21 Tai Chi, Qi Gong, and Other Complementary Alternative Therapies for Treatment of the Aging Spine and Chronic Pain
KEY POINTS
Tai Chi
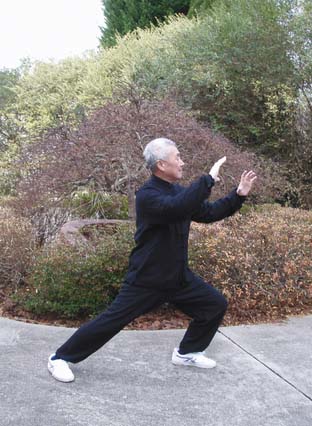
There are five main styles of Tai Chi: Chen, Yang, Wu (or Hao), Wu, and Sun. Although each style has different speeds and forms of movements, practicing any style of Tai Chi requires similar fundamentals, including (1) concentration with internal stillness and quick reaction time, (2) deep breathing skills to enhance its aerobic component, (3) strong leg support and good balance for constant body weight shifting during movements, (4) correct posture and spine alignment with relaxed muscles to maintain stability without unnecessary muscle tension, and (5) an agile torso (lumbar spine) with coordination among all body parts to perform the movements gracefully. Masters of Tai Chi build up internal energy that gives them not only the power needed during combat, but also health and longevity. The latter is the main reason why Tai Chi is widespread in the world, with many participants being attracted to it not for its combative content but for its health benefits. When it is performed for health reasons, the movements can be slow and deliberate with low exercise impact and, therefore, can be tolerated well by the elderly (Figure 21-1).
Even with simplified Tai Chi exercises, studies have demonstrated improvement in balance, reduced fear of falling, and decreased risk of falls in older adults.1 Tai Chi, like other forms of exercise, can also reduce blood pressure, improve heart failure, normalize blood lipids and glucose levels,2 and positively affect bone mineral density in postmenopausal women.3 In the older population, when compared to age and body size-matched sedentary controls, Tai Chi practitioners have higher oxygen uptake, greater flexibility, and a lower percentage of body fat.4
From Qi Gong to Energy-Based Therapies
Besides Qi Gong, other main types of energy-based therapies include Reiki (Japanese), Breema (American), and therapeutic touch (American). Some of these are critically questioned by the research community. For instance, in therapeutic touch, practitioners with their hands placed several inches to feet away from a patient claim that they can feel the energy field emanated by a human body and detect certain patterns of disruption; however, in one clinical investigation, they could correctly detect only 44% of the time (less than chance) the position of a child’s hand.5 Although this illustrates certain doubts on energy-based therapies for their bioenergy base, we are not rejecting their clinical effects as the possible effects may be achieved in other ways.
Mind-Body Therapies
Mindfulness Meditation
The mindfulness-based stress reduction (MBSR) program was developed at the University of Massachusetts Medical Center. Mindfulness meditation has three purposes: knowing the mind, training the mind, and freeing the mind. It calls for awareness of conscious and unconscious thoughts, feelings, and behaviors that underlie emotional, physical, and spiritual health, and cultivates greater awareness of one’s own bodily functions for the unity of mind and body. The mind is known to be a factor in stress and stress-related disorders. In mindfulness meditation, patients learn to distinguish between mind and awareness, learn to see how the mind dwells on anxiety and fear that burns up energy, learn to stay in the present moment while experiencing high levels of pain, and learn to distinguish between pain sensations and the mind’s creation of the experience of suffering. The practice thus brings nonjudgmental moment-to-moment awareness to thoughts, sensations, or emotions as they arise.
In one qualitative study, 27 older adults with chronic low back pain participated in a MSBR program.6 The authors found a report of improved attention, improved quality of sleep, and improved quality of life along with reduction in pain. In another randomized controlled study of 37 older adults with chronic pain, subjects were randomized into MSBR or wait-list control groups. MSBR participants were found to have improvement in pain acceptance, activity engagement, and physical functioning after 6 months.7 Both studies showed that MSBR was feasible and effective in the older adult population with spine conditions and chronic pain.
Guided Imagery
There have been few studies on guided imagery in older subjects with pain. Morone and Greco8 reviewed two studies that were done over a short period of time with small numbers of subjects. Both found that guided imagery was feasible in older adults using the techniques at home, without difficulty and with good compliance, and the practice reduced pain and increased mobility in these subjects.
Spirituality and Religiousness
The role of spirituality and religiousness in health, viewed from a scientific perspective, has been yielding interesting, perhaps intriguing, results. In general, studies have reported fairly consistent positive relationships with physical health, mental health, and substance abuse outcomes, mostly using cross-sectional or prospective designs.9 There were few studies found in the literature regarding spirituality/religiousness in older patients with nonmalignant chronic pain. Baetz and Bowen10 polled 37,000 Canadians and found that those who reported stronger religious beliefs had fewer reports of pain and increased reports of psychological well being. Of those with chronic pain, those who reported more religious and/or spiritual beliefs were more likely to use positive coping mechanisms including attitudinal and activity strategies, and reported increased control and self-efficacy, which led to an increase in pain tolerance. They were also more likely to exercise.
Basic Science
Attention and Pain
Chronic pain is associated with impairment of attentional processes. Attention can be thought of as the preferential processing of various types of cognitive information. The function of attention is the appropriate selection of stimuli, maintenance of concentration, and interactions with space and time.11 The anterior cingulate cortex (ACC) is needed for sustained attention, because it modulates one’s ability to concentrate over time by coordinating and integrating task-specific processes. The ACC has a pivotal role in executive processes, motivation, allocation of attentional resources, premotor functions, and error detection. It is activated by moderate-to-intense painful stimulation, and positron emission tomography studies have revealed a large concentration of opiate receptors in this region.12 The more intense and the longer the duration of painful stimuli, the more active the ACC becomes.
Pain may interrupt complex cognition and capture attention that might otherwise be allocated elsewhere; chronic pain may result in a person sustaining focus on the pain rather than other stimuli. Various studies have shown that persons reporting greater attention to pain also report higher pain intensity; persons engaging in attention-demanding tasks report lower pain intensity. Directing attention away from the pain decreases the perception of pain; this distraction away from pain decreases activity in the ACC, insular cortex, thalamus, and somatosensory regions.12–14
Another area of interest is the periaqueductal gray (PAG), which receives major inputs from the frontal cortex, hypothalamus, frontal granular, insular cortex, and amygdala. The PAG projects to the rostral ventromedial medulla, which in turn sends projections to pain-transmitting neurons in the dorsal horn of the spinal cord and the trigeminal nucleus caudalis.15 Within this complex neuronetwork, PAG plays an important role in the descending modulation of pain and in defensive behavior. A study using functional MRI assessed changes in the PAG region in normal subjects.15 Noxious and warm thermal stimuli were applied to the subjects, who were told whether or not to attend to pain. Increased activity within the PAG correlated with perceptual decreases in pain intensity; a greater change in PAG activity was found with a larger decrease in reported pain intensity. Activation difference in the PAG significantly correlated with the total pain score change, using visual analogue scale (VAS), between conditions; a greater change in PAG activity was found with a larger decrease in reported pain intensity. Increased activity within the PAG correlated with perceptual decreases in pain intensity.
Regulation of the Autonomic Nervous System
Tai Chi, Qi Gong, and other energy-based therapies, as well as mind-body interaction, all claim to be able to lower blood pressure, provide a sense of relaxation and serenity, improve sleep, strengthen the immune system, and improve pain, physical activities, and quality of life. These can be viewed as positive effects on a range of autonomic physiological processes, confirmed by research studies that examined Tai Chi and mind-body interactions.16,17 The aforementioned neuronetwork, i.e., ACC and PAG, has also been found to modulate autonomic function.18,19 Therefore, future mechanistic research may help further understand the interplay among the central, peripheral, and autonomic nervous systems with the resultant clinical effects from these holistic therapies.
Case Discussion
Tai Chi is an exercise that is considered to be holistic because it integrates mind concentration with a high level of internal engagement and external movements. However, it is not the only exercise that should be considered holistic. In fact, any exercise, sport, or activity that requires such integration of mind and body would produce similar effects. The selection of the type lies in the provider’s experience and the patient’s preference. For instance, if the patient preferred to learn dancing, which also requires concentration, graceful posture, and poised movements, the clinical effects might be as significant as seen with Tai Chi.
Even with the improvements achieved by Tai Chi exercises, treatment of depression also played an important role in clinical progress. The contribution of depression to pain is often not recognized by patients. Depression can worsen pain symptoms, and effective treatment of depression can improve chronic pain.20 Active treatments and socialization are extremely important for treatment of depression as well as pain, to break the cycle of pain and depression. The socialization at the Tai Chi classes, along with pain group therapy that introduced chronic pain coping strategies that diverted the patient’s attention from pain to more positive images of his own health and condition, all contributed to his improvements in this clinical case.
The impact of sleep in chronic pain management has been often underestimated even by pain specialists. However, there are strong correlations between chronic pain and sleep difficulties.21 Education on sleep hygiene and the use of relaxation techniques helped improve this patient’s sleep, which contributed to decreased pain at morning time. Improved pain and function further provided improved sleep at night.
Conclusion
The holistic concept has been the focus and attraction of most complementary alternative therapies that have demonstrated their clinical effects in the aging spine and chronic pain. Their promising clinical effects have earned their place in a comprehensive clinical management program as an integral part of reducing pain and improving function. Complementary and alternative medical practices can be blended with traditional evidence-based medicine to optimally promote a healing environment and overall patient well-being.22 Their underlying mechanisms prompt further investigation; however, use of the simple pharmacological model must be avoided due to their complicated involvement of multiple aspects of healing, such as active exercises, concentration, mind-body interaction, attention modification, and autonomic regulation.
1. Taggart H.M. Effects of Tai Chi exercise on balance, functional mobility, and fear of falling among older women. Appl. Nurs. Res.. 2002;15(4):235-242.
2. Yeh G.Y., Wang C., Wayne P.M., et al. Tai chi exercise for patients with cardiovascular conditions and risk factors: a systematic review. J. Mol. Signal.. 2009;29(3):152-160.
3. Wayne P.M., Kiel D.P., Krebs D.E., et al. The effects of Tai Chi on bone mineral density in postmenopausal women: a systematic review. Arch. Phys. Med. Rehabil.. 2007;88(5):673-680.
4. Lan C., Lai J.S., Wong M.K., et al. Cardiorespiratory function, flexibility, and body composition among geriatric Tai Chi Chuan practitioners. Arch. Phys. Med. Rehabil.. 1996;77(6):612-616.
5. Rosa L., Rosa E., Sarner L., et al. A close look at therapeutic touch. JAMA. 1998;279(13):1005-1010.
6. Morone N.E., Lynch C.S., Greco C.M., et al. “I felt like a new person.” The effects of mindfulness meditation on older adults with chronic pain: qualitative narrative analysis of diary entries. J. Pain. 2008;9:841-848.
7. Morone N.E., Greco C.M., Weiner D.K. Mindfulness meditation for the treatment of chronic low back pain in older adults: a randomized controlled pilot study. Pain. 2008;134:310-319.
8. Morone N.E., Greco C.M. Mind-body interventions for chronic pain in older adults: a structured review. Pain Med.. 2007;8:359-375.
9. Thoresen C.E. Spirituality and health. J. Health Psych.. 1999;4:291-300.
10. Baetz M., Bowen R. Chronic pain and fatigue: associations with religion and spirituality. Pain Res. Manage.. 2008;13:383-388.
11. Gitelman D.R. Attention and its disorders. BriMed. Bulletin. 2003;65:21-34.
12. Bantick S.J., Wise R.G., Ploghaus A., et al. Imaging how attention modulates pain in humans using functional MRI. Brain. 2002;125:310-319.
13. Petrovic P., Petersson K.M., Ghatan P.H., et al. Pain-related cerebral activation is altered by a distracting cognitive task. Pain. 2000;85:19-30.
14. Longe S.E., Wise R., Bantick S., et al. Counter-stimulatory effects on pain perception and processing are significantly altered by attention: An fMRI study. Neuroreport. 2001;12:2021-2025.
15. Tracey I., Ploghaus A., Gati J.S., et al. Imaging attentional modulation of pain in the periaqueductal gray in humans. J. Neurosci.. 2002;22:2748-2752.
16. Lu W.A., Kuo C.D. The effect of Tai Chi Chuan on the autonomic nervous modulation in older persons. Med. Sci. Sports Exercise. 2003;35(12):1972-1976.
17. Critchley H.D. Psychophysiology of neural, cognitive and affective integration: fMRI and autonomic indicants. Int J. Psychophysiol.. 2009;73(2):88-94.
18. Tang Y.Y., Ma Y., Fan Y., et al. Central and autonomic nervous system interaction is altered by short-term meditation. Proc. Natl. Acad. Sci. U.S.A.. 2009;106(22):8865-8870.
19. Bandler R., Keay K.A., Floyd N., et al. Central circuits mediating patterned autonomic activity during active vs. passive emotional coping. Brain Res. Bull.. 2000;53(1):95-104.
20. Lunde L.H., Nordhus I.H., Pallesen S., et al. The effectiveness of cognitive and behavioural treatment of chronic pain in the elderly: a quantitative review. J. Clin. Psychol. Med. Settings. 2009;16(3):254-262.
21. Stiefel F., Stagno D. Management of insomnia in patients with chronic pain conditions. CNS Drugs. 2004;18(5):285-296.
22. Geimer-Flanders J. Creating a healing environment: rationale and research overview. Cleve, Clin. J. Med.. 2009;76(Suppl. 2):S66-S69.