CHAPTER 23 Surgical problems
Bile
For anatomical causes of obstruction see pages 131–3.
Functional gut obstruction can occur in babies in the following circumstances:
Sometimes bile is seen in aspirates when the feeding tube sits at or has passed through the pylorus — this can be confirmed on an abdominal X-ray. In an otherwise well baby, this can be fixed by pulling the tube back so that its tip lies in the body of the stomach.
Determining cause
Gastrointestinal perforation
The management of infants with gastrointestinal perforation should include:
Necrotising enterocolitis (NEC)
There is a wide spectrum of clinical features in NEC. Signs can include feeding intolerance, vomiting, lethargy, temperature instability, abdominal distension, diarrhoea with or without frank blood, abdominal wall erythema and shock.
The Bell criteria are often used to classify the severity of the illness:
In general terms, large-bowel NEC is a much more benign illness than small-bowel NEC.
Gut obstruction — anatomical causes
Oesophageal atresia
Proximal bowel obstruction
Pyloric stenosis
Pyloric stenosis is uncommon in neonates. It causes non-bile-stained ‘projectile’ vomiting.
Duodenal atresia
Duodenal atresia presents soon after birth with persistent vomiting, which is usually bile-stained.
Malrotation
Baby of mother with polyhydramnios
Delayed passage of meconium
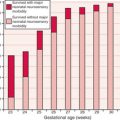
The normal time to passage of meconium increases with decreasing gestational age (GA).
Diagnosis
Always examine the perineum and anus carefully.
Gastroschisis
Therefore, the important aspects of the immediate management of a baby born with gastroschisis are: