Chapter 28 Syringomyelia
• The presence of syringomyelia requires lifelong neurological follow-up with repeat magnetic resonance imaging scans.
• When a patient with Chiari I or Chiari II malformation, with hydrocephalus and syringomyelia, has deteriorated radiologically, the shunt should be investigated first before any treatment for syringomyelia is considered.
• Chiari I patients with syringomyelia require decompression of the cerebrospinal fluid (CSF) obstruction at the craniovertebral junction.
• Treatment of syringomyelia caused by trauma requires decompression of the CSF at the level of the deformity or block followed by spinal stabilization, when clinically indicated. Treatment with a syringosubarachnoid or syringopleural shunt may stop the progression of the syrinx and neurological deterioration but the long-term prognosis remains guarded.
• Chiari II malformation is very different from that of Chiari I with respect to syringomyelia management.
The condition, syringomyelia, was described in 1876 by Leyden1 and in 1891 by Abbe and Coley.2 Although several theories had been proposed in the 1960s and 1970s on the pathophysiology surrounding the formation and propagation of syringomyelia, the real progress came after the advent of magnetic resonance imaging (MRI) in the past decade, which facilitated noninvasive high-definition imaging of the condition, and later with the development of dynamic in vivo imaging of CSF movement.
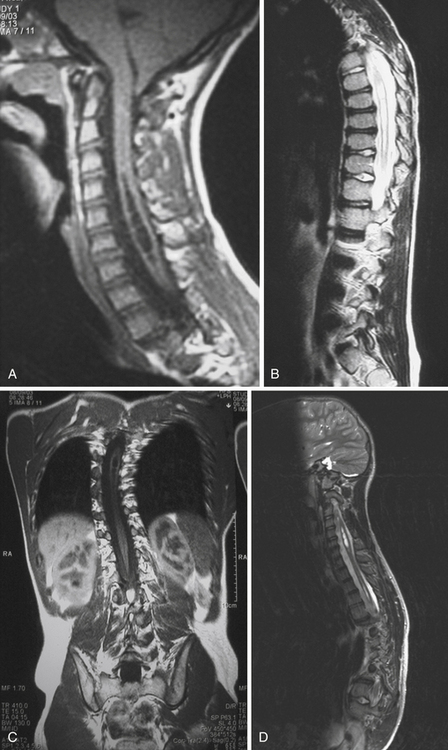
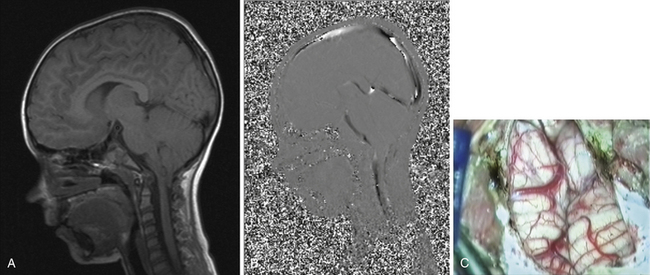
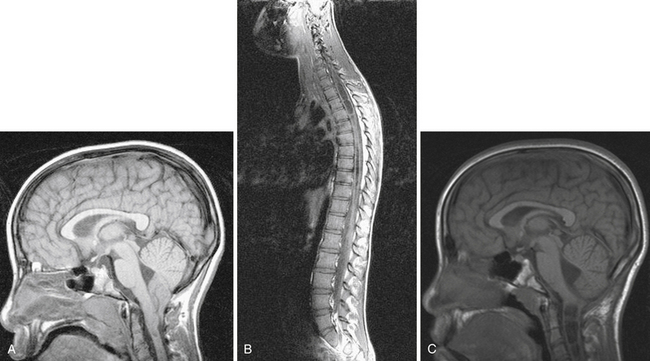
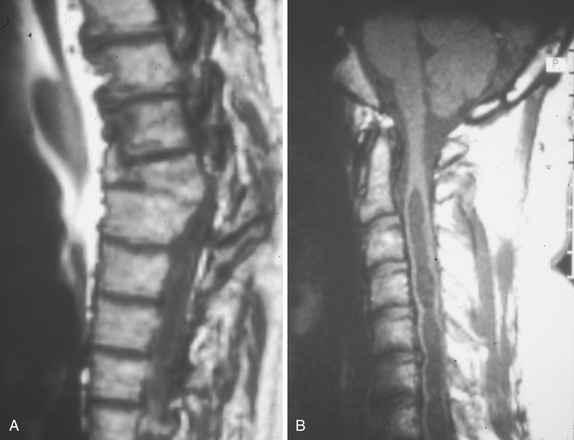
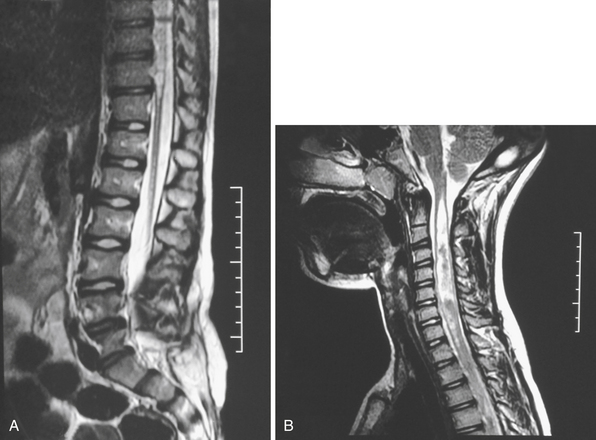
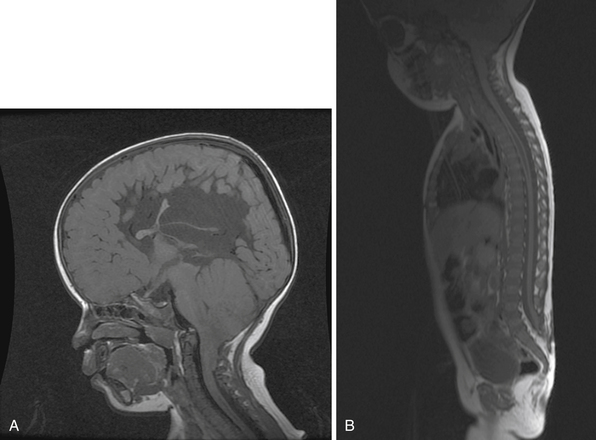
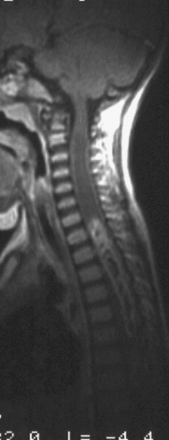
Syringomyelia is most frequently associated with hindbrain herniation. Hindbrain herniation, or Chiari I malformation, is the herniation of the cerebellar tonsils for 5 mm or more beyond the foramen magnum below a line connecting the basion and opisthion (Figs. 28.1 to 28.3). In large clinical series 50% to 80% of patients with symptomatic Chiari I malformation (CMI) have syringomyelia. However, because these series contained only symptomatic patients it is difficult to know the precise incidence of syringomyelia among all patients with Chiari I malformation. It is unclear also if syringomyelia represents an evolutionary stage in the natural history of the Chiari I malformation or it starts ab initio, from the beginning of the creation of the malformation. In most patients, Chiari I malformation is regarded as congenital. It is unclear if the malformation changes with time, if the cerebellar herniation increases. Certainly, from studies in asymptomatic patients and from the author’s unpublished experience of following over 20 asymptomatic children for many years with yearly MRI scans, in most patients the cerebellar herniation does not increase with time.3,4 Very few occasions of spontaneous resolution of Chiari I malformation have been reported.5 On the other hand, syringomyelia frequently changes with time. Acquired Chiari I malformation can develop following lumbar shunt placement or failure of a ventricular shunt, if the hindbrain is pulled down through the foramen magnum.6,7 Syringomyelia may be associated also with various other conditions such as spinal arachnoid cysts; traumatic paraplegia (Fig. 28.4); postinfectious, postinflammatory, or tuberculous meningitis; chemical insults following use of intrathecal agents, antibiotics, or myelographic contrast agent Myodil-Pantopaque; epidural abscess; Pott’s disease; and idiopathic meningeal fibrosis. In addition, various forms of spinal dysraphism such as spinal lipoma (Fig. 28.5), diastematomyelia (Fig. 28.6), recurrent tethering after myelomeningocele repair (Fig. 28.7), thickened filum terminale, rare malformations affecting the foramen magnum region such as achondroplasia, posterior fossa arachnoid cysts, Chiari II malformation, syndromic craniosynostosis, osteogenesis imperfecta, mucopolysaccharidosis, and spinal cord tumors can also be associated with syringomyelia (Fig. 28.8).
Syringomyelia affects commonly the cervical and upper thoracic spinal cord, although it can extend throughout the entire spinal cord, creating a holocord syringomyelia (see Figs. 28.3B and 28.5). If untreated, it follows a progressive and often relentless course over a number of years. Usually the neurological deterioration is gradual, but sudden deterioration has been described. The neurological function of arms and legs is at risk and patients in whom, despite treatment, the syringomyelia cavity continues to extend end up quadriplegic. The cavity may extend both proximally and distally and the tension of the fluid inside it continues to increase. Longstanding syringomyelia provokes gliosis formation in the cavity walls and the surrounding cord. Gliosis formation has been seen in postmortem examinations, in which the cavity walls are seen to be clearly lined by gliotic tissue.8 A drain inserted in the syringomyelia cavity may be encased by gliotic tissue.8 Even though surgical treatment may lead to radiological collapse of the syringomyelia cavity, sometimes this is not associated with clinical improvement. Gliosis inside the cord may lead to progressive neurological loss even after successful surgery and collapse of the cavity.9 The syringomyelia cavity can reach the upper cervical cord and medulla, becoming syringobulbia (Fig. 28.3C); it may cause deterioration of neurological function in the arms and eventually affect the function of the lower brainstem, producing bulbar palsy, respiratory failure, and death.
Epidemiology
The incidence of Chiari I malformation in the general population is estimated at 7%, but not all subjects are symptomatic. The increasing use of MRI scanning in the investigation of headaches has led to an increase in the incidence of this diagnosis. It is unclear, though, what percentage of patients with radiological evidence of Chiari I malformation have symptoms attributable to it. Syringomyelia has a prevalence of 8.4 cases per 100,000 population. It is estimated that in the United States, 21,000 Americans suffer from syringomyelia. More accurately, the figure is likely to be considerably higher, as even today, despite the wide availability of MRI scanning, the condition is underdiagnosed. The incidence of post-traumatic syringomyelia is around 1% to 3% of cases of paraplegia with a male predominance and relatively young age, and parallel to the incidence or trauma for age and gender.10–12 Why so few patients develop syringomyelia following spinal cord injury is not known. The average time between spinal injury and symptomatic presentation is 7 years (range: 3 months to 30 years). Post-traumatic syringomyelia is rare in children.
Pathophysiology of Syringomyelia
The mechanism of formation of syringomyelia has not been adequately explained yet. Most of the studies that attempt to explain the development of syringomyelia focus on the model of hindbrain hernia in Chiari I malformation. In experimental studies, dye injected in the spinal subarachnoid space has been found in the central canal, believed to have traveled there along the Virchow-Robin spaces beside the vessels of the cord. It is unclear when and how the creation of the cavity commences.13 There are reports of a presyringomyelia state seen in MRI scans of patients with Chiari I malformation, with upper cervical spinal cord swelling, which subsequently developed into syringomyelia.14–16 These reports are very few, in contrast to the very high numbers of patients with established syringomyelia that have been reported and are seen in clinical practice. This by implication may signify that the presence of a presyringomyelia state may be the exception rather than the rule. Several theories have been proposed on the formation and propagation of syringomyelia. The most notable ones, in chronological order, are Gardner’s hydrodynamic theory, Williams’ theory of “pressure dissociation,” and Oldfield’s theory of increased subarachnoid CSF pressure wave:
 In the 1960s Gardner observed that in patients with hindbrain hernia the foramen of Magendie was partially obstructed by a membrane. He believed that fluid entered the central canal in the obex at the floor of the fourth ventricle due to the “water hammer” effect of the arterial pulsations on CSF flow. Fluid accumulated inside the central canal creating the syringomyelia cavity—communicating syringomyelia or hydromyelia.17,18 This led to the surgical concept of obex plugging, where a piece of muscle or cotton wool was used to plug the obex. Syringomyelia not communicating with the central canal was called noncommunicating. MRI studies have shown that in the majority of the patients there is no direct communication between the obex and the syringomyelia cavity. Cardiac gated cine phase contrast MRI (cine PC-MRI) studies have shown that during systole the syrinx cavity contracts, whereas if Gardner’s theory was correct it should expand under the force of inflowing CSF. Gardner’s theory is regarded as imperfect and the term communicating syringomyelia has been used with less frequency. The technique of obex plugging has fallen out of favor, if for no other reason than the material used to plug the obex caused significant arachnoid fibrosis and adhesions, with subsequent recurrence of the syringomyelia.
In the 1960s Gardner observed that in patients with hindbrain hernia the foramen of Magendie was partially obstructed by a membrane. He believed that fluid entered the central canal in the obex at the floor of the fourth ventricle due to the “water hammer” effect of the arterial pulsations on CSF flow. Fluid accumulated inside the central canal creating the syringomyelia cavity—communicating syringomyelia or hydromyelia.17,18 This led to the surgical concept of obex plugging, where a piece of muscle or cotton wool was used to plug the obex. Syringomyelia not communicating with the central canal was called noncommunicating. MRI studies have shown that in the majority of the patients there is no direct communication between the obex and the syringomyelia cavity. Cardiac gated cine phase contrast MRI (cine PC-MRI) studies have shown that during systole the syrinx cavity contracts, whereas if Gardner’s theory was correct it should expand under the force of inflowing CSF. Gardner’s theory is regarded as imperfect and the term communicating syringomyelia has been used with less frequency. The technique of obex plugging has fallen out of favor, if for no other reason than the material used to plug the obex caused significant arachnoid fibrosis and adhesions, with subsequent recurrence of the syringomyelia.
 In the early 1980s Williams described the concept of “pressure dissociation” between the subarachnoid CSF spaces of the head and the spine secondary to the block of hindbrain hernia, based on in vivo CSF pressure measurements and in vitro biomechanical studies, which he performed.19 Every time a Valsalva maneuver takes place (e.g., coughing) the pressure from the chest and abdomen is transmitted to the spinal canal through the valveless venous plexus around the vertebral bodies. Normally, pressures are equalized within the spine rapidly. In the presence of a partial subarachnoid block, fluid is forced upward past the block more efficiently than it can run down again. This leads to a collapsed theca below the block, which exerts a suction effect on the spinal cord (the “suck” mechanism). Fluid that has entered the cord cavity can extend the cavity (the “slosh” mechanism).9,20,21 Williams’ theories were partly verified by MRI scan observations, and Williams’ demonstrations of his “suck and slosh” theory with models were impressive. Using cine PC-MRI it has been shown that in the presence of hindbrain hernia CSF movement in the region of the foramen magnum differs between systole and diastole. However, Williams’ observations of pressure differential were not confirmed by other studies of intraoperative CSF pressure measurements.22 It is possible that the sitting position he used to obtain his readings contributed to exaggerated cranial-spinal pressure difference readings, owing to CSF leakage from the site of the spinal measuring needle.
In the early 1980s Williams described the concept of “pressure dissociation” between the subarachnoid CSF spaces of the head and the spine secondary to the block of hindbrain hernia, based on in vivo CSF pressure measurements and in vitro biomechanical studies, which he performed.19 Every time a Valsalva maneuver takes place (e.g., coughing) the pressure from the chest and abdomen is transmitted to the spinal canal through the valveless venous plexus around the vertebral bodies. Normally, pressures are equalized within the spine rapidly. In the presence of a partial subarachnoid block, fluid is forced upward past the block more efficiently than it can run down again. This leads to a collapsed theca below the block, which exerts a suction effect on the spinal cord (the “suck” mechanism). Fluid that has entered the cord cavity can extend the cavity (the “slosh” mechanism).9,20,21 Williams’ theories were partly verified by MRI scan observations, and Williams’ demonstrations of his “suck and slosh” theory with models were impressive. Using cine PC-MRI it has been shown that in the presence of hindbrain hernia CSF movement in the region of the foramen magnum differs between systole and diastole. However, Williams’ observations of pressure differential were not confirmed by other studies of intraoperative CSF pressure measurements.22 It is possible that the sitting position he used to obtain his readings contributed to exaggerated cranial-spinal pressure difference readings, owing to CSF leakage from the site of the spinal measuring needle.
 Using preoperative PC-MRI scanning and intraoperative CSF pressure measurements in patients with syringomyelia and Chiari I malformation, Oldfield’s group observed that CSF velocity was increased at the foramen magnum but CSF flow was decreased. Cervical subarachnoid CSF pressure was increased, spinal CSF compliance was decreased, and syrinx CSF flowed caudally during systole and cranially during diastole.22,23 They surmised that the prolapsed cerebellar tonsils act like a piston, partially occluding the subarachnoid space, and create a state of increased subarachnoid pressure waves, which compress the spinal cord from without and force CSF into the syrinx cavity and propagate it with each heartbeat.
Using preoperative PC-MRI scanning and intraoperative CSF pressure measurements in patients with syringomyelia and Chiari I malformation, Oldfield’s group observed that CSF velocity was increased at the foramen magnum but CSF flow was decreased. Cervical subarachnoid CSF pressure was increased, spinal CSF compliance was decreased, and syrinx CSF flowed caudally during systole and cranially during diastole.22,23 They surmised that the prolapsed cerebellar tonsils act like a piston, partially occluding the subarachnoid space, and create a state of increased subarachnoid pressure waves, which compress the spinal cord from without and force CSF into the syrinx cavity and propagate it with each heartbeat.
All these theories do not explain precisely how and where CSF enters the cord and the mechanism of formation of septations inside the syringomyelia cavity. In the past decade, research with in vitro computer simulations using parameters gained from MRI has focused on the hydrodynamic properties of CSF, how they are altered in the presence of a subarachnoid block, and how the spinal cord viscoelastic properties relate to these changes.24–31 It is hoped that as our noninvasive imaging of CSF flow evolves, more insights will be gained on the formation and propagation of syringomyelia.
In patients who suffer spinal cord trauma, cord contusion leads to edema, blood effusion, and subsequent cord liquefaction during the first few months after injury in up to 50% of patients. Subsequently, cavity formation results and may be referred to as the primary cyst.32–34 Commonly, the cyst at the site of the injury is separated from the syringomyelia cavity by an intact septum. The syringomyelia cavity may decompress above and below the injury site following treatment, but the primary cysts may remain unchanged.35,36 As the acute injury settles, inflammation is followed by adhesions in the subarachnoid space and gliosis in the cord. Obstruction of the CSF pathways may be compounded by narrowing of the bony spinal canal from the spinal fracture. Fluid may enter the cord at the fracture site, which is often thin-walled.
Posterior Fossa Volume
The pathophysiology of syringomyelia and Chiari I malformation is often studied together, as the latter is the most common coexisting pathological condition with the former. The theory that a small posterior fossa is implicated in the cause of hindbrain hernia has been pursued for many years. It is a very obvious suggestion, as it is unlikely that Chiari I patients have “excess” cerebellar tissue compared to normal control subjects. It follows logically that some patients may have a smaller posterior fossa, which is unable to accommodate the normal volume of cerebellum. Early two-dimensional studies on lateral skull radiographs demonstrated that the height or the area of the posterior fossa is small in patients with Chiari I malformation.37,38 Recent studies used advanced image analysis techniques to calculate posterior fossa volume in computed tomography (CT) or MRI scans.39–41 The researchers conclude that the posterior fossa is smaller than normal in patients with Chiari I malformation due to presumed maldevelopment of the occipital enchondrium. This finding supports to a large extent the widespread philosophy of surgical treatment of hindbrain hernia with craniovertebral decompression to provide the cerebellum with more room, that has evolved in the past two decades.
Careful appraisal of all these studies demonstrates that none has separated patients with Chiari I according to the presence of syringomyelia. In fact, in most studies the patients with syringomyelia form the majority of the sample. A study that focused on the pediatric age group demonstrated that patients with Chiari I alone have posterior fossa of normal volume, whereas patients with Chiari I and syringomyelia have posterior fossa volume significantly smaller than normal.42 The difference in posterior fossa volume ratio according to the presence of syringomyelia was more pronounced in children who presented before the age of 10 years and smaller in those presenting after the age of 10 years. After the age of 10 years there is no significant change in the growth of the cranium overall, and little change in the growth of the skull base.43 These findings challenge the view that the development of syringomyelia represents an evolutionary stage of the Chiari I malformation. From personal observations, although new development of syringomyelia can be seen after craniovertebral decompression as a result of arachnoiditis, in patients who did not have syringomyelia at presentation, such development has not been seen in nonoperated patients with Chiari I malformation alone. Currently, there are no sizeable reports in the literature of patients with nonoperated Chiari I malformation, who have been followed for a very long time, to clearly define the risk of developing new syringomyelia. On the other hand, the phenomenon of acquired Chiari I malformation in different circumstances (e.g., following lumbar or ventricular shunting) is well recognized.6,7
There is increasing evidence that the mechanism of symptoms creation in Chiari I malformation is probably not volume related. Even in patients with syringomyelia, it has been noticed that in a small proportion of patients symptoms and radiological signs have not responded following suboccipital craniectomy, leading certain authors to conclude that the underlying mechanism causing the syringomyelia is not volume related. The presence of normal posterior fossa in Chiari I alone does not explain the development of tonsillar herniation. It could be postulated that localized venous hypertension and possible altered geometry of the posterior fossa43,44 could initiate the downward migration, which subsequently is perpetuated by CSF movement and impaction. Personal observations during foramen magnum decompression operations for Chiari only in the absence of syringomyelia indicate that soon after dural opening and division of arachnoidal adhesions that link the impacted tonsils to the surrounding structures, the cerebellar tonsils usually ascend to their natural position, without the need for further coagulation or resection. Thus, it appears that foramen magnum decompression probably works by allowing disimpaction of the tonsils from the craniovertebral junction, rather than “enlarging” the posterior fossa, as the tonsils never move to occupy the newly enlarged cisterna magna, but ascend to a normal location. In that line, there is a universal tendency for reduction of the size of the craniectomy in the foramen magnum.
Clinical Features
Presenting Symptoms
Symptoms relevant to the presence of syringomyelia include weakness or clumsiness from arms and legs, which may not be following a myotomal distribution; paresthesias, dysesthesias, and pain, which may not be following a dermatomal distribution; unsteady gait; muscle atrophy; and spasticity. Pain is commonly a prominent feature. In a small percentage of patients there may be urinary and fecal incontinence and impotence in male patients. The location of symptoms may not be correlated with radiological findings. They can be strikingly unilateral even though the syrinx may appear to occupy the central part of the cord on imaging. Syringobulbia can be life threatening. The commonest symptom of syringobulbia is spreading facial numbness. Swallowing and voice may also be affected, then vision, hearing, and finally respiratory function. Nocturnal hypoventilation has been described in the presence of syringomyelia not extending to the medulla.45
It should be emphasized that a significant proportion of patients with radiologically identified Chiari I malformation do not experience any symptoms and their malformation was identified incidentally during investigations for other reasons.3,4 A large study of 22,591 MRI scans identified 175 patients with Chiari I malformation and 14% of them were completely asymptomatic.
Clinical Examination Findings
In patients with Chiari I malformation or syringobulbia clinical examination findings include lower cranial nerves and cerebellar signs. In patients with syringomyelia long tract signs are common. Neuro-ophthalmological findings include impaired visual acuity, extraocular muscle palsy, nystagmus, and papilledema in a small minority.46 Ophthalmological assessment is of paramount importance in patients with Chiari I malformation. Other signs from lower cranial nerves include facial sensory loss, sensorineural or conductive hearing loss, impaired vestibular function, vocal cord palsy, and impaired gag reflex. Cerebellar signs such as dysmetria or truncal ataxia are not uncommon.
Clinical examination findings associated with syringomyelia include weakness of arms and legs, not always following a myotomal distribution, and sensory deficits over arms and legs, not always following dermatomal distribution. Unilateral weakness of one upper limb, not infrequently associated with a sudden strain and associated pain, is commonly seen. The small muscles of the hand are often affected first and wasting of the first dorsal interosseous muscle between the fingers and the thumb may be an early finding. The triceps or the shoulder musculature could be affected before the hand. In advanced cases it is not uncommon to find claw deformity in the hand with wasting of all the forearm and arm musculature. Sensory loss can be of spinothalamic or dorsal column type, occasionally in patchy distribution. It is usually unilateral and tends to involve the upper limb early, progressing by an increase of the density of the deficit more often than by anatomical extension. It can even be variable throughout the course of the day, and is presumably related to a variable state of filling of the syrinx. The traditionally described pain/temperature dissociation that is loss of pain and temperature sensation with preserved light touch and joint position sense is rare. Muscular atrophy and fasciculation can be seen as well as dystrophic (Charcot) joints. Hyper- or hyporeflexia can be present depending on the level of syringomyelia.47,48 Asymmetry is not uncommon and certain reflexes may be unexpectedly spared. Spasticity can affect upper and lower limbs. Scoliosis is a common finding with syringomyelia in young children, and is seen often in previously undiagnosed young adults as well.49–53 Short neck and low hairline are seen in patients with basilar invagination. Horner syndrome is seen infrequently. Gross disturbance of sweating can occur.54 Dry skin or hyperhidrosis can be observed, usually symmetrically in the lower half of the body, although the upper limbs may be affected in an asymmetrical distribution with facial involvement at times, and unequal pupils may be the only feature.
In patients with spinal cord injury incomplete paraplegia that deteriorates or the development of new autonomic features may be associated with syringomyelia. The most important features are those that ascend. Descending syringomyelia is rarely diagnosed. In complete paraplegia, improvement of leg spasms could imply downward extension of the syringomyelia. So also could alteration of sweating patterns and impairment of other autonomic functions such as bladder and bowel control and sexual function. Pain is common in post-traumatic syringomyelia, and a paraplegic complaining of severe pain has syringomyelia until proved otherwise.9–12,35,36,55–59 It is frequently associated with straining and progression of neurological deficit. Although it is commonly experienced at the level of the deficit, it can affect sites above or below that level and can be misleading. It can be confused with chest or abdominal disease. Not infrequently it is soon replaced by dysesthetic sensory loss.
Diagnosis
Radiology
MRI scanning shows the Chiari malformation and the extent of the syringomyelia cavity and haustrations, especially in T2-weighted sequences.34,60,61 Around 15% of patients have hydrocephalus. Other pathological conditions are clearly demonstrated. The syrinx in children with profound scoliosis can be difficult to visualize in MRI scanning (see Fig. 28.1). Because the curvature of the spine can be extensive it may not be possible to have the entire spinal cord in a single sagittal view, and it may be difficult to correctly count the vertebral levels and identify the full extent of the syrinx (see Fig. 28.1B and C). Children with significant scoliosis can have syringomyelia in the absence of Chiari I malformation. Post-traumatic syringomyelia and its relation with primary cysts shows well in MRI scans (see Fig. 28.4), although in some patients with extensive spinal fractures it may be difficult to identify the complexity of the bony injury. Spinal lipomas (see Fig. 28.5) and diastematomyelia (see Fig. 28.6) are clearly seen. In patients with spinal lipoma there may be the need to obtain fat suppression sequences to visualize the relation between lipoma and spinal cord better, in preparation for a cord untethering. In patients with diastematomyelia, commonly the syringomyelia cavity is not extensive. Spinal cord tumors are clearly identified in contrast-enhanced MRI sequences (see Fig. 28.8). Whenever a patient is found to have syringomyelia in the absence of a clearly identifiable associated lesion, contrast-enhanced sequences should be obtained to exclude the presence of spinal cord tumor. In a small minority of patients no associated lesion is identified. Information relating to the CSF circulation can be obtained with cardiac gated cine PC-MRI (see Fig. 28.2B). In current clinical practice the value of cine-MRI is limited in the influence it may have in clinical decisions. The utility of this tool is evolving in the study of CSF movement and its correlation with clinical symptoms and outcome.62–68 Sequential MRI is useful in assessing the results of treatment or in observing the evolution of the symptoms and deciding when radiological progression may indicate a need for surgical intervention.69,70
Neurophysiological Tests
Nerve conduction studies, brainstem evoked potentials, spontaneous electromyography (EMG), motor evoked potentials (MEPs), and somatosensory evoked potentials (SSEPs) have been used in the study of patients with syringomyelia.71,72 It has not been easy to use such tests to tailor the indication for surgery, as normal neurophysiological tests do not imply absence of threat of neurological deterioration. Usually these tests are abnormal when clinical symptoms or signs have been established. Nevertheless, they may prove useful in the follow-up of patients treated surgically. SSEPs, EMG, and MEPs can be useful intraoperatively in selected cases with tumors, syringomyelia, and other spinal cord anomalies.
Controversies in Management
Controversy surrounds the following issues:
1. When does hindbrain hernia/Chiari I malformation need surgical treatment?
2. When does syringomyelia need surgical treatment?
3. What is the best surgical treatment for the management of hindbrain hernia?
4. What is the best surgical treatment for the management of syringomyelia?
5. What is the best management of recurrent syringomyelia?
6. What is the best management of the associated hydrocephalus?
Natural History
Hindbrain Hernia
There are no prospective, nonoperative studies outlining the natural history of hindbrain hernia and syringomyelia. In surgical series of patients with symptomatic hindbrain hernia the incidence of syringomyelia varies from 55% to 85%,9,61,73–79 but inevitably all such series have a highly selected population. There are very few studies following “asymptomatic” patients.4 The absence of such data is largely due to historical reasons: before the advent of MRI it was very difficult to diagnose hindbrain hernia and syringomyelia. Since the introduction of MRI, the condition is diagnosed more frequently, and the clinicians have adopted a wide variety of successful surgical and conservative approaches. Neurosurgeons who see larger numbers of patients with these conditions tend to appreciate more common signs and symptoms such as motor and sensory deficits or tussive headaches.
The general attitude is that a completely asymptomatic Chiari I malformation can be managed conservatively and followed closely.80 The difference of opinion among clinicians rests on what constitutes asymptomatic hindbrain hernia. In most patients who provide a history, there is clear evidence of tussive, cough-, or exercise-induced headache or occipital pain. Some even admit to arm pain on exertion. In small children, motor developmental delay of mild degree is frequently seen in both arm dexterity and fluency of walking. Such cases should be seen as symptomatic patients and considered for potential treatment. Other more subtle symptoms and signs can go unnoticed unless a longitudinal approach is adopted. It should be remembered that intracranial hypertension can be otherwise “silent” and only manifest with papilledema on funduscopic examination. It is the author’s belief that the incidence of truly asymptomatic hindbrain hernia is smaller than stated. Instead, there is a spectrum of symptom intensity and symptoms may change or develop in time, and the neurosurgeon’s decision to operate or not is relevant to his or her expertise in the field and willingness to follow these patients over the long term.
Syringomyelia
Similar to hindbrain hernia, the natural history of untreated syringomyelia is not charted conclusively. It is considered that syringomyelia deteriorates with time, but the speed with which this deterioration takes place is unknown.81 When faced for the first time with a patient with syringomyelia, it is difficult to postulate on the risk of sudden neurological deterioration, although such a complication is well documented albeit rare. Similarly, in the presence of a large syringomyelia cavity, it is not known what percentage of patients develop symptoms over what time frame. Whereas the typical symptoms and signs of syringomyelia are readily appreciated, the subtler ones are easier to miss. Mild scoliosis and very subtle motor developmental delay in very young children are important. Long-standing syringomyelia leads to gliosis in the spinal cord and irreversible neurological damage. Thus, it would be reasonable to have a low threshold for considering treatment when syringomyelia is discovered.
Surgery
Indications for Surgical Treatment
 In patients with Chiari I malformation only, and no syringomyelia, the presence of occipital headaches, cough induced or deteriorating, and possibly other cerebellar symptoms is an indication for surgical treatment with craniovertebral decompression. Other subtle symptoms should be considered individually.
In patients with Chiari I malformation only, and no syringomyelia, the presence of occipital headaches, cough induced or deteriorating, and possibly other cerebellar symptoms is an indication for surgical treatment with craniovertebral decompression. Other subtle symptoms should be considered individually.
 In patients with Chiari I malformation and syringomyelia, the presence of relevant symptoms and clinical findings, as discussed previously, constitutes an indication for surgical treatment with craniovertebral decompression. A distended syringomyelia occupying the cervical cord, even if asymptomatic, merits surgical treatment, as it potentially threatens vital neurological functions. In contrast, the patient with a small, two-level cavity and no relevant symptoms can be watched with repeat MRI scans annually.
In patients with Chiari I malformation and syringomyelia, the presence of relevant symptoms and clinical findings, as discussed previously, constitutes an indication for surgical treatment with craniovertebral decompression. A distended syringomyelia occupying the cervical cord, even if asymptomatic, merits surgical treatment, as it potentially threatens vital neurological functions. In contrast, the patient with a small, two-level cavity and no relevant symptoms can be watched with repeat MRI scans annually.
 The presence of scoliosis in children, even in the absence of other neurological symptoms, requires surgical treatment to stabilize the progression of scoliosis. Most orthopedic surgeons would not contemplate surgical correction of scoliosis in the presence of untreated syringomyelia, as the risk of postoperative paraplegia or quadriplegia is significant.
The presence of scoliosis in children, even in the absence of other neurological symptoms, requires surgical treatment to stabilize the progression of scoliosis. Most orthopedic surgeons would not contemplate surgical correction of scoliosis in the presence of untreated syringomyelia, as the risk of postoperative paraplegia or quadriplegia is significant.
 Patients with post-traumatic syringomyelia merit early surgery because syringomyelia can expand silently and insidiously, compromising residual neurological function. Surgical decompression at the site of the subarachnoid block is recommended, which is commonly the fracture site.
Patients with post-traumatic syringomyelia merit early surgery because syringomyelia can expand silently and insidiously, compromising residual neurological function. Surgical decompression at the site of the subarachnoid block is recommended, which is commonly the fracture site.
 In patients with spinal dysraphism, syringomyelia rarely constitutes an urgent indication for surgery. An expanded syrinx may be the result of a shunt failure, which needs to be addressed first. Patients with symptoms from spinal cord tethering and a new syrinx may need surgical treatment.
In patients with spinal dysraphism, syringomyelia rarely constitutes an urgent indication for surgery. An expanded syrinx may be the result of a shunt failure, which needs to be addressed first. Patients with symptoms from spinal cord tethering and a new syrinx may need surgical treatment.
 Patients with spinal cord tumors require surgical excision for their tumor, which leads to reduction of the syringomyelia cavity.82 Recurrence of syringomyelia commonly implies tumor recurrence or CSF block, or arachnoiditis at the level of the previous surgery.
Patients with spinal cord tumors require surgical excision for their tumor, which leads to reduction of the syringomyelia cavity.82 Recurrence of syringomyelia commonly implies tumor recurrence or CSF block, or arachnoiditis at the level of the previous surgery.
 Patients with spinal arachnoid cysts commonly have neurological symptoms from cord compression and require surgical excision or drainage of the cyst.83,84
Patients with spinal arachnoid cysts commonly have neurological symptoms from cord compression and require surgical excision or drainage of the cyst.83,84
 Patients with postinflammatory syringomyelia present particular difficulties because commonly they have significant neurological deficits from their condition even before syringomyelia develops. This is not always easy to appreciate if the development of radiological syringomyelia is associated with the development of new symptoms. When a clear link is established between radiological and clinical deterioration, surgery should be pursued. If such a clear link is not apparent, a period of observation and regular repeat scanning may be preferable.
Patients with postinflammatory syringomyelia present particular difficulties because commonly they have significant neurological deficits from their condition even before syringomyelia develops. This is not always easy to appreciate if the development of radiological syringomyelia is associated with the development of new symptoms. When a clear link is established between radiological and clinical deterioration, surgery should be pursued. If such a clear link is not apparent, a period of observation and regular repeat scanning may be preferable.
 Patients with recurrent syringomyelia and unclear neurological signs require careful assessment. Repeat surgery for such patients often has guarded results and caution should be exercised. Often an initial period of observation and repeat MRI scans is a good strategy, reserving surgery for when there is a clear clinical or radiological deterioration.
Patients with recurrent syringomyelia and unclear neurological signs require careful assessment. Repeat surgery for such patients often has guarded results and caution should be exercised. Often an initial period of observation and repeat MRI scans is a good strategy, reserving surgery for when there is a clear clinical or radiological deterioration.
The challenging patients are those with unremarkable symptoms and whose syringomyelia is not progressing or has only moderate distention. In patients with post-traumatic syringomyelia, and incomplete paraplegia, indications for surgery can be difficult to discern. There is a risk of allowing further deterioration to occur by not intervening surgically. It is not uncommon for a patient who has what appears to be a stable syringomyelia, not increasing in size over a number of years, to develop rapid clinical deterioration. On the other hand, there is a complication rate associated with any operative procedure, and it is often difficult to justify surgery in stable patients. As the natural history of syringomyelia can be variable, it is recommended to err toward early surgical treatment, as it is likely that untreated patients will deteriorate. In general, it is believed that early surgery offers better long-term results.9,21,36 Patients with recurrent syringomyelia, years after an initial successful surgical treatment and unclear neurological signs, require careful assessment and pose a significant dilemma. Repeat surgery for such patients often has guarded results and caution should be exercised. Often an initial period of clinical observation and repeat MRI scans is a good initial management strategy, reserving surgery for when there is a clear clinical or radiological deterioration.
Surgical Strategy
 Patients with Chiari I malformation (with or without syringomyelia) require craniovertebral decompression as the first procedure.
Patients with Chiari I malformation (with or without syringomyelia) require craniovertebral decompression as the first procedure.
 Patients with post-traumatic syringomyelia require surgical decompression at the site of the subarachnoid block.
Patients with post-traumatic syringomyelia require surgical decompression at the site of the subarachnoid block.
 Patients with dysraphic states require cord untethering or craniovertebral decompression relevant to their pathological condition as the first procedure.
Patients with dysraphic states require cord untethering or craniovertebral decompression relevant to their pathological condition as the first procedure.
 Patients with post-inflammatory syringomyelia need careful radiological evaluation to appreciate the site of the subarachnoid block, and surgical strategy is then tailored accordingly.
Patients with post-inflammatory syringomyelia need careful radiological evaluation to appreciate the site of the subarachnoid block, and surgical strategy is then tailored accordingly.
Surgical Management of Chiari I Malformation
Craniovertebral decompression for Chiari I malformation includes occipital craniectomy and removal of the arch of C1 at least, depending on the extent of the hindbrain hernia.20,80,85–101 This aims to remove the block of CSF flow in the craniovertebral junction due to the prolapsed tonsils. The size of the craniectomy has been decreasing over the years, and now a craniectomy flap of 3 × 3 cm is regarded as satisfactory; larger defects are associated with cerebellar slumping.69 This operation leads to clinical improvement of symptoms in 80% of patients and to radiological improvement of syringomyelia in up to 70% of the patients.102 Syringopleural or syringosubarachnoid shunts used as primary treatment have a very poor long-term success rate in the presence of an active subarachnoid block, which acts as a filling mechanism for the syringomyelia.8,103–107
Controversy exists on whether the arachnoid mater should be opened. Most neurosurgeons prefer to open the arachnoid. The proponents of opening the arachnoid maintain that dissection of the arachnoid adhesions on the foramen magnum safeguards against recurrence. The proponents of leaving the arachnoid intact believe that breaching the arachnoid can promote creation of further adhesions owing to the intraoperative spillage of blood. Essentially, the decision focuses on opening the dura or not, as commonly during dural opening the arachnoid is breached and has to be opened widely. Recently, intraoperative ultrasound scanning (US) has indicated that absence of CSF flow at the foramen magnum after craniectomy may be an indication for opening the arachnoid membrane and is used by several neurosurgeons routinely.108 Utilization of intraoperative ultrasound is not regarded as mandatory, though. Recently, the technique of extradural decompression has been revisited with claimed satisfactory results, especially in young children.
Another controversial issue is the use of a duraplasty graft to enlarge the cisterna magna after lysis of the arachnoid adhesions versus closure of the craniectomy without duraplasty, by closing the overlying muscles and leaving the dura open, thus creating a pseudomeningocele.9,21,80,85,93,109–112 When performing duraplasty, some surgeons prefer to use pericranial graft, harvested from the occipital area just above the craniectomy site, and others prefer to use artificial graft. The use of a duraplasty decreases the incidence of CSF leak but often adequately treats the associated syringomyelia. In patients who do not receive a duroplasty, the risk of a CSF leak is higher, but the possibility of recurrence or failure to adequately treat an associated syrinx decreases.
Patients who have craniocervical instability in the context of syndromes affecting the craniocervical junction (e.g., Morquio syndrome, achondroplasia) may need simultaneous atlanto-occipital fixation in the same operation after the craniovertebral decompression.74,113,114 A small group of patients have anterior compression from basilar invagination and should be considered for anterior decompression transorally.115
Surgical Management of Post-Traumatic Syringomyelia
In the 1970s and 1980s syringosubarachnoid and syringopleural shunts were used widely but in the 2000s long-term effectiveness has been questioned.11,55,87,105,106,116–122 A variety of complications and infection have been observed. The drain functions for some time, the cord collapses around it, and the draining holes become occluded by gliotic tissue. Subsequently the syringomyelia recurs if the filling mechanism has not been corrected.8 The current treatment of post-traumatic syringomyelia is decompressive laminectomy and subarachnoid space reconstruction by lysis of arachnoid adhesions at the fracture site.9,35,36,57,83,94,123,124 This operation should not be performed before issues of spinal stability have been addressed. This technique results in radiological improvement of the syringomyelia in up to 80% of the patients.
In the late 1980s and early 1990s attempts were made to treat post-traumatic syringomyelia with omental grafting.125 This operation involved laparotomy first in order to harvest a vascularized pedicle of omentum, which was subsequently tunneled under the skin to the spine and was laid over the injured spinal cord at the injury site, which was exposed by laminectomy. These operations were associated with high morbidity and low success rates in controlling the syringomyelia and have been abandoned.
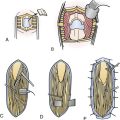
Surgical Management of Residual or Recurrent Syringomyelia
When an initial decrease of syringomyelia size has been observed, followed by recurrence, reexploration of the craniovertebral junction, opening of the arachnoid, and extensive dissection of the adhesions in the regions of all the foramina of the fourth ventricle are required.126,127 This surgical strategy is associated with an average success rate (60%). Surgical variations include the use of stents in the foramen magnum to avoid recurrent adhesions. Although the author does not favor stents in this region, they have been reported to offer good long-term control of the syringomyelia. A significant problem with stents in the foramen magnum is the high risk of migration into the brainstem, which causes significant neurological deterioration. If that fails, then as a last measure a syringopleural or subarachnoid shunt could be attempted. These shunts enjoy an average chance of radiological improvement (around 50-60%) but lower than average chance of clinical improvement (around 10-20%).128 However, often, they are the last resort to avoid clinical deterioration in a patient with an expanding syrinx. Insertion of a syringopleural or syringosubarachnoid shunt requires laminotomy in the site of the widest diameter of the syrinx and intradural exposure of the spinal cord. A midline myelotomy is performed. It is recommended to use a fine ultrasound probe prior to performing the myelotomy, to confirm the most dilated location of the syrinx. However, often ultrasound is not needed as the syrinx can dilate the cord so much that the pial surface becomes translucent, making placement of the myelotomy easier. After a small myelotomy is performed, a T-shaped catheter is inserted in the syrinx cavity and secured with pial fine sutures. The other end is placed in the subarachnoid space or threaded toward the chest wall in the midaxillary line and in the pleural cavity. As all shunts, syringomyelia shunts have similar mechanical and infectious risks.
The presence of persistent syringomyelia despite adequate craniovertebral decompression may indicate underlying intracranial hypertension.124,127,129 Invasive intracranial pressure (ICP) measurement may be required to investigate and resolve this issue. In the presence of ventriculomegaly and raised intracranial pressure, ventriculoperitoneal shunt may eventually help resolve the persistent syringomyelia if all other measures have failed.79
Overall, patients with recurrent syringomyelia or recurrent arachnoiditis in the region of the foramen magnum pose significant challenge on their long-term management, and in general they do not have good long-term outcome, as they continue to deteriorate over a number of years.130
Management of the Associated Hydrocephalus
The connection between hydrocephalus and syringomyelia has not been elucidated fully yet. Traditionally hydrocephalus is treated first, before a craniovertebral decompression. From cine PC-MRI there is evidence that hydrocephalus is due to fourth ventricle obstruction. When ventricular shunting is performed first, the syringomyelia cavity reduces in size but the need for craniovertebral decompression is not avoided. Recently, endoscopic third ventriculostomy has been used to treat hydrocephalus, with good results in terms of syringomyelia resolution.131,132
Complications
The complication rate for craniovertebral or spinal decompression is low. Perioperative fatality is rare. Wound infection, CSF leak, meningitis, subdural hematoma, urinary tract infection, and thromboembolic complications have been observed at a low rate. Self-limiting aseptic meningitis affects many patients after craniovertebral decompression, more often when the arachnoid has been opened. A very small percentage of patients suffer catastrophic complications such as posterior fossa hematoma, transverse sinus thrombosis, or brainstem infarction due to posterior inferior cerebellar artery damage. Cerebellar sag or slump has been reported as a delayed side effect of cranioveretebral decompression. It was more common in the 1980s to 1990s and presented with intractable headaches and lower cranial nerve signs. In recent years there has been a tendency for smaller occipital craniectomy, which has reduced the incidence of this complication.
Treatment Outcome
Up to 80% of patients with hindbrain-related syringomyelia experience clinical improvement after craniovertebral decompression. Most symptoms improve, but an unfortunate minority experience long-standing incapacitating chronic headaches, often associated with radiological presence of arachnoid adhesions at the region of the foramen magnum. Established neurological deficits associated with syringomyelia such as sensory loss and weakness improve little. Muscle wasting and severe lower cranial nerve palsies do not improve. Early myelopathy improves variably. Established spasticity improves little and often other surgical options have to be employed (e.g., intrathecal baclofen).133
Intracranial Hypertension and Syringomyelia
Intracranial hypertension may be more common among children with isolated Chiari I malformation than previously realized.134,135 Routine systematic detailed ophthalmoscopy can detect papilledema, which if left untreated can cause blindness. There have been reports of an incidence of up to 13% of papilledema in patients with hindbrain hernia with or without syringomyelia, and some patients may have raised intracranial hypertension without papilledema.135 The incidence of intracranial hypertension in the absence of papilledema remains unknown and may well be more frequent than initially thought. The realization that intracranial hypertension may be present in patients with syringomyelia is fairly recent, and it is possible that those who do not demonstrate resolution of syringomyelia despite apparently successful surgery may well harbor raised ICP. More research is expected to illuminate this aspect of syringomyelia in the future.
Syringomyelia with Chiari II Malformation
1. In Chiari II malformation most of the prolapsed cerebellar tissue is part of the vermis and not the tonsils, as the malformation is created in utero before formation of the cerebellar tonsils. Often, the lower medulla and part of the fourth ventricle are also below the foramen magnum. Whereas in Chiari I the mobile tonsillar tissue can move as a “piston” with every cardiac cycle and “plug” the foramen magnum, in Chiari II the hindbrain hernia contains less “mobile” structures, such as the vermis and the lower medulla, so the analogy may not be appropriate.
2. In support of the previous point, during craniovertebral exploration, in patients with Chiari II malformation there are always significant and dense arachnoid adhesions in the region of the foramen magnum and foramina of Magendie and Luschka, much more than in patients with Chiari I malformation. This is evident even in children who are only a few weeks old at operation.
3. The majority of patients with Chiari I malformation are symptomatic from it, whereas the majority of patients with Chiari II malformation do not experience symptoms directly caused by the malformation unless they present with stridor at birth.80,136
4. Most patients with Chiari I malformation and syringomyelia will require surgical treatment at some stage of their disease. In the context of Chiari II malformation the coexistence of syringomyelia can vary between 40% and 90% in different reports,101,137–142 but only a third of them require treatment for syringomyelia.138
5. In the context of Chiari I malformation, although the phenomenon of progressive development of syringomyelia has been well described, in most patients syringomyelia is present ab initio, at the first clinical presentation,76 and very often is responsible for the symptoms. In the context of Chiari II malformation, syringomyelia may be present at birth, and commonly expands many years later, probably as a manifestation of recurrent spinal cord tethering or insufficient shunt function. The average age of children with Chiari II who have symptomatic syringomyelia is between 4 and 7 years.101,138–142
6. In patients with Chiari I malformation and syringomyelia, hydrocephalus is rare. In contrast, in most patients (80-90%) with Chiari II and syringomyelia there is long-standing hydrocephalus, which has been treated in the first few weeks of life with a ventriculoperitoneal shunt.136,143
There has been no study demonstrating a correlation between the extent of herniation of the hindbrain and the incidence of syringomyelia. In recent years, prenatal repair of myelomeningocele has been performed, and this has been shown to lead to improved motor outcomes and reduced need for ventriculoperitoneal shunting.144 A recent randomized controlled trial showed improved motor outcome and reduced need for shunting in children who had prenatal repair of myelomeningocele, but there was an increased maternal and fetal risk of serious complications such as preterm delivery and uterine dehiscence.145 Nevertheless, as this treatment has been performed for less than two decades and in only three centers worldwide, it is unclear if it leads also to reduced syringomyelia incidence in these patients.
Commonly, patients who had closure of myelomeningocele at birth and have Chiari II malformation, hydrocephalus, and syringomyelia have been stable for many years and at some stage, they present with gradual progressively deteriorating neurological symptoms and signs related to bulbar, long tract, or bladder function.101,129,138–142 Bulbar symptoms include respiratory distress, stridor or sleep apnea, vocal cord paresis, difficulty in swallowing, episodes of aspiration, impaired gag reflex, and oculomotor paresis with squint or diplopia and nystagmus. Motor symptoms and signs include deterioration of leg function in ambulatory patients with progressive difficulty in walking and clumsiness or even spasticity, and if the cervical spinal cord is affected there may be new problems in the upper limbs with clumsiness in fine hand movements and dexterity (e.g., deterioration of writing pattern). Sensory symptoms include new pain or deterioration of previously existing pain in trunk and lower limbs, altered sweating pattern especially below the level of the paraplegia, and patchy altered sensation in a nondermatomal distribution. Patients who have intact bladder function can develop deterioration of the micturition pattern. Many paraplegic patients with spina bifida have scoliosis, and the development of syringomyelia can coincide with deterioration of the scoliotic curve.146
In patients with Chiari II malformation the causative link of such symptoms with syringomyelia is not always obvious or firm. Patients with Chiari II, hydrocephalus, and a shunt often develop many of the symptoms outlined previously even in the absence of syringomyelia when their shunt is malfunctioning, and they improve after successful shunt revision. Even scoliosis deterioration has been reported in association with shunt malfunction.147 Moreover, most patients who had repair of myelomeningocele at birth have the radiological appearance of a tethered cord at the repair site in MRI scans. Regardless of how successful and anatomically correct the repair has been, the spinal cord never ascends to its correct level and always appears attached to the area of the repaired defect. This situation becomes established in the first few weeks after the repair and remains unchanged even when the patient is clinically very well and stable.
The presence of syringomyelia is easily diagnosed in the sagittal spinal T1- and T2-weighted MRI scans in patients with Chiari II (see Fig. 28.7). In contrast to Chiari I–related syringomyelia which is most often cervical in location, in Chiari II the center of gravity of the cavity is located usually in the thoracic cord. It can be either “segmental,” occupying a few segments of the spinal cord, or “holocord,” occupying the entire spinal cord. Although in Chiari II the syringomyelia cavity is commonly longer than in Chiari I, its transverse diameter is usually less than that seen in cavities associated with Chiari I malformation. Rarely, the syringomyelia cavity is in the cervical cord and threatens to become syringobulbia.
Occasionally, the presence of syringomyelia is discovered incidentally, in the course of such a routine MRI scan.138 These patients tend to have mild to moderate syringomyelia. In the absence of symptoms, and if the cavity’s transverse diameter is less than half the width of the spinal cord, most often we would elect to avoid surgery and instead observe at first and repeat the scan in a few months, before we decide to consider surgical treatment. Clinically “silent” syringomyelia cavities often remain radiologically stable and do not require treatment for years. In most units, though, routine MRI scans of patients with Chiari II malformation are not performed, reserving that examination for when new clinical problems arise.
In most cases, the presence of new neurological symptoms prompts an MRI scan, which can demonstrate syringomyelia. It is difficult to determine whether the clinical symptoms are due to the syringomyelia, the hydrocephalus, or the tethered cord. This dilemma has created inconsistencies in the management of patients with Chiari II and syringomyelia. There are no agreed protocols or robust evidence originating from randomized studies on how these patients should be managed,148 and different schemes and algorithms have been suggested based on clinical series, often reflecting prevailing tendencies at the time and the difference in experience, training, and attitude. Although there have been many attempts to classify and group different neurological symptoms, the situation is even more confusing with scoliosis, as there is no clear evidence if its deterioration is directly related to syringomyelia.146
It is universally accepted that in a patient who has had treatment for hydrocephalus with a ventriculoperitoneal shunt and now presents with clear neurological deterioration and significant syringomyelia, the shunt must be investigated first, and even in the absence of ventriculomegaly or symptoms of raised ICP, shunt revision should be performed to exclude shunt malfunction and establish a functioning shunt.101,137–142 In most patients, shunt revision leads to improvement of the clinical symptoms and radiological improvement of the syringomyelia or at worst stabilization, thus not requiring any further surgical measures. Recently, endoscopic third ventriculostomy (ETV) has been tried when a patient presents with blocked shunt, in order to remove the shunt completely, with some success.
In a small proportion of patients the ventricles have been either normal or borderline enlarged at birth and these patients have not had surgical ventricular drainage procedures.144 An even smaller proportion has moderate ventriculomegaly without symptoms of raised pressure, which represents a state of arrested hydrocephalus and is not treated surgically in most cases. Patients who have syringomyelia and have not had shunts before, in the presence of moderate ventriculomegaly, should be considered for surgical drainage of the ventricles. Most surgeons would insert a ventricular shunt, although in the past few years there have been reports of successful treatment and resolution of the syringomyelia cavity with ETV.131
If hydrocephalus treatment (shunt revision/insertion or ETV) has not resulted in clinical or radiological improvement, craniovertebral decompression should be performed to establish CSF circulation in the craniocervical junction if the predominant symptoms are those of craniovertebral junction compression, and tethered cord release should be undertaken if the predominant symptoms are those of bladder dysfunction.101,141 Both surgical options have significant challenges.
Craniovertebral decompression in Chiari II malformation is considerably more difficult than in Chiari I, as part of the contents of the hindbrain hernia is not only the cerebellum but also the lower medulla. It is not uncommon for the fourth ventricle to be at the level of the foramen magnum or even lower. The hindbrain hernia can extend down as low as C4-C5. When C1-C2 laminectomy has been performed and if the dura is opened, care should be taken as dissection may result in early access and exposure of the floor of the fourth ventricle. If the surgeon is opening the dura, care must be taken to ensure that durotomy is below the low-lying torcular. In some patients, a surgeon may elect not to open the dura and just perform a bony decompression as the results can be catastrophic if care is not taken to avoid the low-lying sinuses. Inadvertent damage to the brainstem can have severe neurological side effects and bulbar palsy. At the end of the procedure, if the dura is opened, closure is performed either with duraplasty from pericranium or artificial material, or by leaving the dura open in the pseudomeningocele technique as for Chiari I. Craniovertebral decompression in patients with Chiari II has mixed results.129,138 Severe bulbar symptoms tend not to improve and long-tract signs show moderate improvement. Bilateral vocal cord paresis and very young age are poor prognostic factors.129 When craniovertebral decompression is performed for syringomyelia, especially in the absence of bulbar symptoms, results are better with good chance of success, over 60%.
If despite all these measures, the clinical symptoms and the radiological appearances of syringomyelia persist, insertion of a syringopleural or syringosubarachnoid shunt could be considered.107,138–140 The use of syringomyelia shunts is controversial. Many authors have suggested them as an early surgical option, before craniovertebral decompression.137,141 There is no conclusive evidence on the best time to use them. There have been reports of good result in spina bifida patients.107 Nevertheless, in the analogy of Chiari I malformation, if a syringomyelia shunt is inserted before addressing the block at the foramen magnum, the beneficial effect tends to be short lived.8
Armonda R.A., Citrin C.M., Foley K.T., Ellenbogen R.G. Quantitative cine-mode magnetic resonance imaging of Chiari I malformations: an analysis of cerebrospinal fluid dynamics. Neurosurgery. 1994;35:214-224.
Gardner W.J., Angel J. The mechanism of syringomyelia and its surgical correction. Clin Neurosurg. 1959;6:131-140.
Milhorat T.H., Chou M.W., Trinidad E.M., et al. Chiari I malformation redefined: clinical and radiographic findings for 364 symptomatic patients. Neurosurgery. 1999;44:1005-1017.
Oldfield E.H., Muraszko K., Shawker T.H., Patronas N.J. Pathophysiology of syringomyelia associated with Chiari I malformation of the cerebellar tonsils. Implications for diagnosis and treatment. J Neurosurg. 1994;80:3-15.
Sgouros S., Williams B. A critical appraisal of drainage in syringomyelia. J Neurosurg. 1995;82:1-10.
Williams B. Simultaneous cerebral and spinal fluid pressure recordings. Cerebrospinal dissociation with lesions at the foramen magnum. Acta Neurochir. 1981;59:123-142.
Please go to expertconsult.com to view the complete list of references.
1. Leyden E. Ueber hydromyelus und syringomyelia. Virchows Arch Path Anat. 1876;68:1-26.
2. Abbe R., Coley W.B. Syringomyelia. Operation-exploration of cord, withdrawal of fluid, exhibition of patient. J Nerv Ment Dis. 1892;19:512-520.
3. Meadows J., Kraut M., Guarneri M., et al. Asymptomatic Chiari Type I malformations identified on magnetic resonance imaging. J Neurosurg. 2000;92:920-926.
4. Novegno F., Caldarelli M., Massa A., et al. The natural history of the Chiari type I anomaly. J Neurosurg Pediatr. 2008;2:179-187.
5. Jatavallabhula N.S., Armstrong J., Sgouros S., Whitehouse W. Spontaneous resolution of isolated Chiari I malformation. Childs Nerv Syst. 2006;22:201-203.
6. Chumas P.D., Armstrong D.C., Drake J.M., et al. Tonsillar herniation: the rule rather than the exception after lumboperitoneal shunting in the pediatric population. J Neurosurg. 1993;78:568-573.
7. Payner T.D., Prenger E., Berger T.S., Crone K.R. Aquired Chiari malformations: incidence, diagnosis, and management. Neurosurgery. 1994;34:429-434.
8. Sgouros S., Williams B. A critical appraisal of drainage in syringomyelia. J Neurosurg. 1995;82:1-10.
9. Williams B. Syringomyelia. Neurosurg Clin North Am. 1990;1:653-685.
10. Barnett H.J.M., Botterell E.H., Jousse A.T., Wynn-Jones M. Progressive myelopathy as a sequel to traumatic paraplegia. Brain. 1966;89:159-173.
11. Barnett H.J.M., Jousse A.T. Posttraumatic syringomyelia (cystic myelopathy). Vinken P.J., Bruyn G.W., editors. Handbook of Clinical Neurology. Vol. 26. Amsterdam: North-Holland; 1976:113-157.
12. Rossier A.B., Foo D., Shillito J., Dyro F.M. Posttraumatic cervical syringomyelia. Brain. 1985;108:439-461.
13. Ball M.J., Dayan A.D. Pathogenesis of syringomyelia. Lancet. 1972;ii:799-801.
14. Fischbein N.J., Dillon W.P., Cobbs C., Weinstein P.R. The “presyrinx” state: a reversible myelopathic condition that may precede syringomyelia. AJNR. 1999;20:7-20.
15. Goh S., Bottrell C.L., Alken A.H., et al. Presyrinx in children with Chiari malformations. Neurology. 2008;71:351-356.
16. Levy E.I., Heiss J.D., Kent M.S., et al. Spinal cord swelling preceding syrinx development. Case report. J Neurosurg. 2000;92(Suppl 1):93-97.
17. Gardner J.W. Hydrodynamic mechanism of syringomyelia: its relationship to myelocele. J Neurol Neurosurg Psychiatry. 1965;28:247-259.
18. Gardner W.J., Angel J. The mechanism of syringomyelia and its surgical correction. Clin Neurosurg. 1959;6:131-140.
19. Williams B. Simultaneous cerebral and spinal fluid pressure recordings. Cerebrospinal dissociation with lesions at the foramen magnum. Acta Neurochir. 1981;59:123-142.
20. Williams B. A critical appraisal of posterior fossa surgery for communicating syringomyelia. Brain. 1978;101:223-250.
21. Williams B. Surgery for hindbrain related syringomyelia. In: Symon L., editor. Advances and Technical Standards in Neurosurgery. Wien: Springer-Verlag; 1993:108-164.
22. Heiss J.D., Patronas N., DeVroom H.L., et al. Elucidating the pathophysiology of syringomyelia. J Neurosurg. 1999;91:553-562.
23. Oldfield E.H., Muraszko K., Shawker T.H., Patronas N.J. Pathophysiology of syringomyelia associated with Chiari I malformation of the cerebellar tonsils. Implications for diagnosis and treatment. J Neurosurg. 1994;80:3-15.
24. Bertram C.D., Brodbelt A.R., Stoodley M.A. The origins of syringomyelia: numerical models of fluid/structure interactions in the spinal cord. J Biomech Eng. 2005;127(7):1099-1109.
25. Carpenter P.W., Berkouk K., Lucey A.D. Pressure wave propagation in fluid-filled co-axial elastic tubes. Part 2: mechanisms for the pathogenesis of syringomyelia. J Biomech Eng. 2003;125(6):857-863.
26. Chang H.S., Nakagawa H. Hypothesis on the pathophysiology of syringomyelia based on simulation of cerebrospinal fluid dynamics. J Neurol Neurosurg Psychiatry. 2003;74:344-347.
27. Cho K.H., Iwasaki Y., Imamura H., et al. Experimental model of posttraumatic syringomyelia: the role of adhesive arachnoiditis in syrinx formation. J Neurosurg. 1994;80:133-139.
28. Hemley S.J., Biotech B., Tu J., Stoodley M.A. Role of the blood-spinal cord barrier in posttraumatic syringomyelia. J Neurosurg Spine. 2009;11:696-704.
29. Hentschel S., Mardal K.A., Lovgren A.E., et al. Characterization of cyclic CSF flow in the foramen magnum and upper cervical spinal canal with MR flow imaging and computational fluid dynamics. AJNR Am J Neuroradiol. 2010;31(6):997-1002.
30. Martin B.A., Loth F. The influence of coughing on cerebrospinal fluid pressure in an in vitro syringomyelia model with spinal subarachnoid space stenosis. Cerebrospinal Fluid Res. 2009;6:17.
31. Stoodley M.A., Jones N.R., Yang L., Brown C.J. Mechanisms underlying the formation and enlargement of noncommunicating syringomyelia: experimental studies. Neurosurg Focus. 2000;8(3):E2.
32. Frankel H.L. Ascending cord lesion in the early stages following spinal injury. Paraplegia. 1969;6:111-118.
33. Kakoulas B. Pathology of spinal injuries. Cent Nerv Syst Trauma. 1984;1:117-129.
34. Quencer R.M. The injured spinal cord: evaluation with magnetic resonance and intraoperative sonography. Radiol Clin North Am. 1988;26:1025-1045.
35. Williams B., Terry A.F., Jones H.W.F., McSweeney T. Syringomyelia as a sequel to traumatic paraplegia. Paraplegia. 1981;19:67-80.
36. Williams B. Post-traumatic syringomyelia, an update. Paraplegia. 1990;28:296-313.
37. Nyland H., Krogness K.G. Size of posterior fossa in Chiari type 1 malformation in adults. Acta Neurochir. 1978;40:233-242.
38. Stovner L.J., Bergan U., Nilsen G., Sjaastad O. Posterior cranial fossa dimensions in the Chiari I malformation: relation to pathogenesis and clinical presentation. Neuroradiology. 1993;35:113-118.
39. Badie B., Mendoza D., Batzdorf U. Posterior fossa volume and response to suboccipital decompression in patients with Chiari I malformation. J Neurosurg. 1995;37:214-218.
40. Nishikawa M., Sakamoto H., Hakuba A., et al. Pathogenesis of Chiari malformation: a morphometric study of the posterior cranial fossa. J Neurosurg. 1997;86:40-47.
41. Tubbs R.S., Wellons J.C.III, Smyth M.D., et al. Children with growth hormone deficiency and Chiari I malformation: a morphometric analysis of the posterior cranial fossa. Pediatr Neurosurg. 2003;38:324-328.
42. Sgouros S., Kountouri M., Natarajan K. Posterior fossa volume in children with Chiari malformation type I. J Neurosurg Pediatr. 2006;105(Suppl 2):101-106.
43. Sgouros S., Kountouri M., Natarajan K. Skull base growth in children with Chiari malformation type I. J Neurosurg Pediatr. 2007;107(Suppl 3):188-192.
44. Vega A., Quintana F., Berciano J. Basichondrocranium anomalies in adult Chiari type I malformation: a morphometric study. J Neurol Sci. 1990;99:137-145.
45. Bhangoo R., Sgouros S., Walsh A.R., Clarke J.R. Hindbrain-hernia-related syringomyelia without syringobulbia, complicated by permanent nocturnal central hypoventilation requiring non-invasive ventilation. Childs Nerv Syst. 2006;22:113-116.
46. Rowlands A., Sgouros S., Williams B. Ocular manifestations of hindbrain-related syringomyelia and outcome following craniovertebral decompression. Eye. 2000;14:884-888.
47. Dworkin G.E., Staas W.E. Posttraumatic syringomyelia. Arch Phys Med Rehabil. 1985;66:329-331.
48. Umbach I., Heilporn A. Post-spinal cord injury syringomyelia. Paraplegia. 1991;29:219-221.
49. Arai S., Ohtsuka Y., Moriya H., et al. Scoliosis associated with syringomyelia. Spine. 1993;18:1591-1592.
50. Bhangoo R., Sgouros S. Scoliosis in children with Chiari I-related syringomyelia. Childs Nerv Syst. 2006;22:1154-1157.
51. Ghanem I.B., Londono C., Delalande O., Dubousset J.F. Chiari I malformation associated with syringomyelia and scoliosis. Spine. 1997;22:1313-1317.
52. Hoffman H.J., Neill J., Crone K.R., et al. Hydrosyringomyelia and its management in childhood. Neurosurgery. 1987;21:347-351.
53. Ono A., Suetsuna F., Ueyama K., et al. Surgical outcomes in adult patients with syringomyelia associated with Chiari malformation type I: the relationship between scoliosis and neurological findings. J Neurosurg Spine. 2007;6(3):216-221.
54. Stanworth P. The significance of hyperhidrosis in patients with post-traumatic syringomyelia. Paraplegia. 1982;20:282-287.
55. Edgar R.E., Quail P. Progressive post-traumatic cystic and non-cystic myelopathy. Br J Neurosurg. 1994;8:7-22.
56. Falci S.P., Indeck C., Lammertse D.P. Posttraumatic spinal cord tethering and syringomyelia: surgical treatment and long-term outcome. J Neurosurg Spine. 2009;11(4):445-460.
57. Holly L.T., Johnson J.P., Masciopinto J.E., Batzdorf U. Treatment of posttraumatic syringomyelia with extradural decompressive surgery. Neurosurg Focus. 2001;8(3):E8.
58. Lyons B.M., Brown D.J., Calvert J.M., et al. The diagnosis and management of post traumatic syringomyelia. Paraplegia. 1987;25:340-350.
59. Quencer R.M., Green B.A., Eismont F.J. Post-traumatic spinal cord cysts: clinical features and characterization with metrizamide computed tomography. Radiology. 1983;146:415-423.
60. Amer T.A., el Shmam O.M. Chiari malformation type I: a new MRI classification. Magn Reson Imaging. 1997;15:397-403.
61. Milhorat T.H., Chou M.W., Trinidad E.M., et al. Chiari I malformation redefined: clinical and radiographic findings for 364 symptomatic patients. Neurosurgery. 1999;44:1005-1017.
62. Armonda R.A., Citrin C.M., Foley K.T., Ellenbogen R.G. Quantitative cine-mode magnetic resonance imaging of Chiari I malformations: an analysis of cerebrospinal fluid dynamics. Neurosurgery. 1994;35:214-224.
63. Arunkumar M.J., Korah I., Chandy M.J. Dynamic CSF flow study in the pathophysiology of syringomyelia associated with arachnoid cysts of the posterior fossa. Br J Neurosurg. 1998;12:33-36.
64. Baledent O., Gondry-Jouet C., Stoquart-Elsankari S., et al. Value of phase contrast magnetic resonance imaging for investigation of cerebral hydrodynamics. J Neuroradiol. 2006;33(5):292-303.
65. Mauer U.M., Freude G., Danz B., Kunz U. Cardiac-gated phase-contrast magnetic resonance imaging of cerebrospinal fluid flow in the diagnosis of idiopathic syringomyelia. Neurosurgery. 2008;63:1139-1144.
66. McGirt M.J., Nimjee S.M., Floyd J., et al. Correlation of cerebrospinal fluid flow dynamics and headache in Chiari I malformation. Neurosurgery. 2005;56:716-721.
67. McGirt M.J., Nimjee S.M., Fuchs H.E., George T.M. Relationship of cine phase-contrast magnetic resonance imaging with outcome after decompression for Chiari I malformation. Neurosurgery. 2006;59(1):140-146.
68. Sansur C.A., Heiss J.D., DeVroom H.L., et al. Pathophysiology of headache associated with cough in patients with Chiari I malformation. J Neurosurg. 2003;98(3):453-458.
69. Duddy M.J., Williams B. Hindbrain migration after decompression for hindbrain hernia: a quantitative assessment using MRI. Br J Neurosurg. 1991;5:141-152.
70. Firsching R., Sanker P. MRI follow-up in syringomyelia. Observations from 12 cases. Acta Neurochir. 1993;123:206-207.
71. Anderson N.E., Frith R.W., Synek V.M. Somatosensory evoked potentials in syringomyelia. J Neurol Neurosurg Psychiatry. 1986;49:1407-1410.
72. Kakigi R., Shibasaki H., Kuroda Y., et al. Pain-related somatosensory evoked potentials in syringomyelia. Brain. 1991;114:1871-1889.
73. Menezes A.H. Chiari I malformations and hydromyelia complications. Pediatr Neurosurg. 1991-1992;17:146-154.
74. Menezes A.H. Honoured guest presentation: lifetime experiences and where we are going: Chiari I with syringohydromyelia—controversies and development of decision trees. Clin Neurosurg. 2005;52:297-305.
75. Milhorat T.H., Capocelli A.L., Anzil A.P., et al. Pathological basis of spinal cord cavitation in syringomyelia: analysis of 105 autopsy cases. J Neurosurg. 1995;82:802-812.
76. Milhorat T.H., Miller J.I., Johnson W.D., et al. Anatomical basis of syringomyelia occurring with hindbrain lesions. Neurosurgery. 1993;32:748-754.
77. Milhorat T.H. Classification of syringomyelia. Neurosurg Focus. 2000;8(3):E1.
78. Peerless S.J., Durward Q.J. Management of syringomyelia: a pathophysiological approach. Clin Neurosurg. 1982;30:531-576.
79. Williams B., Sgouros S., Nenji E. Cerebrospinal fluid drainage for syringomyelia. Eur J Pediatr Surg. 1995;5(Suppl I):27-30.
80. Haines S.J., Berger M.D. Current treatment of Chiari malformations type I and II: a survey of the Pediatric Section of the American Association of Neurological Surgeons. Neurosurgery. 1991;28:353-357.
81. Anderson N.E., Willoughby E.W., Wrightson P. The natural history of syringomyelia. Clin Exp Neurol. 1986;22:71-80.
82. Samii M., Klekamp J. Surgical results of 100 intramedullary tumours in relation to accompanying syringomyelia. Neurosurgery. 1994;35:865-873.
83. Batzdorf U. Primary spinal syringomyelia. Invited submission from the joint section meeting on disorders of the spine and peripheral nerves. J Neurosurg Spine. 2005;3(6):429-435.
84. Holly L.T., Batzdorf U. Syringomyelia associated with intradural arachnoid cysts. J Neurosurg Spine. 2006;5(2):111-116.
85. Alzate J.C., Kothbauer K.F., Jallo G.I., Epstein F.J. Treatment of Chiari malformation in patients with and without syringomyelia: a consecutive series of 66 cases. Neurosurg Focus. 2001;11(1):E3.
86. Attenello F.J., McGirt M.J., Gathinji M., et al. Outcome of Chiari-associated syringomyelia after hindbrain decompression in children: analysis of 49 consecutive cases. Neurosurgery. 2008;62:1307-1313.
87. Barbaro N.M., Wilson C.B., Gutin P.H., Edwards M.S.B. Surgical treatment of syringomyelia. Favorable results with syringoperitoneal shunting. J Neurosurg. 1984;61:531-538.
88. Depreitere B., Van Calenbergh F., Van Loon J., et al. Posterior fossa decompression in syringomyelia associated with a Chiari malformation: a retrospective analysis of 22 patients. Clin Neurol Neurosurg. 2000;102:91-96.
89. Di Lorenzo N., Fortuna A., Guidetti B. Craniovertebral junction malformations. Clinicopathological findings, long-term results, and surgical indications in 63 cases. J Neurosurg. 1982;57:603-608.
90. Dyste G.N., Menezes A.H., VanGilder J.C. Symptomatic Chiari malformations. An analysis of presentation, management, and long term outcome. J Neurosurg. 1989;71:159-168.
91. Ellenbogen R.G., Armonda R.A., Shaw D.W., Winn H.R. Toward a rational treatment of Chiari I malformation and syringomyelia. Neurosurg Focus. 2000;8(3):E6.
92. Faulhauer K., Loew K. The surgical treatment of syringomyelia. Long term results. Acta Neurochir. 1978;44:215-222.
93. Hayhurst C., Richards O., Zaki H., et al. Hindbrain decompression for Chiari-syringomyelia complex: an outcome analysis comparing surgical techniques. Br J Neurosurg. 2008;22:86-91.
94. Klekamp J., Samii M. Syringomyelia. Diagnosis and Treatment. Berlin: Springer; 2002.
95. Logue V., Edwards M.R. Syringomyelia and its surgical treatment—an analysis of 75 patients. J Neurol Neurosurg Psychiatry. 1981;44:273-284.
96. Matsumoto T., Symon L. Surgical management of syringomyelia—current results. Surg Neurol. 1989;32:258-265.
97. Milhorat T.H., Johnson W.D., Miller J.I., et al. Surgical treatment of syringomyelia based on magnetic resonance imaging criteria. Neurosurgery. 1992;31:231-245.
98. Rhoton A.L. Microsurgery of Arnold-Chiari malformation in adults with and without hydromyelia. J Neurosurg. 1976;45:473-483.
99. Sahuquillo J., Rubio E., Poca M.A., et al. Posterior fossa reconstruction: a surgical technique for the treatment of Chiari I malformation and Chiari I/syringomyelia complex—preliminary results and magnetic resonance imaging quantitative assessment of hindbrain migration. Neurosurgery. 1994;35:874-884. discussion 884-885
100. Tubbs R.S., McGirt M.J., Oakes W.J. Surgical experience in 130 pediatric patients with Chiari I malformations. J Neurosurg. 2003;99:291-296.
101. Zerah M. Syringomyélie de l’enfant. [Syringomyelia in childhood.]. Neurochirurgie. 1999;45(Suppl 1):37-57. (article in French)
102. Wetjen N.M., Heiss J.D., Oldfield E.H. Time course of syringomyelia resolution following decompression of Chiari malformation type I. J Neurosurg Pediatr. 2008;1:118-123.
103. Batzdorf U., Klekamp J., Johnson J.P. A critical appraisal of syrinx cavity shunting procedures. J Neurosurg. 1998;89:382-388.
104. Tognetti F., Calbucci F. Syringomyelia: syringo-subarachnoid shunt versus posterior fossa decompression. Acta Neurochir. 1993;123:196-197.
105. Van Calenberg F., Van den Bergh R. Syringo-peritoneal shunting: results and problems in a consecutive series. Acta Neurochir. 1993;123:203-205.
106. Vaquero J., Martinez R., Salazar J., Santos H. Syringosubarachnoid shunt for treatment of syringomyelia. Acta Neurochir. 1987;84:105-109.
107. Vernet O., Farmer J.P., Montes J.L. Comparison of syringopleural and syringosubarachnoid shunting in the treatment of syringomyelia in children. J Neurosurg. 1996;84:624-628.
108. Milhorat T.H., Bolognese P.A. Tailored operative technique for Chiari type I malformation using intraoperative color Doppler ultrasonography. Neurosurgery. 2003;53:899-906.
109. Durham S.R., Fjeld-Olenec K. Comparison of posterior fossa decompression with and without duraplasty for the surgical treatment of Chiari malformation type I in pediatric patients: a meta-analysis. J Neurosurg Pediatr. 2008;2:42-49.
110. Hoffman C.E., Souweidane M.M. Cerebrospinal fluid related complications with autologous duraplasty and arachnoid sparing in type I Chiari malformation. Neurosurgery. 2008;62(3 Suppl 1):156-160.
111. Munshi I., Frim D., Stine-Reyes R., et al. Effects of posterior fossa decompression with and without duraplasty on Chiari malformation-associated hydromyelia. Neurosurgery. 2000;46:1384-1390.
112. Yundt K.D., Park T.S., Tantuwaya V.S., Kaufman B.A. Posterior fossa decompression without duraplasty in infants and young children for treatment of Chiari malformation and achondroplasia. Pediatr Neurosurg. 1996;25:221-226.
113. Fenoy A.J., Menezes A.H., Fenoy K.A. Craniocervical junction fusions in patients with hindbrain herniation and syringohydromyelia. J Neurosurg Spine. 2008;9:1-9.
114. Wang S., Wang C., Yan M., et al. Syringomyelia with irreducible atlantoaxial dislocation, basilar invagination and Chiari I malformation. Eur J Spine. 2010;19:361-366.
115. Grabb P.A., Mapstone T.B., Oakes W.J. Ventral brain stem compression in pediatric and young adult patients with Chiari I malformations. Neurosurgery. 1999;44:520-528.
116. Lesoin F., Petit H., Thomas C.E., et al. Use of the syringoperitoneal shunt in the treatment of syringomyelia. Surg Neurol. 1986;25:131-136.
117. Padovani R., Cavalo M., Gaist G. Surgical treatment of syringomyelia: favorable results with syringosubarachnoid shunting. Surg Neurol. 1989;32:173-180.
118. Philips T.W., Kindt G.W. Syringoperitoneal shunt for syringomyelia: a preliminary report. Surg Neurol. 1981;16:462-466.
119. Shannon N., Symon L., Logue V., et al. Clinical features, investigation and treatment of post-traumatic syringomyelia. J Neurol Neurosurg Psychiatry. 1981;44:35-42.
120. Tator C.H., Meguro K., Rowed D.W. Favourable results with syringosubarachnoid shunts for treatment of syringomyelia. J Neurosurg. 1982;56:517-523.
121. Wester K., Kjosavik I.F., Midgard R. Multicystic syringomyelia treated with a single, non-valved syringoperitoneal shunt. Acta Neurochir. 1989;98:148-152.
122. Williams B., Page N. Surgical treatment of syringomyelia with syringopleural shunting. Br J Neurosurg. 1987;1:63-80.
123. Klekamp J., Batzdorf U., Samii M., Bothe H.W. Treatment of syringomyelia associated with arachnoid scarring caused by arachnoiditis or trauma. J Neurosurg. 1997;86:233-240.
124. Sgouros S., Williams B. Management and outcome of post-traumatic syringomyelia. J Neurosurg. 1996;85:197-205.
125. Sgouros S., Williams B. A critical appraisal of pediculated omental graft transposition in progressive spinal cord failure. Br J Neurosurg. 1996;10:547-553.
126. Sacco D., Scott R.M. Reoperation for Chiari malformations. Pediatr Neurosurg. 2003;39:171-178.
127. Tubbs R.S., Webb D.B., Oakes W.J. Persistent syringomyelia following pediatric Chiari I decompression: radiological and surgical findings. J Neurosurg Pediatr. 2004;100(Suppl 5):460-464.
128. Cacciola F., Capozza M., Perrini P., et al. Syringopleural shunt as a rescue procedure in patients with syringomyelia refractory to restoration of cerebrospinal fluid flow. Neurosurgery. 2009;65:471-476.
129. Pollack I.F., Pang D., Albright A.L., Krieger D. Outcome following hindbrain decompression of symptomatic Chiari malformations in children previously treated with myelomeningocele closure and shunts. J Neurosurg. 1992;77:881-888.
130. Bogdanov E.I., Heiss J.D., Mendelevich E.G. The post-syrinx syndrome: stable central myelopathy and collapsed or absent syrinx. J Neurol. 2006;253:707-713.
131. Buxton N., Jaspan T., Punt J. Treatment of Chiari malformation, syringomyelia and hydrocephalus by neuroendoscopic third ventriculostomy. Minim Invasive Neurosurg. 2002;45:231-234.
132. Hayhurst C., Osman-Frah J., Das K., Mallucci C. Initial management of hydrocephalus associated with Chiari malformation type I-syringomyelia complex via endoscopic third ventriculostomy: an outcome analysis. J Neurosurg. 2008;108:1211-1214.
133. Sixt C., Riether F., Will B.E., et al. Evaluation of quality of life parameters in patients who have syringomyelia. J Clin Neurosci. 2009;16(12):1599-1603.
134. Poca M.A., Sahuquillo J., Ibanez J., et al. Intracranial hypertension after surgery in patients with Chiari I malformation and normal or moderate increase in ventricular size. Acta Neurochir Suppl. 2002;81:35-38.
135. Sgouros S., Willshaw H. Intracranial hypertension associated with Chiari I malformation. Childs Nerv Syst. 2006;22:1053-1054.
136. McLone D.G. Continuing concepts in the management of spina bifida. Pediatr Neurosci. 1992;18:254-256.
137. Caldarelli M., Di Rocco C., Colosimo C.Jr., et al. Surgical treatment of late neurological deterioration in children with myelodysplasia. Acta Neurochir (Wien). 1995;137:199-206.
138. Caldarelli M., Di Rocco C., La Marca F. Treatment of hydromyelia in spina bifida. Surg Neurol. 1998;50:411-420.
139. Craig J.J., Gray W.J., McCann J.P. The Chiari/hydrosyringomyelia complex presenting in adults with myelomeningocele: an indication for early intervention. Spinal Cord. 1999;37:275-278.
140. Koyanagi I., Iwasaki Y., Hida K., et al. Surgical treatment of syringomyelia associated with spinal dysraphism. Childs Nerv Syst. 1997;13:194-200.
141. La Marca F., Herman M., Grant J.A., McLone D.G. Presentation and management of hydromyelia in children with Chiari type-II malformation. Pediatr Neurosurg. 1997;26:57-67.
142. Rauzzino M., Oakes W.J. Chiari II malformation and syringomyelia. Neurosurg Clin North Am. 1995;6:293-309.
143. Dias M.S., McLone D.G. Hydrocephalus in the child with dysraphism. Neurosurg Clin North Am. 1993;4:715-726.
144. Tulipan N., Hernanz-Schulman M., Bruner J.P. Reduced hindbrain herniation after intrauterine myelomeningocele repair: a report of four cases. Pediatr Neurosurg. 1998;29:274-278.
145. Adzick N.S., Thom E.A., Spong C.Y., et al(MOMS Investigators). A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med. 2011;364(11):993-1004.
146. Dias M.S. Neurosurgical causes of scoliosis in patients with myelomeningocele: an evidence-based literature review. J Neurosurg. 2005;103(Suppl 1):24-35.
147. Sgouros S. Hydrocephalus with myelomeningocele. In: Cinalli G., Maixner W.J., Sainte-Rose C., editors. Pediatric Hydrocephalus. Milano: Springer-Verlag Italia; 2004:133-144.
148. Piatt J.H.Jr. Syringomyelia complicating myelomeningocele: review of the evidence. J Neurosurg Pediatr. 2004;100(Suppl 2):101-109.