage 3 ROP at any time during hospital course | 1.00/0.96 |
| Chiang et al., 200613 | Type 2 or worse ROP | 0.72–0.83/0.90–0.99 |
| Treatment-requiring ROP | 0.85–0.90/0.95–0.97 | |
| Wu et al., 200619 | Prethreshold or worse ROP | 1.00/0.98 |
| Chiang et al., 20078 | Type 2 or worse ROP at 31–33 wks PMA | 0.71–0.86/0.93–0.97 |
| Type 2 or worse ROP at 35–37 wks PMA | 1.00/0.85–0.94 | |
| Treatment requiring ROP at 31–33 wks PMA | NA/0.94–1.00 | |
| Treatment requiring ROP at 35–37 wks PMA | 1.00/0.81–0.94 | |
| Photo-ROP Cooperative Group, 200820 | “Clinically significant ROP” | 0.92/0.37 |
| Dhaliwal et al., 200917 | Stage 3 ROP at 34 wks PMA or 4–6 wks CA | 0.57/0.98 |
| Presence of plus disease | 0.80/0.98 | |
| Lorenz et al., 200921 | Suspected treatment-requiring ROP: threshold ROP in zone II, prethreshold in zone I, or disease possibly requiring treatment but not reliably classified from images | 1.00/NA |
| Silva et al., 20119 | Referral-warranted ROP: type 2 or worse | 1.00/0.99 |
| Dai et al., 201122 | Treatment-requiring ROP | 1.00/0.98 |
PMA, postmenstrual age; CA, chronological age; NA, not applicable.
* RetCam; Clarity Medical Systems, Pleasanton, CA. For definition of “clinically significant ROP”, see text.
In a prospective study, Chiang et al. (248 exams from 67 infants) examined the effect of PMA and disease severity on telemedicine accuracy. At 31–33 weeks PMA, the sensitivity and specificity by three expert graders was 71%–86% and 93%–97% respectively for detection of type 2 or worse ROP, and the specificity for detection of treatment-requiring ROP was 94%–100%. At 35–37 weeks PMA, sensitivity and specificity by three graders were 91%–97% and 98%–100% respectively for detection of any ROP, 100%–100% and 85%–94% respectively for detection of type 2 or worse ROP, and 100%–100% and 81%–94% respectively for detection of treatment-requiring ROP.8 The finding of higher accuracy in older infants was in agreement with previous studies.15
Dhaliwal et al. (245 exams from 81 infants) conducted a masked, double-observer prospective longitudinal cohort study. Two pediatric ophthalmologists were randomized to perform examinations using either telemedicine or ophthalmoscopy. Sensitivity of telemedicine for detecting stage 3 or worse ROP was 57%, and specificity was 98% compared to ophthalmoscopy. Sensitivity for detecting plus disease was 80%, and specificity was 98%. Absolute agreement between ophthalmoscopy and telemedicine was 96% for detection of stage 3, and 97% for detection of plus disease.17 Dai et al. (422 exams from 108 infants) conducted a study in which all infants received telemedicine imaging and ophthalmoscopy by a pediatric ophthalmologist. Images were reviewed independently by a masked grader. Using ophthalmoscopy as the reference standard, sensitivity of telemedicine for detecting treatment-requiring ROP (i.e., type 1 or worse) was 100% and specificity was 98%. The positive predictive value of telemedicine for detecting treatment-requiring ROP was 86%, and the negative predictive value was 100%.22
Scott et al. compared the accuracy of telemedicine vs ophthalmoscopy using a study design in which these two methods were performed by the same experts in 67 consecutive infants. There was substantial to near-perfect agreement between these methods, with absolute intra-grader agreement of 86% (178/206 eyes) and kappa values of 0.66–0.85 between ophthalmoscopy and telemedicine. Among the 14% (28/206 eyes) intra-expert discrepancies, some cases provided photographic evidence that ophthalmoscopy failed to recognize mild ROP that was detected by telemedicine. There were also discrepancies involving presence of zone I and plus disease, in which telemedicine may have provided theoretical advantages by allowing examiners to review their diagnoses, make more exact measurements of anatomical landmarks, and directly compare images to standard photographs.23
Image quality
Several studies have examined the quality of images captured by nurses, ophthalmic photographers, or ophthalmologists. Ells et al. found that wide-angle images were captured successfully in 96% of examinations, and that 94% of image sets could be graded remotely. In the remaining 6%, readable photographs were obtained within 1–4 weeks.18 Wu et al. found that 79% of initial retinal images and 78% of repeated images were acceptable.19 The Photo-ROP cooperative group found that 92% of image sets were acceptable.20 Chiang et al. reported that telemedicine graders reported an “unknown” diagnosis because of inadequate image quality or insufficient retinal coverage in 0%–41% of exams at 31–33 weeks PMA, and in 0%–7% of exams at 35–37 weeks PMA.8 Lorenz et al. reported that, among 6460 telemedicine imaging sessions conducted at five NICUs over a six-year period, nearly 98% were of adequate quality.21 Heavy fundus pigmentation, corneal and vitreous haze, smaller palpebral fissures, and limited dilation may be associated with decreased image quality.8,13,16,19
Cost-effectiveness, speed, and satisfaction
Economic and practical factors must be considered for long-term viability of telemedicine systems. Two studies have compared the cost-effectiveness of telemedicine versus ophthalmoscopy for ROP management using decision tree models created from published results involving disease incidence, diagnostic accuracy, and treatment outcomes. One study, performed in the United States, found that telemedicine is more cost-effective than traditional ophthalmoscopy ($3193 per quality-adjusted life year [QALY] compared to $5617/QALY).24 The second study, performed in the United Kingdom, modeled five possible strategies for ROP surveillance using telemedicine and ophthalmoscopy, and found that telemedicine using image capture and grading by visiting nurses (£175 per infant examined) and telemedicine using image capture by visiting nurses and image grading by remote ophthalmologists (£201/infant examined) were more cost-effective than traditional ophthalmoscopy at the NICU bedside (£321/infant examined).25
Other studies have examined logistical factors such as examination time and acceptability to patients. Richter et al. found that telemedicine examinations required significantly less physician time than ophthalmoscopy (1.02–1.75 minutes per telemedicine exam versus 4.17–6.63 minutes per ophthalmoscopic exam).26 Lee et al. developed and validated a survey instrument to assess attitudes toward digital imaging and telemedicine by parents, and found high acceptance of these technologies. Families did, however, report that face-to-face contact with physicians was important.27
Evaluation of operational ROP telemedicine programs
A telemedicine program involving five German NICUs has been operational since 2001. In this program, all premature infants at risk for ROP are screened with wide-angle imaging and also examined by local ophthalmologists. All suspected treatment-requiring ROP stages were detected with 100% sensitivity, and the overall positive predictive value for treatment-requiring ROP was 88.2% after 6460 examinations in 1222 infants.21
A similar program involving four NICUs, in which nurses are trained to capture serial images, has been used for routine telemedicine management at Stanford University since 2005.9 Infants felt to have referral-warranted (i.e. type 2 or worse) or treatment-requiring (i.e. type 1 or worse) ROP based on telemedicine were referred for complete ophthalmoscopic evaluation. Within one week of NICU discharge, all infants in this program received a mandatory ophthalmoscopic examination by the same retinal specialist. The sensitivity of telemedicine for identifying referral-warranted and treatment-requiring ROP was reported to be 100%, the positive predictive value of telemedicine for identifying treatment-requiring ROP was 90%, and the negative predictive value was 100%. No known cases of treatment-requiring ROP were missed, and there were no adverse outcomes such as retinal detachment.9
Barriers and challenges
Despite technological advances to support telemedicine for ROP management, its widespread adoption has been limited by factors such as medical licensure and lack of consistent insurance coverage and reimbursement policies.28 The level of diagnostic accuracy required for implementation of real-world ROP telemedicine systems is unclear, given concerns about medicolegal liability. Furthermore, it is difficult to rigorously assess accuracy because there may be variability in the reference standard of indirect ophthalmoscopy. Capturing images with sufficient diagnostic quality may not always be practical, particularly in the peripheral retinas of younger infants, warranting re-evaluation either by repeat imaging or ophthalmoscopy. Finally, implementation of telemedicine for ROP requires approval of physicians and financial investments for new equipment and information technologies.
Future directions
Telemedicine has potential benefits for ROP management, education, and research. Studies have demonstrated that it has very high accuracy for detection of clinically significant ROP, particularly in older infants. An ongoing study is examining the validity, reliability, feasibility, safety, and cost-effectiveness of an ROP telemedicine system to detect referral-warranted ROP with a multicenter design,29 and a centralized image-reading center.
Attention should be given to training protocols, and to the assignment of roles and responsibilities for neonatology and ophthalmology personnel. Rules must be defined for cases in which image quality is inadequate, and when digital imaging is impractical because of systemic illness, infection contact precautions, or other reasons. Development of image capture protocols will help standardize the process of ROP telemedicine diagnosis, analogous to what has been done in diseases such as diabetic retinopathy (Chapter 50, Telescreening for diabetic retinopathy). Reading center software, which helps optimize workflow and mitigate risk, should be easily accessible for ophthalmologists and hospitals.30 The success from several operational programs suggests that this is practical, but the maintenance of large sustainable ROP telemedicine programs will require generalizable solutions to these challenges.
1 Multicenter trial of cryotherapy for retinopathy of prematurity. Preliminary results. Cryotherapy for Retinopathy of Prematurity Cooperative Group. Pediatrics. 1988;81:697–706.
2 Early Treatment for Retinopathy of Prematurity Cooperative Group. Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol. 2003;121:1684–1694.
3 Section on Ophthalmology American Academy of Pediatrics, American Academy of Pediatrics. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2006;117:572–576. Erratum in Pediatrics 2006;118:1324
4 Laws DE, Morton C, Weindling M, et al. Systemic effects of screening for retinopathy of prematurity. Br J Ophthalmol. 1996;80:425–428.
5 Chiang MF, Jiang L, Gelman R, et al. Interexpert agreement of plus disease diagnosis in retinopathy of prematurity diagnosis. Arch Ophthalmol. 2007;125:875–880.
6 Chiang MF, Thyparampil PJ, Rabinowitz D. Interexpert agreement in identification of macular location in infants at risk for retinopathy of prematurity. Arch Ophthalmol. 2010;128:1153–1159.
7 Ocular Surgery News U.S. Edition [Internet]. Survey: Physicians being driven away from ROP treatment. http://www.osnsupersite.com/view/asp?rID=18018, 2006. [cited 2010 Nov 1]
8 Chiang MF, Wang L, Busuioc M, et al. Telemedical retinopathy of prematurity diagnosis: accuracy, reliability, and image quality. Arch Ophthalmol. 2007;125:1531–1538.
9 Silva RA, Murakami Y, Lad EM, et al. Stanford University network for diagnosis of retinopathy of prematurity (SUNDROP): 36-month experience with telemedicine screening. Ophthalmic Surg Lasers Imaging. 2011;42:12–19.
10 Mukherjee AN, Watts P, Al-Madfai H, et al. Impact of retinopathy of prematurity screening examination on cardiorespiratory indices: a comparison of indirect ophthalmoscopy and RetCam imaging. Ophthalmology. 2006;113:1547–1552.
11 Chiang MF, Gelman R, Martinez-Perez ME, et al. Image analysis for retinopathy of prematurity diagnosis. J AAPOS. 2009;13:438–445.
12 Schwartz SD, Harrison SA, Ferrone PJ, et al. Telemedical evaluation and management of retinopathy of prematurity using a fiberoptic digital fundus camera. Ophthalmology. 2000;107:25–28.
13 Chiang MF, Keenan JD, Starren J, et al. Accuracy and reliability of remote retinopathy of prematurity diagnosis. Arch Ophthalmol. 2006;124:322–327.
14 Roth DB, Morales D, Feuer WJ, et al. Screening for retinopathy of prematurity employing the RetCam 120: sensitivity and specificity. Arch Ophthalmol. 2001;119:268–272.
15 Yen KG, Hess D, Burke B, et al. Telephotoscreening to detect retinopathy of prematurity: preliminary study of the optimum time to employ digital fundus camera imaging to detect ROP. J AAPOS. 2002;6:64–70.
16 Shah PK, Narendran V, Saravanan VR, et al. Screening for retinopathy of prematurity: a comparison between binocular indirect ophthalmoscopy and RetCam 120. Indian J Ophthalmol. 2006;54:35–38.
17 Dhaliwal C, Wright E, Graham C, et al. Wide-field digital retinal imaging versus binocular indirect ophthalmoscopy for retinopathy of prematurity screening: a two-observer prospective, randomised comparison. Br J Ophthalmol. 2009;93:355–359.
18 Ells AL, Holmes JM, Astle WF, et al. Telemedicine approach to screening for severe retinopathy of prematurity: a pilot study. Ophthalmology. 2003;110:2113–2117.
19 Wu C, Petersen RA, VanderVeen DK. RetCam imaging for retinopathy of prematurity screening. J AAPOS. 2006;10:107–111.
20 Photographic Screening for Retinopathy of Prematurity (PHOTO-ROP) Cooperative Group. The photographic screening for retinopathy of prematurity study (PHOTO-ROP): primary outcomes. Retina. 2008;28:S47–S54.
21 Lorenz B, Spasovska K, Elflein H, et al. Wide-field digital imaging based telemedicine for screening for acute retinopathy of prematurity (ROP). Six-year results of a multicentre field study. Graefes Arch Clin Exp Ophthalmol. 2009;247:1251–1262.
22 Dai S, Chow K, Vincent A. Efficacy of wide-field digital retinal imaging for retinopathy of prematurity screening. Clin Experiment Ophthalmol. 2011;39:23–29.
23 Scott KA, Kim DY, Wang L, et al. Telemedical diagnosis of retinopathy of prematurity: intraphysician and agreement between ophthalmoscopic examination and image-based interpretation. Ophthalmology. 2008;115:1222–1228.
24 Jackson KM, Scott KE, Graff-Zivin J, et al. Cost-utility analysis of telemedicine and ophthalmoscopy for retinopathy of prematurity management. Arch Ophthalmol. 2008;126:493–499.
25 Castillo-Riquelme MC, Lord J, Moseley MJ, et al. Cost-effectiveness of digital photographic screening for retinopathy of prematurity in the United Kingdom. Int J Technol Assess Health Care. 2004;20:201–213.
26 Richter GM, Sun G, Lee TC, et al. Speed of telemedicine vs ophthalmoscopy for retinopathy of prematurity diagnosis. Am J Ophthalmol. 2009;148:136–142.
27 Lee JY, Du YE, Coki O, et al. Parental perceptions toward digital imaging and telemedicine for retinopathy of prematurity management. Graefes Arch Clin Exp Ophthalmol. 2010;248:141–147.
28 Grigsby J, Sanders JH. Telemedicine: where it is and where it’s going. Ann Intern Med. 1998;129:123–127.
29 ClinicalTrials.gov [Internet]. US National Institutes of Health. Telemedicine approaches to evaluating acute-phase ROP. Available from http://clinicaltrials.gov/ct2/show/NCT01264276, 2011. [cited 2011 June 28]
30 Focus-ROP Remote Disease Management [Internet]. Cast a wide safety net for retinopathy of prematurity (ROP). Available from http://www.focusrop.com/, 2011. [reviewed 2011 Jan 12; cited 2011 May 6]
* “Referral-warranted ROP” was defined as any ROP in zone I, plus disease, or stage 3 ROP.
† Clinically significant ROP was defined as: (a) zone 1, any ROP, without vascular dilation or tortuosity; (b) zone II, stage 2, with up to one quadrant of vascular dilation and tortuosity; (c) zone II, stage 3, with up to one quadrant of vascular dilation and tortuosity; (d) any vascular dilation and tortuosity noted in eyes for which ridge characteristics were not interpretable (not imaged or poor image quality); or (e) any ROP noted in eyes for which disc features (plus disease) were not interpretable (not imaged or poor image quality).