CHAPTER 68 Synovectomy of the Elbow
INTRODUCTION
Rheumatoid arthritis affects 1% to 2% of the general population.53 The most common cause of elbow arthritis is rheumatoid arthritis in which the involvement of elbow after an average of at least 10 years can be seen in more than half of the patients clinically or radiologically.17,25,27 Medical management is discussed in detail in Chapters 74 and 75. The mainstays of surgical treatment available for the patient with rheumatoid arthritis of the elbow include synovectomy, interposition arthroplasty, and total elbow replacement, in addition to other treatment options with limited application like arthrodesis and resection arthroplasty. Joint replacements and interposition arthroplasty are considered in Chapters 54, 55, and 69. Synovectomy with or without radial head excision is a well-recognized and accepted form of treatment for the rheumatoid elbow. This procedure reduces the amount of joint fluid and removes proliferative synovitis, and thereby decreases intra-articular pressure, relieves pain, and reduces swelling. After a few months, a new synovial membrane is regenerated in the joint5; however, the lack of villous change, vasculitis, and decreased pathologic enzymatic activity in the new synovial membrane and the joint fluid34 indicates a difference in the inflammatory process after synovectomy.38 Still, the role of synovectomy must be defined in the context of the success of total elbow replacement. The primary indication for elbow synovectomy in a patient with rheumatoid arthritis is persistent painful synovitis that is unresponsive to at least 6 months of appropriate medical management as an initial interventive procedure. Despite this, controversy still remains as to the role and method of execution, especially in advanced stages and in patients with instability and stiffness. This chapter highlights the issues of open versus arthroscopic techniques and the resection versus preservation of the radial head during elbow synovectomy.
INDICATIONS AND PATIENT SELECTION
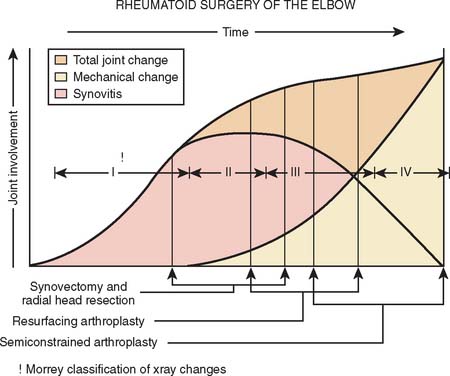
Synovectomy is ideal for the patients who present with uncontrolled synovitis resulting in a painful elbow with limited function. However, a period of nonsurgical treatment including anti-inflammatory agents, steroids, disease-modifying anti-rheumatic drugs in addition to maintaining supple joints with an active range of motion program and splinting for at least 6 months should be attempted before surgery is considered4 (see Chapter 54). Early in the disease, synovitis is a prominent feature (Fig. 68-1). A warm, swollen elbow with a mild flexion contracture and a painful limitation of flexion and extension in addition to pronation and supination characterizes a typical joint. As the disease progresses, the synovitis generally wanes and persistent pain and stiffness results from joint destruction with articular incongruity.
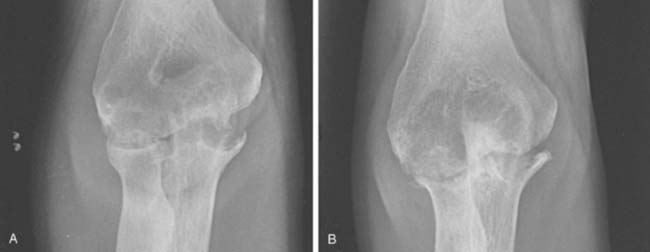
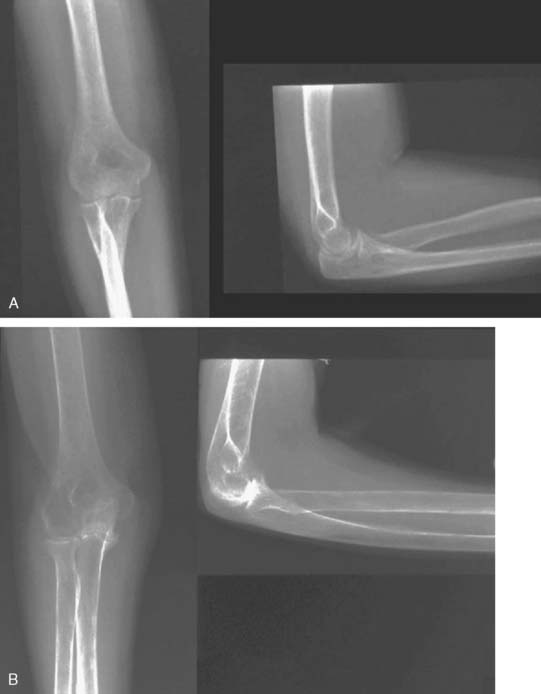
Although classically the disease stage employs the Carson system, for our purposes, it is convenient to describe the radiographic appearance into five categories. Type I: synovitis with a normal appearing joint; type II: loss of joint space but maintenance of the subchondral architecture; type IIIA: alteration of the subchondral architecture; type IIIB: alteration of the architecture with deformity; type IV: gross deformity; type V: radiographic appearance of ankylosis (Fig. 68-2).

FIGURE 68-2 A, Mayo radiographic classification of rheumatoid involvement of the elbow considers synovitis, articular involvement, and joint distraction (see text). B, A type V radiographic presentation is one of ankylosis, as reported by Connor and associates.6
This classification is helpful in providing a basis for treatment options (see Fig. 68-1). Elbow synovectomy is ideally reserved for the early stages of the disease (type I, type II, and early type IIIA) (Fig. 68-3).
Synovectomy per se is not effective or reliable in restoring motion. As a result, a functional arc (30 to 130 degrees of flexion) should ideally be present.33 In patients with a long-standing and advanced disease, this arc is often not present. Therefore, a total arc of flexion of at least 80 degrees is recommended before the procedure. However, more recently, it has been shown that with anterior and posterior capsular release or capsulectomy, a better outcome may be possible even in those with less than 80 degrees of flexion.28,41
The role of synovectomy in more advanced stages of disease is still debatable in the literature. In advanced stages of the disease, damage to either or both the medial and lateral ligamentous complexes combined with bony and cartilaginous loss in addition to significant erosion and instability of the radial head may result in gross medial-lateral elbow instability, precluding synovectomy. This is an indication for total elbow arthroplasty, which can be reliable even in the presence of instability.6,14,32 Critical assessment of prior reports reveal a small number of articles that report worsening of the results over the long term, especially due to the development of instability.10,50 On the other hand, the majority of reports agree that advanced radiographic stage of the disease might not influence the ultimate outcome* (Fig. 68-4). Furthermore, although instability can be seen in up to 50% of patients in the advanced stages,40 this generally does not seem to cause symptomatic instability requiring an operation.† As a result, synovectomy might be employed with reservations in advanced stages as well if instability is not one of the major complaints of the patient. Nevertheless, those experienced with the techniques of total elbow replacement as well as synovectomy, and those who are familiar with the results of both, favor total elbow replacement to synovectomy in treating later stages of the disease because patients are more satisfied, functional improvement is greater, and the results are more predictable.6,14,32
CONTRAINDICATIONS
One of the major contraindications to synovectomy is severe joint disruption. Synovectomy performed in this situation will not correct instability, and débridement of the joint may actually aggravate instability, particularly when radial head excision is performed. In the series of Rymaszewski and colleagues,40 most of the displeased patients had medial tenderness and pain with attempted valgus stress in the elbow, which was attributed to tension on medial collateral ligaments, mainly due to resection of the radial head. Also, the initial good results may deteriorate with time with increasing instability of the joints due to gradual bone loss.50
Limited elbow motion is the other major contraindication for synovectomy of the elbow, because elbow function cannot predictably be improved, and some patients lose some motion. Severe joint stiffness resulting from inflammatory fibroarthrosis is more commonly seen in juvenile rheumatoid arthritis. Because complete ankylosis can be observed in these patients, grade 5 radiologic classification was added to the original classification of the rheumatoid arthritis6 (see Fig. 68-2). Synovectomy alone cannot be advocated in this subgroup of patients for the sole purpose of improving motion.30 Radiographic involvement of the joint architecture with deformity (type IIIB) is also a relative contraindication.
TECHNIQUES
Synovectomy can be performed nonsurgically (chemical or radiation synovectomy)8,15,37,44 or surgically, which can be performed either open or by an arthroscopic technique.‡
NONSURGICAL SYNOVECTOMY
Chemical and radiation synovectomy has been advocated as a noninvasive procedure. Owing to the size and subcutaneous surface of the joint, rhenium-186,15 yttrium-90,44 and osmic acid37 have been used with caution at the elbow. Although patients with early radiologic stages of elbow involvement have a better success rate, especially with the addition of triamcinolone to radiosynovectomy, the overall success rate is less than 50% with these agents with a very limited follow-up.15,44
The potential for cartilage necrosis and the subcutaneous location of this joint has limited the use of these agents in the United States.16,31 Also, radial head excision, if needed, is not possible. Besides, in marked synovitis in which synovial swelling is above the effective penetration range of the radionuclide, the lower layers of synovium cannot be reached by radiosynoviorthesis and the destruction process and pain will continue.15 However, this technique can be considered as a more conservative treatment option to surgical synovectomy, especially in patients who are unable to undergo surgery.
SURGICAL SYNOVECTOMY
ARTHROTOMY
Although there are an increasing number of reports on arthroscopic synovectomy, open surgery is still commonly performed for elbow synovectomy. This technique is well established and requires less technical expertise than arthroscopic synovectomy, particularly when radial head excision is performed. However, more remarkable postoperative pain, increased risk of wound breakdown, and increased risk of infection, in addition to loss of ligamentous or muscle and tissue supports require a delay in the initiation of rehabilitation, which might potentially result in elbow stiffness.3,21
Technique
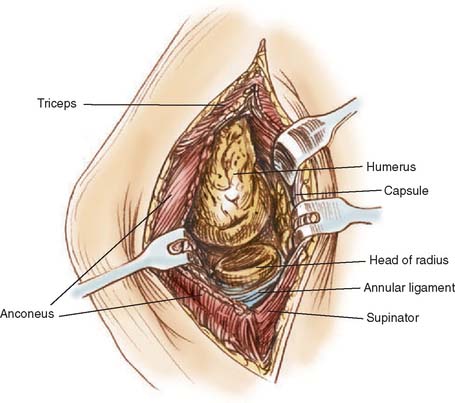
An extensile Kocher approach provides excellent visualization of the lateral joint and preserves the medial collateral ligaments (Fig. 68-5). The radial head is removed if there are significant symptoms with pronation and supination or marked radial humeral joint pain with flexion and extension. The synovitis typically involves the sacriform recess of the radial neck and a thorough synovectomy of this region is required. If the radial head is removed, a very thorough synovectomy can be carried out.2,13,18,22,39,50,54 If radial head is preserved anterior compartment exposure is more difficult but can still be adequately achieved. A second medial exposure is not necessary in our experience and that of most of the investigators.§ The triceps is elevated from the lateral column and the joint is extended. The posterior compartment synovectomy can then be carried out.
Because a complete synovectomy can be achieved through the extensile Kocher approach, separate lateral and medial approaches have been advocated sporadically.7,39,50 The main advantage of adding a medial incision is that radial head need not be resected for adequate synovectomy.7 However, even in bilateral approach proponents, it has been noted that if an extended lateral approach is used, results do not differ.39 In various reports, a medial incision is also added to an extended lateral approach in several cases because of the need for the decompression and translocation of the ulnar nerve.3,26,49,54 The use of Mayo posteromedial triceps reflecting exposure has also been advocated for synovectomy of the elbow.20 It provides for identification of the ulnar nerve and facilitates subsequent skin incision for total elbow replacement. However, surgery is more extensive than the extensile Kocher approach with the added potential for extensor mechanism complications, and we have not found it necessary to use this approach for routine synovectomy. Synovectomy and débri-dement through a transolecranon approach is contraindicated.21
ARTHROSCOPIC SYNOVECTOMY
Arthroscopy is being used with increasing frequency to diagnose and treat elbow disorders. Because elbow arthroscopy has become popular in recent years, concern regarding potential complications, including septic arthritis, superficial skin infection, persistent drainage from portal sites, and most frequently, nerve injuries (transient and permanent), has also risen23 (see Chapters 40 and 41). The risk can be minimized with observation of certain safety precautions. In our series, of all procedures, it was found that two factors were associated with a higher risk of nerve palsy–the performance of capsular release and the diagnosis of rheumatoid arthritis.23 In experienced hands, the advantages of arthroscopic over open synovectomy are obvious. It can be performed on an out-patient basis, causes minimal morbidity (decreased scarring, decreased risk of infection, less postoperative pain), possibly enables a more thorough visualization of the elbow joint than is possible with an arthrotomy during some procedures, results in rapid return of motion, and shortens the recovery period.23 With improved technique and greater experience, a complete synovectomy including excision of the radial head, if necessary, is possible (see Chapter 40).
Technique
Several strategies can be used and our technique of elbow arthroscopy has evolved.36 Patients are placed in the lateral decubitus position, with the involved elbow over a padded bolster. The forearm is allowed to swing free, and the elbow is flexed to 90 degrees (Fig. 68-6). The arm is then prepared in the usual fashion. The forearm is exsanguinated by elevating the limb. A soft elastic bandage is then wrapped around the hand and forearm to within 10 cm of the olecranon. The tourniquet, which is used routinely, is inflated to 250 mmHg. The elastic bandage is left on until the end of the procedure, to limit the periarticular swelling to the elbow area. At the end of the procedure, the bandage and the tourniquet are removed and any accumulated edema rapidly dissipates into the tissues of the forearm and arm.
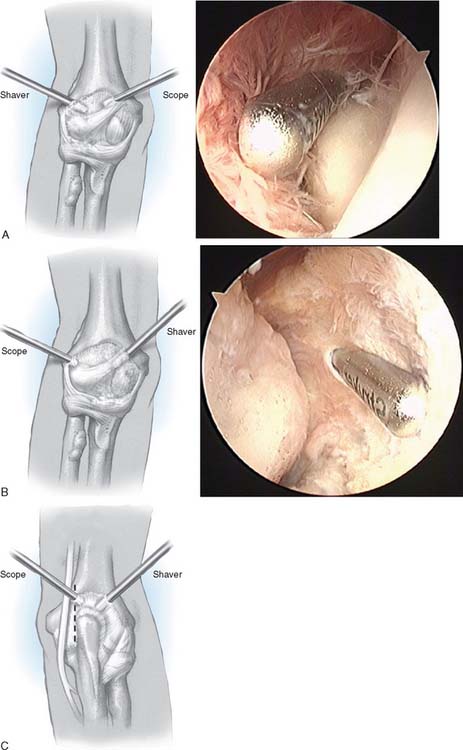
We begin the procedure by visualization through anteromedial portal (Fig. 68-7). Somewhat more proximal than the standard anteromedial portal, this increases nerve-to-portal distance and minimizes the amount of manipulation through the bulky muscles of the flexor pronator origin. An 18-gauge needle helps determine the optimal site for this portal. Portal placement has been accomplished with both the outside-in and the inside-out technique, but over time, the outside-in technique has been preferred. Emphasis is placed on using the retractors through proximal anterolateral and distal anteromedial portals. These portals are primarily used for visualization in the anterior compartments instead of pressurization to accomplish joint distension. This reduces the risk of edema and allows more complex surgical procedures to be performed. The débriding instrument is a 4-mm reciprocating device with outflow to gravity inserted through an anterior/lateral portal.
Synovitis can be extensive, and visualization improves as removal of synovium proceeds. The tip of the resector must be in view at all times and closed immediately if muscle fibers are seen or if the cutting head disappears from view. The shaver blade should always point inward and away from the capsule which is often extremely thin in rheumatoid arthritis. With the help of a switch stick, the débriding instrument is introduced to anteromedial portal and an anterior synovectomy is completed (see Fig. 68-7B).
Considerable visualization of the posterior compartment can usually be achieved through the midlateral posterior portal. A posterior synovectomy is completed by inserting the débriding instrument through a posterolateral portal (see Fig. 68-7C). The instrument can then be switched (with the arthroscope in the posterolateral and shaver in the midlateral portal) to facilitate removal of synovium in the sacriform recess and removal of radial head when indicated.
RESULTS
OPEN SYNOVECTOMY
Surveillance
Considering recognized inconsistencies inherent in summarizing diverse reports using different evaluation standards, 71% to 93% of the procedures can be considered to have a satisfactory outcome in short to intermediate term. The rate of repeat synovectomy, resurfacing arthroplasty, or conversion to total elbow replacement in these patients occurs in up to 10%.2,7,21,22,26,39 The long-term results of open elbow synovectomy are summarized in Table 68-1.
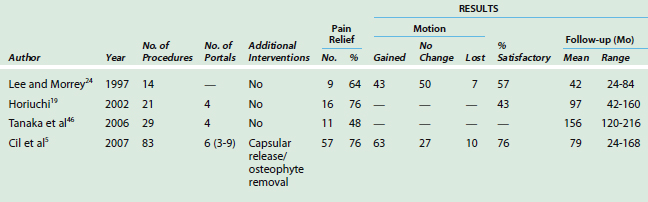
TABLE 68-1 Results of Elbow Synovectomy for Rheumatoid Arthritis (Open Procedures, Average Follow-up >5 years)
Some reports suggest that results deteriorate minimally with time.7,8,26,41,49 In a study by Herold and Schroeder18 in 11 patients (12 elbows) at 14 years after the surgery, 83% maintained satisfactory pain relief, however, radiographic progression was noted and reoperation was required in two elbows. In another long-term study with follow-up averaging 10 to 20 years, only 67% of 21 patients were satisfied with the procedure.1 Others with surveillance averaging 7 to 8 years reported initial satisfactory results of 90% had decreased to less than 75% at final assessment.43,50 Gendi and associates13 reported a large series of 113 elbows 5 to 20 years after synovectomy and noted a cumulative survival rate of 81% at 1 year, decreasing an average of 2.6% per year. By final follow-up, 46% of the procedures had failed. There is a tendency toward failure to appear after 3 years of follow-up.39,45 Rymaszewski and colleagues40 noted 25% of the patients with initial good pain relief deteriorated after an average of 6 years of follow-up. Many reoperations occur within the first 5 years3,12,29,40 but failure is seen with increasing frequency after 8 to 9 years.12,18,46,50 Clearly there are no data to suggest that synovectomy arrests the progress of disease process.
RADIAL HEAD
The value of radial head resection continues to be debated. Although most series report radial head excision in the majority of their cases,¶ more recent results suggest that its preservation can reliably achieve comparable results with pain relief in 70% to 83% of the patients even at about 9 to 13 years of follow-up.29,43,46,49 The majority maintain or regain a functional arc of motion, with approximately 50% improving flexion and extension, 30 to 35% remaining unchanged, and 15% losing a small amount of motion. When capsular release or capsulectomy is done in addition to open synovectomy, a significant increase in flexion arc, particularly originating from gain in extension had been shown in the vast majority of the patients in two studies.28,41 Although pronation and supination is also a function of wrist joint which is usually involved, gain in forearm rotation is regularly noted.¶
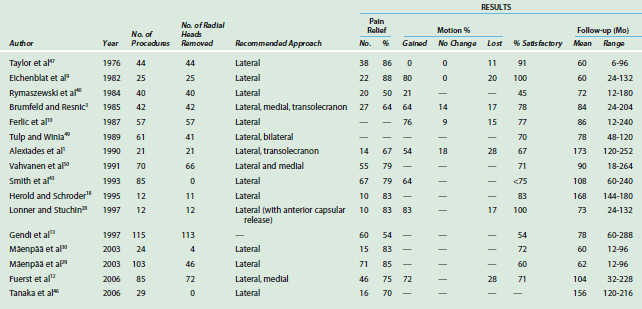
ARTHROSCOPIC SYNOVECTOMY
Surveillance
There is still a dearth of reports regarding the results of arthroscopic synovectomy (Table 68-2). Horiuchi and colleagues19 reported on 20 patients with a mean follow-up of 8 years. Similar to the trend seen in open synovectomies and our initial report on arthroscopic synovectomies,24 71% of satisfactory results at 2 years decreased to 43% at the final follow-up. Also, clinically apparent synovitis occurred in 24% of the elbows, with two of them requiring total elbow replacement. However, these authors did not débride the medial gutter and did not perform osteophyte excision or capsular release. Furthermore, they had reported favorable results mainly in patients with early-stage disease. Tanaka and colleagues46 recently observed similar results with 48% pain relief at an average follow-up of 13 years in 29 elbows. They compared these results with a matched group of open synovectomies and detected no significant difference between the overall clinical results of both procedures. However, especially in elbows with a limited preoperative arc of flexion (<90 degrees), arthroscopic synovectomy provided significantly better function than open surgery after mid-term follow-up, and motion and function continued to be better in those patients at the most recent follow-up evaluation.
MAYO EXPERIENCE
We recently updated the results of our initial assessment of arthroscopic synovectomy in 83 elbows with an average follow-up of 6.5 years (2 to 14 years).24 Pain relief was observed in 76%, with a satisfaction rate of 76%. Unlike the techniques employed in the past, we also performed capsular release and/or capsulectomy in two thirds of our patients and osteophyte excision in one half, along with medial gutter synovectomy. This technique required an average of six portals, but the arc of flexion increased from 91 degrees to 119 degrees, with an average gain in flexion of 10 degrees and extension of 18 degrees. Eight patients (10%) required total elbow replacement, leaving 80% free of total elbow replacement at 14 years; this is comparable to open synovectomy (Fig. 68-8).
REPEAT SYNOVECTOMY
Repeat synovectomy following an initial failed procedure has occasionally been recommended. The frequency of performing repeat synovectomy has been reported to be between 1% to 20%12,13,18,29,30,43,45,50 after open procedures and 6% to 9%5,35 after arthroscopic synovectomy. Most repeat synovectomies are performed within 3 years after the index operation,5,21 indicating a lack of initial satisfactory response.12,50 Because the results of repeat synovectomy following a return of symptoms is less predictable, other successful alternatives such as total elbow replacement or interposition arthroplasty should be considered in case of a failure6,14,32 (see Chapters 54 and 69).
TOTAL ELBOW REPLACEMENT FOR FAILED SYNOVECTOMY
Schemitsch and colleagues42 compared patients undergoing capitellocondylar total elbow replacements with patients who had a failed open synovectomy and radial head excision. The rate of complication, reoperations, and postoperative instability was higher in patients with previous synovectomy procedures with an average follow-up of 4 years. Fink and colleagues11 found a higher complication rate as well as a higher rate of loosening, especially in patients with previous distraction interposition arthroplasty in addition to previous open synovectomies. However, van der Lugt and colleagues51 demonstrated no increased rate of complications after a previous radial head resection and open synovectomy and no effect on the long-term functional outcome and survival an unlinked implant. In our assessment of the Coonrad/Morrey replacement after synovectomy and radial head excision, similar outcomes were documented compared with a control group.52 Yet, open synovectomy and radial head excision, although not associated with any increased rate of revision following subsequent arthroplasty of the elbow, do increase slightly the risk of complications.52
COMPLICATIONS
Motion Loss
Loss of motion, as noted earlier, can occur in 10% to 20% of patients. These problems are less commonly seen in those with clear indications for the procedure initially. More important, arthroscopic synovectomy and early aggressive motion facilitate early motion and appear to eliminate the tendency for motion loss after synovectomy.5
Instability
Residual instability has been reported in about 15% of the patients.48 The incidence is higher, up to 50%, in patients with more advanced disease and in those with significant instability before synovectomy.40 This is particularly true if radial head excision is performed in patients with pre-existing instability. Instability is not a common problem, even with radial head excision, if the ulnohumeral joint is reasonably intact and if the medial collateral ligament is also competent.
Neuropathy
Nerve injury is rare after open synovectomy but is a significant potential risk with arthroscopic synovectomy given the fact that the neurovascular structures lie very closely to the joint capsule.23 The risk of neurovascular injury is always a concern and a significant disadvantage especially in patients with rheumatoid arthritis with limited range of motion.19,23,24,35,46 This is particularly true with anterior or posterior capsulectomy. Hence, the operating surgeon must either be able to identify the radial or ulnar nerve at the time of capsulectomy or have sufficient experience with this procedure and knowledge of the neural anatomy in relation to capsule and intra-articular structures so that such visualization of the nerves is not necessary. Temporary ulnar nerve neuropraxia occurred in one patient (7%) in our initial report24; two ulnar nerve neuropraxias and one median nerve neuropraxia accounted for a 4% frequency in the updated series.5
1 Alexiades M.M., Stanwyck T.S., Figgie M.P., Inglis A.E. Minimum ten-year follow-up of elbow synovectomy for rheumatoid arthritis. Orthop. Trans. 1990;14:255.
2 Brattstrom H., Al Khudairy H. Synovectomy of the elbow in rheumatoid arthritis. Acta Orthop. Scand. 1975;46:744.
3 Brumfield R.H.Jr, Resnick C.T. Synovectomy of the elbow in rheumatoid arthritis. J. Bone Joint Surg.. 1985;67A:16.
4 Bryan R.S., Morrey B.F.. Rheumatoid arthritis of the elbow. Evarts C.M., editor. Surgery of the Musculoskeletal System, 2nd ed., Vol. 2. London: Churchill Livingstone, 1990;1759.
5 Cil, A., Morrey, B. F., and O’Driscoll, S.: Arthroscopic synovectomy of the elbow: An update with improved surgical technique. (In press.)
6 Connor P.M., Morrey B.F. Total elbow arthroplasty in patients who have juvenile rheumatoid arthritis. J. Bone Joint Surg. 1998;80A:678.
7 Copeland S.A., Taylor J.G. Synovectomy of the elbow in rheumatoid arthritis. J. Bone Joint Surg. 1979;61B:69.
8 Dawson T.M., Ryan P.F., Street A.M., Robertson P.L., Kalff V., Kelly M.J., Cicuttini F.M. Yttrium synovectomy in haemophilic arthropathy. Br. J. Rheumatol. 1994;33:351.
9 Eichenblat M., Hass A., Kessler I., Israel R. Synovectomy of the elbow in rheumatoid arthritis. J. Bone Joint Surg. 1982;64A:1074.
10 Ferlic D.C., Patchett C.E., Clayton M.L., Freeman A.C. Elbow synovectomy in rheumatoid arthritis: Long-term results. Clin. Orthop. 1987;220:119.
11 Fink B., Krey D., Schmielau G., Tillmann K., Rüther W. Results of elbow endoprostheses in patients with rheumatoid arthritis in correlation with previous operations. J. Shoulder Elbow Surg. 2002;11:360.
12 Fuerst J., Fink B., Futher W. Survival analysis and long-term results of elbow synovectomy in rheumatoid arthritis. J. Rheumatol. 2006;33:892.
13 Gendi N.S.T., Axon J.M.C., Carr A.J., Pile K.D., Burge P.D., Mowat A.G. Synovectomy of the elbow and radial head excision in rheumatoid arthritis. Predictive factors and long-term outcome. J. Bone Joint Surg. 1997;79B:918.
14 Gill D.R.J., Morrey B.F. The Coonrad-Morrey total elbow arthroplasty in patients who have rheumatoid arthritis. J. Bone Joint Surg. 1998;80A:1327.
15 Gobel D., von Rothkirch G.-T., Becker W. Radiosynoviorthesis with rhenium-186 in rheumatoid arthritis: A prospective study of three treatment regimens. Rheumatol. Int. 1997;17:105.
16 Goldberg V.M., Rashbaum R., Zika J. The role of osmic acid in the treatment of immune synovitis. Arthritis Rheum. 1976;19:737.
17 Gschwend N. Operations in the repair of the elbow joint. In: Gschwend N., editor. Surgical Treatment of Rheumatoid Arthritis. New York: Georg Thieme Verlag; 1980:45.
18 Herold N., Schroder H.A. Synovectomy and radial head excision in rheumatoid arthritis: 11 patients followed for 14 years. Acta Orthop. Scand. 1995;66:252.
19 Horiuchi W., Momohara S., Tomatsu T., Inoue K., Toyama Y. Arthroscopic synovectomy of the elbow in rheumatoid arthritis. J. Bone Joint Surg. 2002;84A:342.
20 Inglis A.E., Figgie M.P. Septic and non-traumatic conditions of the elbow. In: Morrey B.F., editor. The Elbow and Its Disorders. 2nd ed. Philadelphia: W. B. Saunders; 1993:759.
21 Inglis A.E., Ranawat C.S., Straub L.R. Synovectomy and debridement of the elbow in rheumatoid arthritis. J. Bone Joint Surg. 1971;53A:652.
22 Jensen C.M., Rasmussen S.W., Haugegaard M., Melchior T.M., Hansen H. Elbow synovectomy in rheumatoid arthritis. Acta Orthop. Belg. 1996;62:144.
23 Kelly E.W., Morrey B.F., O’Driscoll S.W. Complications of elbow arthroscopy. J. Bone Joint Surg. 2001;83A:25.
24 Lee B.P.H., Morrey B.F. Arthroscopic synovectomy of the elbow for rheumatoid arthritis. A prospective study. J. Bone Joint Surg. 1997;79B:770.
25 Lehtinen J.T., Kaarela K., Ikavälko M., Kauppi M.J., Belt E.A., Kuusela P.P., Kautiainen H.J., Lehto M.U. Incidence of elbow involvement in rheumatoid arthritis. A 15 year endpoint study. J. Rheumatol. 2001;28:70.
26 Linclau L.A., Winia W.P., Korts J.K. Synovectomy of the elbow in rheumatoid arthritis. Acta Orthop. Scand. 1983;54:935.
27 Ljung P., Jonsson K., Rydgren L., Rydholm U. The natural course of rheumatoid elbow arthritis: A radiographic and clinical five-year follow-up. J. Orthop. Rheumatol. 1995;8:32.
28 Lonner J.H., Stuchin S.A. Synovectomy, radial head excision, and anterior capsular release in stage III inflammatory arthritis of the elbow. J. Hand Surg. 1997;22A:279.
29 Mäenpää H.M., Kuusela P.P., Kaarela K., Kautiainen H.J., Lehtinen J.T., Belt E.A. Reoperation rate after elbow synovectomy in rheumatoid arthritis. J. Shoulder Elbow Surg. 2003;12:480.
30 Mäenpää H.M., Kuusela P.P., Lehtinen J.T., Savolainen A., Kautiainen H., Belt E. Elbow synovectomy on patients with juvenile rheumatoid arthritis. Clin. Orthop. Relat. Res. 2003;412:65.
31 Mitchel N., Laurin C., Shepard N. The effect of osmium tetroxide and nitrogen mustard on normal articular cartilage. J. Bone Joint Surg. 1973;55B:814.
32 Morrey B.F., Adams R.A. Semiconstrained arthroplasty for the treatment of rheumatoid arthritis of the elbow. J. Bone Joint Surg. 1992;74A:479.
33 Morrey B.F., Askew L.J., An K.N., Chao E.Y. A biomechanical study of normal functional elbow motion. J. Bone Joint Surg. 1981;63A:872.
34 Myllyla T., Peltonen L., Puranen J., Korhonen L. Consequences of synovectomy of the knee joint, clinical, histopathological and enzymatic changes and changes in 2 components of complement. Ann. Rheum. Dis. 1983;42:28.
35 Nemoto K., Arino H., Yoshihara Y., Fujikawa K. Arthroscopic synovectomy for the rheumatoid elbow: A short term outcome. J. Shoulder Elbow Surg. 2004;13:652.
36 O’Driscoll S.W., Morrey B.F. Arthroscopy of the elbow: Diagnostic and therapeutic benefits and hazards. J. Bone Joint Surg. 1992;74A:84.
37 Oka M., Rekonen A., Ruotsi A. The rate and distribution of intra-articularly injected osmium tetroxide (os-191). Acta Rheum. 1969;15:35.
38 Paus A., Refsum S., Forre O. Histopathologic changes in arthroscopic synovial biopsies before and after open synovectomy in patients with chronic inflammatory joint diseases. Scand. J Rheumatol. 1990;19:202.
39 Porter B.B., Park N., Richardson C., Vainio K. Rheumatoid arthritis of the elbow: The results of synovectomy. J. Bone Joint Surg. 1974;56B:427.
40 Rymaszewski L.A., Mackay I., Amis A.A., Miller J.H. Long-term effects of excision of the radial head in rheumatoid arthritis. J. Bone Joint Surg. 1984;66B:109.
41 Saito T., Koshino T., Okamoto R., Horiuchi S. Radical synovectomy with muscle release for the rheumatoid elbow. Acta Orthop. Scand. 1986;57:71.
42 Schemitsch E.H., Ewald F.C., Thornhill T.S. Results of total elbow arthroplasty after excision of the radial head and synovectomy in patients who had rheumatoid arthritis. J. Bone Joint Surg. 1996;78A:1541.
43 Smith S.R., Pinder I.M., Ang S.C. Elbow synovectomy in rheumatoid arthritis: Present role and value of repeat synovectomy. J. Orthop Rheumatol. 1993;6:155.
44 Stucki G., Bozzone P., Treuer E., Wassmer P., Felder M. Efficacy and safety of radiation synovectomy with yttrium-90: A retrospective long-term analysis of 164 applications in 82 patients. Br. J. Rheumatol. 1993;32:383.
45 Summers G.D., Taylor A.R., Webley M. Elbow synovectomy and excision of the radial head in rheumatoid arthritis: A short term palliative procedure. J. Rheumatol. 1988;15:566.
46 Tanaka N., Sakahashi H., Hirose K., Ishima T., Ishiim S. Arthroscopic and open synovectomy of the elbow in rheumatoid arthritis. J. Bone Joint Surg. 2006;88A:521.
47 Taylor A.R., Mukerjea S.K., Rana N.A. Excision of the head of the radius in rheumatoid arthritis. J. Bone Joint Surg. 1976;58B:485.
48 Torgerson W.R., Leach R.E. Synovectomy of the elbow in rheumatoid arthritis: Long-term results. J. Bone Joint Surg. 1989;71B:664.
49 Tulp J.J.A., Winia W.P. Synovectomy of the elbow in rheumatoid arthritis: Long-term results. J. Bone Joint Surg. 1989;71B:664.
50 Vahvanen V., Eskola A., Peltonen J. Results of synovectomy in rheumatoid arthritis. Arch. Orthop. Trauma Surg. 1991;110:151.
51 van der Lugt J.C.T., Geskus R.B., Rozing P.M. Influence of previous open synovectomy on the outcome of Souter-Strathclyde total elbow prosthesis. Rheumatology. 2004;43:1240.
52 Whaley A., Morrey B.F., Adams R. Total elbow arthroplasty after previous resection of the radial head and synovectomy. J. Bone Joint Surg. 2005;87B:47.
53 Wolfe A.M. The epidemiology of rheumatoid arthritis: A review. Bull. Rheum. Dis. 1968;19:518.
54 Woods D.A., Williams J.R., Gendi N.S.T., Mowat A.G., Burge P.D., Carr A.J. Surgery for rheumatoid arthritis of the elbow: A comparison of radial-head excision and synovectomy with total elbow replacement. J. Shoulder Elbow Surg. 1999;8:291.
* See references 2, 3, 7, 9, 12, 13, 18, 22, 26, 28–30, 35, 39–41, 45, and 49.
† See references 2, 7, 9, 10, 18, 21–23, 26, 28, 39, 41, 45, 49, and 54.
‡ See references 2, 3, 7, 9, 10, 12, 13, 18, 19, 21, 22, 24, 26, 28–30, 35, 39–41, 45, 46, and 49.
§ See references 2, 9, 10, 18, 22, 28–30, 41, and 46.
¶ See references 1, 3, 9, 10, 12, 18, 28, 40, 43, 47, and 50.
¶ See references 3, 7, 9, 10, 12, 18, 28, 40, 43, 45, 46, and 50.