CHAPTER 28 Suture suspension for brow and upper face
History
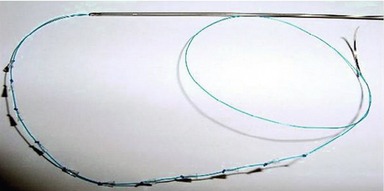
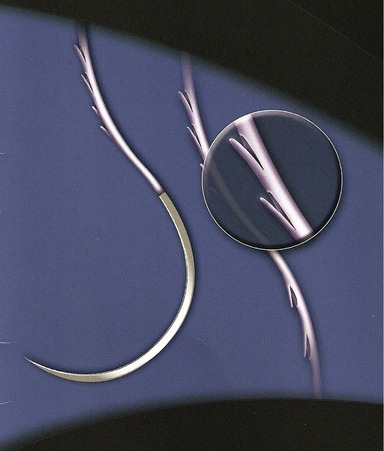
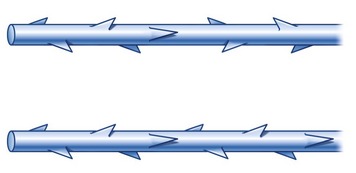
Both barbed suture design and treatment have evolved since their introduction. The original APTOS suture was a multiple-dented suture meant to provide additional traction in tissue. This design was modified to be bi-directional, with the barbs oriented so that tissue would be retained in the central region of the suture without the need for anchoring at either end (Fig. 28.1A). It was then re-designed as a multiple-barbed polypropylene suture intended to provide traction and suspension unidirectionally (Fig. 28.1B). Approval from the FDA for the extended length unidirectional barbed suture was obtained by two different companies in 2004 and 2005, respectively. No other variant of the barbed suture has received approval, but a newer technology called the Silhouette suture (Figs 28.1, Fig. 28.2), which involves the use of clear, flexible, absorbable cones with accompanying small knots on a polypropylene thread, to allow for more effective soft tissue elevation, received FDA approval in November 2006.
Physical evaluation
Closed suture suspension of the brow
In the brow area there is questionable longevity because of the amount of tissue excursion that naturally occurs in this area, but it does provide a non-surgical alternative. The technique is best supplemented with Botox injections before the procedure and also continuing afterwards in order to relax the frontalis, corrugator, and lateral orbicularis muscles to decrease dynamic activity. In a presentation by Dr Nicanor Isse at the American Society of Plastic Surgery in New Orleans in 2005, his review of cases showed a 70% failure rate of brow suture suspension. Patients who might be considered good candidates would be those with mild bilateral brow ptosis with very modest expectations and accepting of an uncertain, but limited, longevity, and who wished to avoid a more extensive surgical procedure. Also, patients who have unilateral ptosis either due to facial asymmetry or neuropraxia of the temporal branch of the facial nerve, occurring after a previous surgery, may find this as a means of temporarily improving facial symmetry while awaiting return of nerve regeneration. In some patients who have a more pronounced soft tissue glide plane after open or endoscopic surgery, brow elevation with threads may provide a modest, but temporary, improvement, with a much less invasive procedure.
Closed suture suspension of midface (closed melopexy)
In considering facial rejuvenation, there are four main areas where correction is required:
The closed midface melopexy only minimally improves tissue descent and volume loss and does nothing for muscle-induced lines or skin changes. Rating each of these areas on a scale of 1 to 4 with the highest score being 4, closed suture suspension provides for tissue descent at best at 0.5 and volume lost at best 0.5 (Table 28.1). It provides no effect on muscle-induced lines or skin changes, giving it a total of one out of four or 25%. For this reason, I call this the 25% rule or 25% lift, meaning that the closed melopexy with sutures provides a 25% improvement with the mini–open face lift, 25% of recovery, 25% of duration, and 25% of cost (Table 28.2). There is an important reason for the disappointing outcome. Suture lifting or suture traction by the threads lifts only the soft tissue which has not previously been dissected. For truly effective lifting to occur, tissue dissection needs to be performed so that tissues can be transposed and anchored under less tension, maintaining the lift until the tissue planes have healed in their new position. In summary, the results are not long-lasting, but they do provide a solution for certain unique situations.
| Tissue descent | 0.5 |
| Volume loss | 0.5 |
| Muscle induced lines | 0.0 |
| Skin changes | 0.0 |
| 25% | 1 out of 4 |
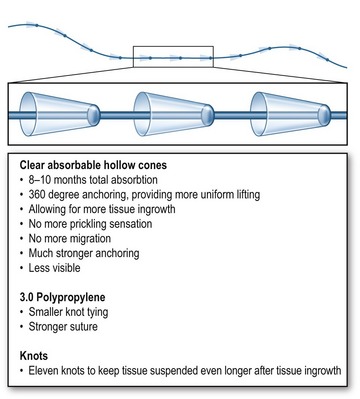
The new Silhouette suture is stronger than the conventional barbed sutures, it stands less chance of breakage, and it interacts with normal tissues through surrounding collagen tissue formation for better results. The suture consists of a 25 cm long 3-0 non-absorbable polypropylene suture that is 50% thinner than the 2-0 used in the design of the barbed sutures. This decreases knot palpability and pain in the temporal area. Suture strength is maintained by avoiding oblique cuts in the suture, in order to create the “barbs” (30–50% loss of suture strength). Each suture holds 11 clear, flexible, absorbable hollow cones that allow for tissue growth inside and around the cones (co-polymer of glycolic acid and lactic acid) (see Fig. 28.2). An immediate anchoring effect is created by the cones. A delayed anchoring effect is produced by a series of knots created on the distal 10 cm of the suture, which is intercolated with the cones (Fig. 28.3). The knots control the position of the cones and create further anchoring of the soft tissue, in turn creating collagen deposition around and inside each loop of the knot. These sutures can easily and safely be removed after the cones are completely absorbed using a small microphlebectomy hook.
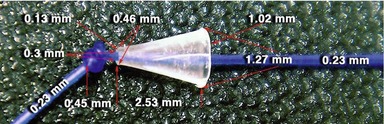
The co-polymer cones (Fig. 28.4) are soft and avoid the pinprick effects of the barbed suture. Their large size (1.0 mm × 2.5 mm) creates a strong grasping effect on the fibrous soft tissue. The cones are hydrophilic, resulting in absorption of water and in a softer feel. They generate more collagen formation, due to the chemical interaction with the tissues, as well as the physical design of the device. A stronger soft tissue support is the result. The cones are absorbed over 8–10 months, with 50% of the device volume being absorbed in approximately five months (Fig. 28.5).
Current status of barbed sutures for cosmetic and wound closure applications
A bi-directionally barbed suture has many barbs serially placed along its length, changing directions somewhere near the suture mid-point, in order to create a mirror image array of barbs in the opposite direction (Figs 28.6, 28.7). Therefore, when engaged in tissue, one end anchors the other end. This suture can be used to close wounds or move tissues differentially along the suture towards the point at which the barbs change direction. The company manufactures both non-absorbable and absorbable sutures, but only the latter (absorbable sutures) are approved for soft tissue approximation for wound closure. This particular suture is made of polydioxanone (PDO). The polymer hydrolyses and its strength degrades in an inverse fashion to the increase in strength of the healing wound.
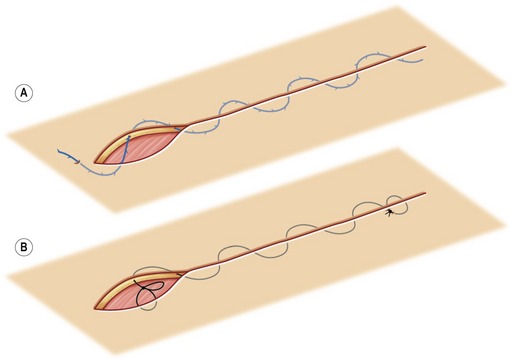
Both barbed and conventional sutures hold best when they engage connective tissue at a right angle to the collagen bundles; however, an ordinary closed loop generally compresses tissue at opposite poles, 180 degrees across from each other. A barbed suture holds better when each barb ensnares collagen fibers. The resulting sinuous passage is preferable to a straight one, as more collagen is encountered. A wavy path will straighten as the suture is tightened, but it will then encounter alternative vectors of force pushing against it. If a suture begins to pull out, new fibers are pressed against the barbs. In contrast, if the barbs in a suture traverse in a straight line, they will encounter a loosened column of tissue as it is pulled out. Undulations also impart elasticity, helping to prevent suture breakage, particularly with ballistic movements of the engaged tissue. Accordingly, curved needles naturally create a stronger closure than straight ones, and they can be used effectively in sinusoidal, helical and mattress patterns (Figs 28.8, 28.9).
Running closures begin near the middle of the wound. As the needle is pulled through the first bite of tissue, the barbs that immediately follow it compress against the shaft of the suture and impart little resistance. As soon as the opposing set of barbs meets the tissue, however, those barbs catch. Then subsequent bites are taken with the first needle until the end of the wound is closed, at which point the needle is simply cut off. The opposite end of the barbed suture closes the wound in a mirror image fashion.
Marking and landmarks
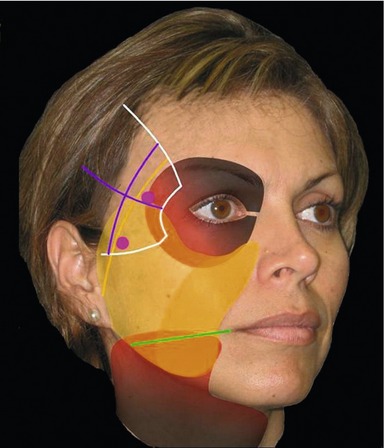
Preoperative marking and preparation (Fig. 28.10): The white line represents the temporal crest, lateral orbital rim, and zygomatic arch. The green line divides the temporal area into its superomedial and inferolateral halves. The purple circles mark the medial zygomatic temporal vein (sentinel vein) and the lateral zygomatic temporal vein. The patient’s skin is marked preoperatively to determine appropriate suture orientation and to prevent injury to the temporal vessels and branches of the facial nerve. The mark for the temporal incisions, about 2 cm behind the hairline, is oriented roughly parallel to the hairline and measures about 3 to 4 cm. This places the incision in the medial half of the temporal area, about 1 cm lateral to the superior temporal crest.
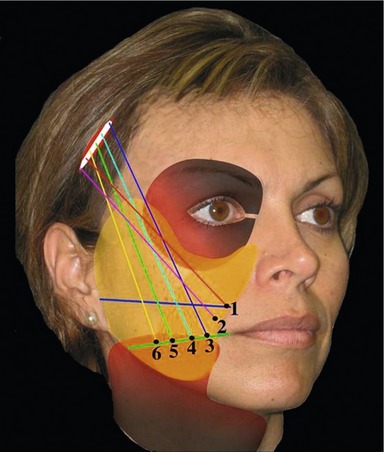
The distal areas of fixation or end points of the suture are marked. These are located at the inferior margin of the malar area. A line is drawn from the midpoint between the ala of the nose and the angle of the mouth to the inferior portion of the tragus. Six points are then marked over this line, starting 5 mm lateral to the nasolabial fold and proceeding at 1 cm intervals until all points are marked (Figs 28.11, 28.12).
Technical steps
Closed midface suture technique
Good candidates for this technique:
• Have mild to moderate midface ptosis.
• Range in age from late thirties to mid-sixties.
• Wish to avoid scars associated with traditional surgical lifts.
• Will accept one week of down time.
• Have realistic expectations; will accept modest lift with shorter period of improvement than with open techniques; will accept need for additional surgery or procedure to maintain improvement and/or correct skin laxity.
• Wish to improve on prior facial surgery.
• Have loose superficial soft tissue glide plane or facial asymmetry; will accept use of Endotine brow and deep midface devices (CoApt, Palo Alto, CA) to provide better fixation and volumetric stacking of soft tissue.
Closed midface surgical procedure
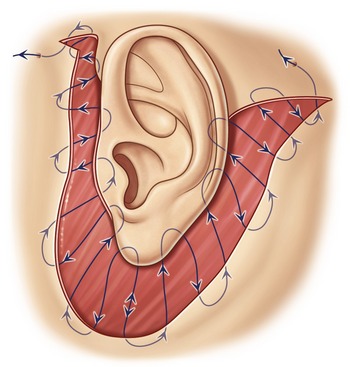
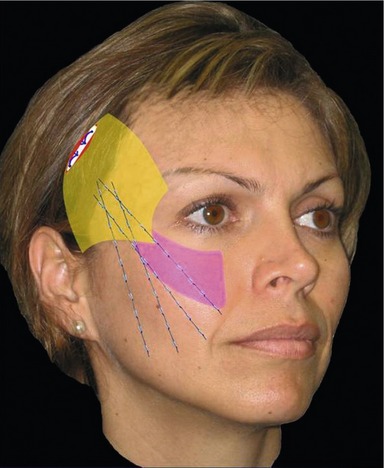
An incision is made in the temporal area approximately 2 to 3 cm behind the anterior hairline, and it is carried down to the deep temporal fascia (DTF) where a plane of blind soft tissue dissection is created between the superficial (STF) and deep temporal fascia (Figs 28.12, 28.13). This facilitates deployment of the 6-inch long straight Silhouette suture needle into the superficial fibrous adipose tissue of the lower temporal area, midface, and lower face. To enhance scar tissue adherence in the midface, insert the needles in pairs, passing the tip just through the exit point in the skin. Leave the needles in place, performing subcutaneous undermining with a small tissue dissector placed through the temporal incision on each side of the needles. Then pull the 6-inch needles completely out of the skin. This will leave intact bridges of tissue where each suture has been placed. The needle exit points are along a line drawn from the buccal commissure medially to the gonion of the mandible laterally. They begin just lateral to the nasolabial fold and are spaced 1 to 1.5 cm apart using a total of four to six sutures per side according to the patient’s needs.
The curved taper needles on the proximal end of the suture are passed through the DTF and then tied in pairs. Tissue repositioning and suspension is accomplished first by tying the knots in the temporal area and then further tissue movement and remodeling are achieved by placing tension on the distal end of the suture and massaging the tissues overlying the sutures from medial to lateral. Distal suture ends can be cut off at the skin at the completion of the procedure or they can be left long to allow for further tissue shaping from one to three days after surgery. One-inch Steri-Strips (3M Healthcare, St. Paul, MN) or one-inch paper tape strips are used for five to seven days to support the facial tissues and minimize bruising and swelling.
Postoperative care
• No talking, except with clenched teeth, for the first 24 hours.
• Low salt and liquid diet for the first 72 hours.
• Cold compresses for three days.
• Clenched mouth talking for three weeks.
• Soft make-up application for three weeks.
• Sleeping on back only, with head elevated above heart.
Complications
Early complications and management
| Complication | Treatment |
|---|---|
| Dimpling | Massage |
| Ecchymosis | Oral and topical arnica montana; oral bromelein |
| Hematoma | Needle aspiration, evacuation, or observation |
| Suture failure | Suture replacement |
| Visible sutures | Suture removal |
| Transmitted pull | Massage |
| Palpable sutures | Nothing, or remove and replace sutures deeper |
| Nerve injury | Observation |
| Skin bunching | Massage |
| Stensen duct rupture (sialocele) | Surgical correction |
Late complications
| Complication | Treatment |
|---|---|
| Dimpling | Massage; needle release |
| Asymmetry | Secondary surgery |
| Scarring | Steroid injection; scar revision |
| Visibility | Suture removal, possible replacement |
| Infection | Antibiotics; possible suture removal |
| Transmitted pull | Massage |
| Patient dissatisfaction |
Pearls & pitfalls
Summary of steps
Closed midface surgical procedure
1. The technique is performed under local anesthesia.
2. An incision is made in the temporal area 2 to 3 cm behind the anterior hairline.
3. The incision is carried down to the DTF where a plane of blind soft tissue dissection is created between STF and DTF, facilitating deployment of the 6-inch long straight Silhouette suture needle into the superficial fibrous adipose tissue.
4. Needles are inserted in pairs, passing the tip just through the exit point in the skin. Subcutaneous undermining is performed with a small tissue dissector placed through the temporal incision on each side of the needles. The 6-inch needles are then pulled completely out of the skin.
5. The curved taper needles on the proximal end of the suture are passed through the DTF and then tied in pairs.
6. Tissue repositioning and suspension is accomplished by tying the knots in the temporal arc and then further tissue movement and remodeling is achieved by placing tension on the distal end of the suture and massaging the tissues overlying the sutures.
7. Distal suture ends can be cut off or they can be left long to allow for further tissue shaping from one to three days after surgery.
8. One-inch Steri-Strips or one-inch paper tape strips are used for 5–7 days to support the facial tissues and minimize bruising and swelling.
Open midface surgical procedure
1. Surgery is performed under general anesthesia requiring  hours.
hours.
2. Mark the patient preoperatively in the sitting upright position.
3. Initial incisions and dissection are the same as for the closed technique.
4. For a modest lift, sutures can be inserted as previously described.
5. For a more dramatic lift, subperiosteal dissection over the middle and medial zygoma and maxilla is completed using illuminated direct vision or the endoscope.
6. Insertion of two to four sutures per side may be done blindly or with illumination. Each needle is inserted in the space created between the STF and DTF down over the zygoma in the subperiosteal space.
7. Sinusoidal advancement with a long straight 6-inch needle is made through the malar pad and soft tissue of the cheek, exiting the skin past the malar pad lateral to the nasolabial fold along the points described in the closed suture procedure.
8. The proximal taper needles are passed through the DTF in the temporal area and tied in pairs. Sutures may be clipped at the skin at the completion of the surgery, or left long for sequential soft tissue molding over one to three days postoperatively.
9. Steri-Strips or one-inch strips of paper tape will support the soft tissue for 5–7 days.
10. This technique simplifies midface suspension with the added benefit of postoperative adjustment.
DeLorenzi CL. Barbed sutures: rationale and technique. Aesthet Surg J. 2006;26:223–229.
Hobar PC, Flood J. Subperiosteal rejuvenation of the midface and periorbital area: a simplified approach. Plast Reconstr Surg. 1999;104:842–851.
Hudson DA, Fernandes DB. Caveats for the use of suspension sutures. Aesthet Plast Surg. 2004;28:170–173.
Isse NG. Elevating the midface with barbed polypropylene sutures. Aesthet Surg J. 2005;26:301–303.
Isse NG. Endoscopic facial rejuvenation. Clin Plast Surg. 1997;24:213–231.
Lee S, Isse N. Barbed polypropylene sutures for midface elevation: early results. Arch Facial Plast Surg. 2005;7:55.
Paul MD. Using barbed sutures in open subperiosteal midface lifting. Aesthet Surg J. 2006;26:725–732.
Ruff G. Technique and uses for absorbable barbed sutures. Aesthet Surg J. 2006;26:620–628.
Sulamanidze MA, Fournier PF, Paikidze TG, Sulamanidze GM. Removal of facial soft tissue ptosis with special threads. Dermatol Surg. 2000;28:367–371.
Sulamanidze MA, Shiffman MA, Paikidze TG, et al. Facial lifting with APTOS threads. Int J Cosmetic Surg Aesthetic Dermatol. 2001;4:275–281.

 circle 26 mm.
circle 26 mm.

 hours. Other complementary procedures can be performed at the same time (Botox, fillers, fat grafting, liposuction, etc.). Mark the patient preoperatively in the sitting upright position, outlining the underlying bony structures, the planned vectors of correction, the path of the temporal branch of the facial nerve and the superficial temporal artery. Initial incisions and dissection are the same as for the closed technique. Blind or illuminated dissection with a periosteal elevator is carried inferiorly, separating the STF from the DTF down to the superior edge of the zygomatic arch, and medially to the lateral orbital rim. For a modest lift, sutures can be inserted as previously described. For a more dramatic lift, subperiosteal dissection over the middle and medial zygoma and maxilla is completed using illuminated direct vision or the endoscope. An optional 1.5 cm incision in the buccal sulcus bilaterally to make subperiosteal dissection of the maxilla and medial zygoma easier to complete with headlight or retractor illumination.
hours. Other complementary procedures can be performed at the same time (Botox, fillers, fat grafting, liposuction, etc.). Mark the patient preoperatively in the sitting upright position, outlining the underlying bony structures, the planned vectors of correction, the path of the temporal branch of the facial nerve and the superficial temporal artery. Initial incisions and dissection are the same as for the closed technique. Blind or illuminated dissection with a periosteal elevator is carried inferiorly, separating the STF from the DTF down to the superior edge of the zygomatic arch, and medially to the lateral orbital rim. For a modest lift, sutures can be inserted as previously described. For a more dramatic lift, subperiosteal dissection over the middle and medial zygoma and maxilla is completed using illuminated direct vision or the endoscope. An optional 1.5 cm incision in the buccal sulcus bilaterally to make subperiosteal dissection of the maxilla and medial zygoma easier to complete with headlight or retractor illumination.







