CHAPTER 9 Surgical Approaches from an Angiosomal Perspective
The concept of the angiosome was initially described in the cutaneous blood supply,1 but has subsequently been shown to pertain to the underlying viscera and skeleton.2 Devascularization of these deeper structures is less obvious than skin necrosis, but is known to occur, resulting in problems such as nonunion of fractures and avascular necrosis of bones. We seek to organize such information, using the angiosome concept, to present a cogent, comprehensible surgical approach to the three-dimensional vascular anatomy of the forearm and wrist.
Functional Microvascular Anatomy
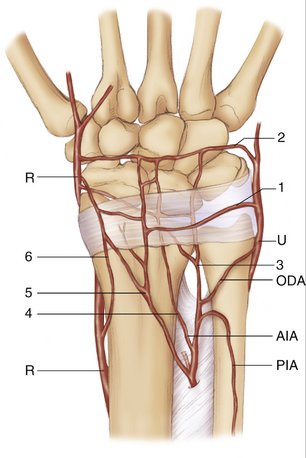
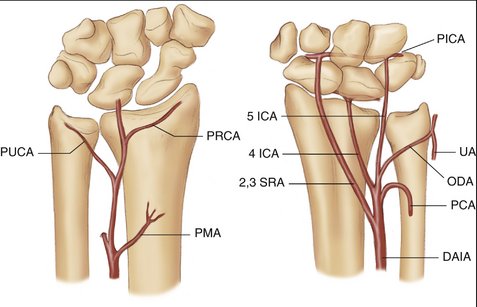
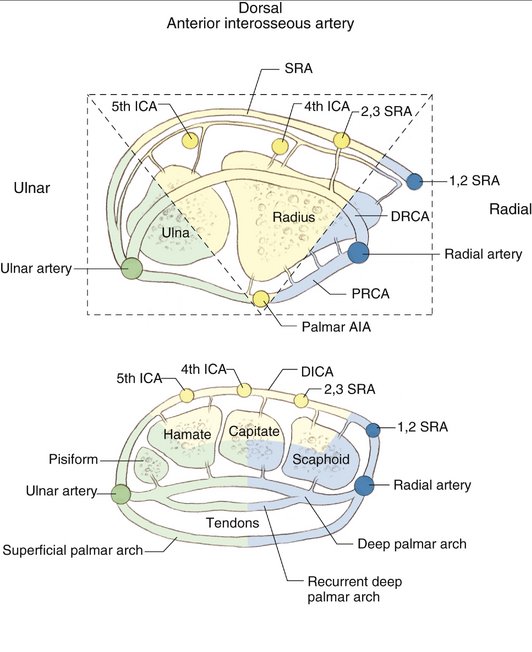
The distal forearm, including the radius, ulna, carpal bones, and overlying soft tissues, is supplied by a network of longitudinal vessels: the radial artery, ulnar artery, anterior interosseous artery (AIA), and posterior interosseous artery (PIA). They are interconnected by dorsal and volar transverse arches (Figs. 9-1 and 9-2). The overlying skin is supplied by direct or septocutaneous perforators arising from these longitudinal vessels (Fig. 9-3), which are small arteries and veins that course along the fibrous septa that separate the muscles in the forearm.
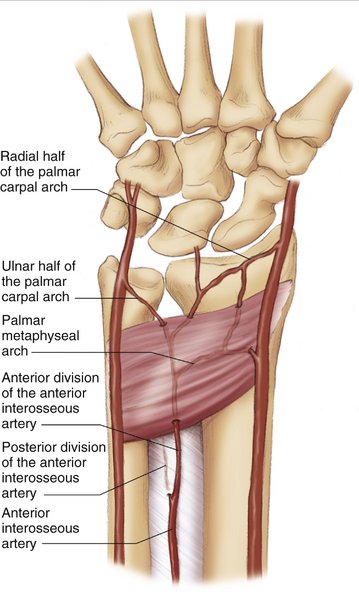
FIGURE 9-1 Palmar Vascularity.
(From Cooney WP, Linscheid RL, Dobyns JH: The Wrist: Diagnosis and Operative Treatment. St Louis: Mosby, 1998, p 108.)
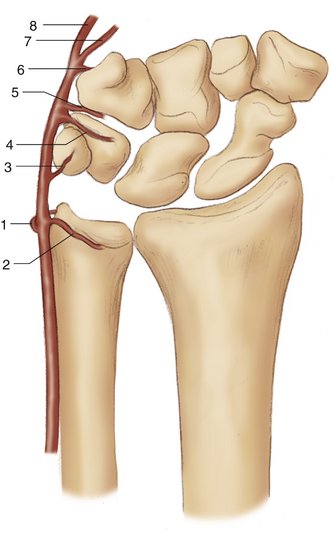
FIGURE 9-3 Perforators of the Forearm, Wrist, and Hand. ADM, abductor digiti minimi; ANC, anconeus muscle; APB, abductor pollicis brevis; APL, abductor pollicis longus; BR, brachioradialis; ECRB, extensor carpi radialis brevis; ECRL, extensor carpi radialis longus; ECU, extensor carpi ulnaris; ED, extensor digitorum; EDM, extensor digiti minimi; EPB, extensor pollicis brevis; EPL, extensor pollicis longus; FCR, flexor carpi radialis; FCU, flexor carpi ulnaris; FDM, flexor digiti minimi; FDS, flexor digitorum sublimus; FPB, flexor pollicis brevis; PL, palmaris longus; PT, pronator teres.
(From Inoue Y, Taylor GI: The angiosomes of the forearm: anatomic study and clinical implications. Plast Reconstr Surg 1996; 98:198.)
An angiosome is a section of tissue that can remain viable based on a single feeding vessel. These angiosomes do not have absolute boundaries, or necrosis from skin incisions would be very common. There is some “built-in” redundancy from the fact that each angiosome connects with the adjacent one via small arteriole branches termed “choke vessels.”1 These vessels respond to ischemic insults within an adjacent angiosome by increasing their diameter to increase blood flow to provide adequate, collateral circulation to the adjacent, compromised angiosome.3 This phenomenon explains the physiology behind the delay procedure commonly used to extend the margins of a flap to be transposed. This process takes 3 days in animal models. In most human clinical applications, the flaps are delayed 1 to 2 weeks before flap transposition. One angiosome may be expanded to include an adjacent angiosome, but it may not cover a more distant angiosome. Adjacent angiosomes tend to interconnect within tissue rather than between intercompartmental fascia separations as might seem intuitive.2 In a traumatic incident or in a surgical dissection if a specific angiosome is rendered ischemic along with its neighboring angiosomes, that angiosome becomes devitalized, predisposing to nonunion or infection.
Radial Artery Angiosome
The radial artery (Fig. 9-4) directly supplies bone (radius, scaphoid, and trapezium), muscle (pronator teres, extensor carpi radialis longus and brevis, brachioradialis, flexor carpi radialis [FCR], flexor digitorum sublimus [FDS], and flexor pollicis longus), and overlying volar radial skin of the forearm, including the mobile extensor wad (see Fig. 9-9).2 The radial forearm flap based on this angiosome has been used as a pedicled septocutaneous flap for coverage of the antecubital fossa; as a pedicled reverse flow septocutaneous flap for hand coverage; and as a free flap to provide skin, muscle, and bone to distant sites.4,5 The radial artery travels between the brachioradialis and FCR, and gives off numerous perforators along the lateral intermuscular septum that either ascend to the overlying skin or dive down to supply the underlying radius and flexor pollicis longus. The versatility of this pedicle and its associated composite flaps is well documented.5–9
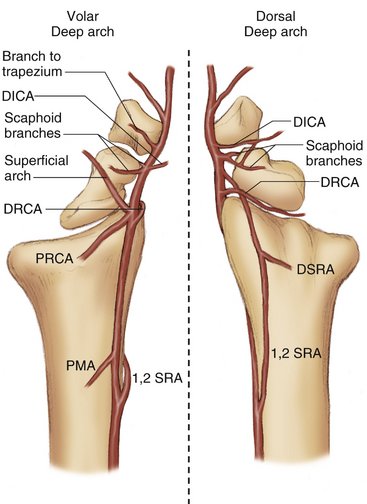
The radial artery not only supplies the voloradial aspect of the distal radius, as might seem intuitively obvious, but also the dorsal aspect of the bone via the 1,2 supraretinacular artery (1,2 SRA), and the dorsal radiocarpal arch (DRCA). The 1,2 intercompartmental artery (ICA) originates from the radial artery approximately 5 cm proximal to the radiocarpal joint. It traverses superficial to the extensor retinaculum over the 1,2 intercompartmental septum sending branches down to the cortical and rarely cancellous bone. Sheetz and colleagues10 described a branch from the 1,2 SRA to the second compartment floor, which penetrates into cancellous bone. This artery connects variably to the radial artery, DRCA, or dorsal intercarpal arch (DICA). The 1,2 SRA also gives off the dorsal supraretinacular arch (DSRA), which connects variably to the 2,3 supraretinacular artery (2,3 SRA), fourth intercarpal artery, fifth intercarpal artery, or ulnar artery. The DRCA, which arises from a direct branch off the radial artery, gives several small feeding vessels to the ridge of the radius at the radiocarpal joint, which descend to the cancellous bone of the metaphysis.10
The radial artery supplies the volar distal radius in a retrograde fashion via the palmar metaphyseal arch (PMA) and palmar radiocarpal arch (PRCA). The PMA originates from the palmar AIA within the pronator quadratus and courses through the muscle to connect with the radial artery giving off scattered perforating branches to the underlying, largely cortical bone. Sheetz and colleagues10 pointed out that the more proximal perforating branches are more likely to penetrate into cancellous bone. This observation was consistent for all of the penetrating vessels of the distal radius in their observations. The PMA pedicle has been used for vascularized bone grafts to the scaphoid. Some authors consider the results of this vascularized bone graft to be inconsistent, which is likely due to the variable penetrating vessels. A larger bone graft rather than a smaller one based on this pedicle is advisable to capture as many perforators as possible. Also, the more proximally the bone graft is harvested to obtain a larger arc of rotation, the more likely it is to have a perforator that penetrates into cancellous bone.
The PRCA is located just proximal to the radiocarpal joint, travels within the palmar wrist capsule, and connects with the palmar AIA and ulnar artery. The PRCA is subdivided into a radial and ulnar component by the palmar AIA forming the T-anastomosis described by Haerle and associates (see Fig. 9-1).11 The radial PRCA gives off multiple branches to the distal radius periosteum supplying cortical and cancellous bone.10
The radial artery supplies the carpus from proximal to distal through (1) branches off the DRCA, (2) branches to the scaphoid tubercle and dorsal ridge, (3) a branch to the DICA, (4) a branch to the trapezium, and (5) branches off the deep palmar arch (Fig. 9-5; see Figs. 9-4 and 9-14). The DRCA arises at the level of the radiocarpal joint and supplies the distal radius, lunate, and triquetrum. It continues to connect to the ulnar artery and possibly the AIA. The branches to the scaphoid arise at the level of the scaphotrapezial joint to enter the distal scaphoid. The volar scaphoid branch frequently connects to the superficial palmar arch (Fig. 9-6), and the dorsal branch connects to the DICA (Fig. 9-7). These arches serve as collateral circulation if the radial artery should become occluded proximally. The DICA originates just distal to the dorsal scaphoid branch and supplies the distal carpal row. Similar to the DRCA, the DICA traverses the wrist to connect with the AIA and ulnar arteries. The branch to the trapezium is the last branch to the carpus before continuing as the dominant vessel to the deep palmar arch. The vascular anatomy of the arches is discussed in further detail later.
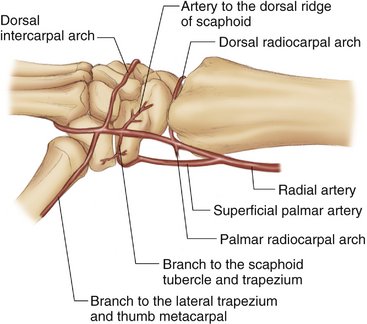
FIGURE 9-5 Schematic of Radial Artery Angiosome.
(From Cooney WP, Linscheid RL, Dobyns JH: The Wrist: Diagnosis and Operative Treatment. St Louis: Mosby, 1998, p 109.)
Anterior Interosseous Artery Angiosome
The AIA (Fig. 9-8) supplies bone (central distal radius and portions of the proximal carpal row), muscles (abductor pollicis longus [APL], extensor pollicis brevis [EPB], extensor pollicis longus [EPL], pronator quadratus, and part of the flexor pollicis longus), and skin and soft tissues of the deep volar and distal dorsal forearm and hand (Fig. 9-9).2 The AIA travels along the anterior surface of the interosseous membrane, then divides into a palmar and dorsal branch just before the pronator quadratus muscle. The palmar AIA gives rise to the PMA and then forms the radial PRCA and ulnar PRCA. As discussed earlier, the PRCA is subdivided into a radial and ulnar component by the palmar AIA. The radial PRCA gives off multiple branches to the distal radius, and the ulnar PRCA, originating just proximal to the radial PRCA, supplies the distal palmar ulnar head. The ulnar PRCA frequently connects to the ulnar artery or the PIA via the oblique dorsal artery to the distal ulna.
FIGURE 9-9 Angiosome of the Forearm.
(From Inoue Y, Taylor GI: The angiosomes of the forearm: anatomic study and clinical implications. Plast Reconstr Surg 1996; 98:207.)
The dorsal branch of the AIA travels through the interosseous membrane into the posterior compartment to supply the dorsal distal radius and contributes to the dorsal arterial arches. Either the common AIA or the proximal dorsal AIA gives off a second dorsal perforating branch, which travels through the interosseous membrane and travels within a septum between the EPB and EPL that segmentally supplies the overlying skin of the distal dorsal radius. These septocutaneous branches have been used as the vascular base of a reverse flap that is able to incorporate skin, dorsal distal radius, and distal posterior interosseous nerve as a composite flap.12,13
The 2,3 SRA arises variably from the common AIA or dorsal branches of the AIA. It courses over the extensor retinaculum and Lister’s tubercle, sending deep perforating branches that usually penetrate into cancellous bone. The 2,3 SRA then connects to the DICA. Other anastomoses between the 1,2 SRA, DRCA, and 4th ICA have been described. Similar to the 1,2 SRA, Sheetz and colleagues10 described a branch from the 2,3 SRA to the second compartment floor.
The 5th ICA arises from the dorsal AIA and connects distally with the DICA. Sheetz and colleagues10 found contributions to the distal radius from the 5th ICA dorsal compartment in only 39% of their specimens. In most cases, the 5th ICA does not directly supply the distal radius or carpus, but serves as a conduit between the radial artery, AIA, and ulnar artery via the DICA.
Posterior Interosseous Artery Angiosome
The PIA supplies bone (ulnar head and neck), muscles (APL, extensor digitorum communis, extensor digiti quinti, extensor carpi ulnaris, EPB, and extensor indicis proprius), and skin of the deep and proximal dorsal forearm (see Fig. 9-9).2 Proximally in the forearm after entering the posterior compartment at the level of the distal edge of the supinator, the PIA continues on top of the APL and beneath the extensor digitorum and extensor carpi ulnaris. It then becomes more superficial in the mid forearm traveling between the extensor carpi ulnaris and extensor digiti quinti. Between the extensor carpi ulnaris and extensor digiti quinti lies a septum from which multiple cutaneous perforators arise supplying the overlying skin of the proximal and mid dorsal forearm. Pedicled flaps for elbow coverage, reverse flow pedicle flaps for distal dorsal hand coverage, and free flaps have been described using this pedicle.14,15
The PIA supplies the distal ulna via the oblique dorsal arteries, which arise from an arch formed by the PIA and the dorsal AIA. The oblique dorsal artery gives off branches that supply the ulnar neck and head and frequently connects to the ulnar artery. The PIA does not have any significant contribution to the radius or carpus (see Fig. 9-2).
Ulnar Artery Angiosome
The ulnar artery (Fig. 9-10) supplies bone (ulna, pisiform, and distal carpal row), muscle (flexor carpi ulnaris, palmaris longus, FCR, FDS, and flexor digitorum profundus), and skin of the ulnar forearm (see Fig. 9-9).2 The ulnar artery travels on the radial side of the flexor carpi ulnaris with the ulnar nerve in the distal two thirds of the forearm. The ulnar artery gives off multiple septocutaneous branches within the medial intermuscular septum to supply the volar/ulnar skin of the entire forearm and wrist. Branches from the ulnar artery to the FDS of the ring and small finger allow for vascularized tendon transfers16 along with overlying fascia and skin. The ascending branch of the dorsal ulnar artery, a branch from the ulnar artery arising 2 to 5 cm proximal to the pisiform, travels superficially and proximally to supply a large area of skin (up to 20 cm long), which may be transferred as a pedicled flap for hand soft tissue coverage.4
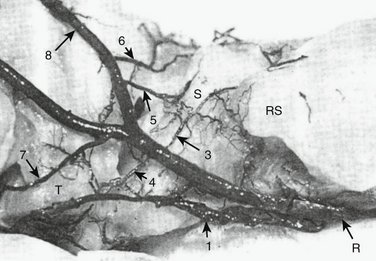
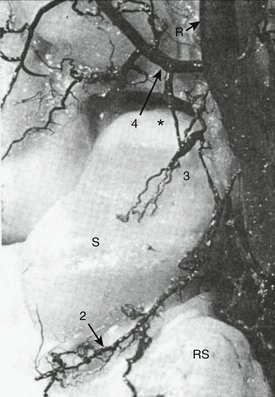
The ulnar artery gives off multiple branches to the distal ulna and carpus largely through the volar and dorsal arches. From proximal to distal, the branches are to the (1) DRCA; (2) PRCA; (3) proximal pisiform and triquetrum; (4) palmar intercarpal arch; (5) distal pisiform and medial hamate, which continues to the DICA; (6) basal metacarpal arch; and (7) superficial and deep palmar arches (Fig. 9-11; see Fig. 9-10). The ulnar artery directly supplies only the ulnar head, pisiform, and medial hamate.
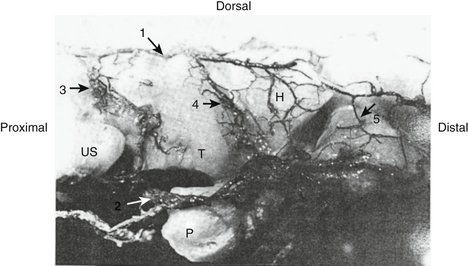
FIGURE 9-11 Injection of Ulnar Artery Angiosome. US, Ulnar styloid; T, triquetrum; P, pisiform; H, hamate; 1, dorsal branch of anterior interosseous artery; 2, medial branch of ulnar artery; 3, dorsal radiocarpal arch; 4, dorsal intercarpal arch; 5, basal metacarpal arch.
(From Gelberman RH, Panagis JS, Taleisnik J, et al: The arterial anatomy of the human carpus, part I: the extraosseous vascularity. J Hand Surg [Am] 1983; 8:372.)
Arches
The arches (Fig. 9-12) serve as bypass routes when one or more of the longitudinal vessels become disrupted and supply the central carpal bones (lunate, triquetrum, trapezoid, capitate).17 There are five volar arches: the PMA, PRCA, palmar intercarpal arch, superficial palmar arch, and deep palmar arch. The PMA and PRCA are interconnected by the radial artery and AIA and supply the radial styloid, volar distal radius, lunate, and triquetrum. Their anatomy was detailed earlier. The palmar intercarpal arch is a diminutive vessel without significant independent contributions arising from the superficial palmar arch and connecting to the ulnar artery at the level of the proximal carpal row. The superficial and deep palmar arches connect the radial to the ulnar arteries. The superficial arch is the continuation of the ulnar artery and supplies the common digital branches, but it does not give any contribution to the carpal vascularity.
The deep palmar arch is the continuation of the radial artery and traverses the wrist just distal to the metacarpal bases. The deep palmar arch gives rise to the radial and ulnar recurrent branches, which combine 45% of the time17 to form a deep recurrent arch. As a group, this deep arch arcade is the dominant supply to the palmar distal carpal row. The radial recurrent artery originates at the level of the index metacarpal and supplies the trapezium and trapezoid.7 The ulnar recurrent branch originates between the bases of the long and ring metacarpals and continues proximally supplying the capitate and hamate, and may connect to the end of the palmar AIA.17 The hook of the hamate is supplied via an accessory ulnar recurrent artery or from direct branches from the ulnar artery.17
There are four dorsal arches: the DSRA, DRCA, DICA, and dorsal metacarpal arch (Fig. 9-13). The supraretinacular arch connects the radial artery, 1,2 ICSRA, 2,3 ICSRA, variably the 4th ICA or 5th ICA, and the ulnar artery. It does not directly supply any underlying bone. The DRCA arises from the radial artery supplying the radius, lunate, and triquetrum, and sometimes connecting to the ulnar artery at the ulnocarpal joint. It also connects to the DICA via interconnecting branches to the lunate and triquetrum. The DICA serves as a conduit between the radial artery, ulnar artery, and dorsal AIA via the 2,3 ICSRA or 5th ICA. The DICA supplies the dorsal distal carpal row. The dorsal metacarpal arch is a series of vascular retes arising from the deep palmar arch and connecting to the DICA, providing a sagittal arch for vascularity of the distal carpal row.
Surgical Approaches (Box 9-1)
Dorsal Approaches
The dorsal distal radius can be approached radially between the first and second compartments, centrally between the third and fourth compartments, or ulnarly between the fifth and sixth compartments. There is little need to cross the dorsal wrist crease at acute angles because extension contractures are uncommon, secondary to the stronger pull of the flexors and the mobility of the dorsal skin. The tips of triangular flaps can be prone to ischemia and wound healing complications.18,19 When opening the extensor retinaculum, it should be incised at an oblique angle creating two peripherally based flaps that may be allowed to slide across one another making for easier closure. The decision to place a flap of retinaculum beneath the extensor tendons in cases of rheumatoid arthritis or hardware placement also should be made on opening instead of closing.
BOX 9-1 Vessels at Risk
| Dorsal radial approach | Branches to the scaphoid |
| Distal 1,2 SRA | |
| 2,3 SRA | |
| DICA | |
| DSRA | |
| Dorsal central approach | DSRA |
| DRCA | |
| 2,3 SRA | |
| DICA | |
| Dorsal ulnar approach | DSRA |
| DRCA | |
| DICA | |
| 5th ICA | |
| Palmar “FCR” approach | PMA |
| PRCA | |
| Palmar AIA | |
| Superficial palmar arch | |
| Palmar midline approach | PRCA |
| Palmar AIA |
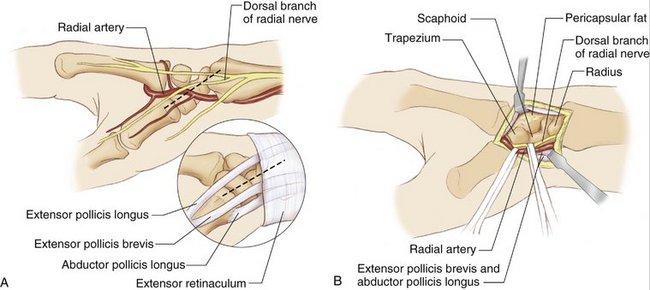
The dorsal radial approach uses a skin incision over the anatomical snuffbox extending proximally or distally depending on the underlying structures to be examined (see Fig. 9-13). Care is taken to identify and retract the radial sensory nerve, which lies just beneath the superficial vein. Perforators to the skin arise more proximally from the lateral intermuscular septum via the radial artery and from the dorsal AIA from the septum between the EPB and EPL (see Fig. 9-3). This is a common approach to the scaphoid. At the level of the scaphotrapezial joint, the volar and dorsal branches to the scaphoid, the reinsertion of the 1,2 SRA, and the origin of the DICA from the radial artery are at risk for injury (see Figs. 9-5 and 9-6). If possible, the branches to the scaphoid should be preserved by identifying and incising the capsule over the scaphocapitate joint. The dissection can be extended laterally to expose the scaphoid, protecting the dorsal ridge vessels if exposure of the entire dorsal surface of the scaphoid is required. If connections between the superficial palmar arch and the volar scaphoid branch or between the DICA and the dorsal scaphoid branch exist, it may be possible to mobilize the radial artery further without injury to the scaphoid vascular supply (see Figs. 9-6 and 9-7).
The central or standard dorsal approach to the wrist uses a linear skin incision starting at the base of the second metacarpal and extending proximally and obliquely crossing just ulnar to Lister’s tubercle.20 Alternatively, one may begin at the base of the third metacarpal and extend proximally (Fig. 9-14). By necessity, the supraretinacular arch is divided. The extensor retinaculum is divided obliquely just ulnar to Lister’s tubercle, and the EPL is released from its compartment. The subperiosteal plane is entered at the base of the third compartment, and the remaining compartments are elevated off the radius, being mindful to attempt to leave the perforators from the 1,2 ICSRA at the base of the second compartment along with the origin of the dorsal radiocarpal ligament radially, and the dorsal radioulnar ligament and dorsal AIA branches ulnarly.
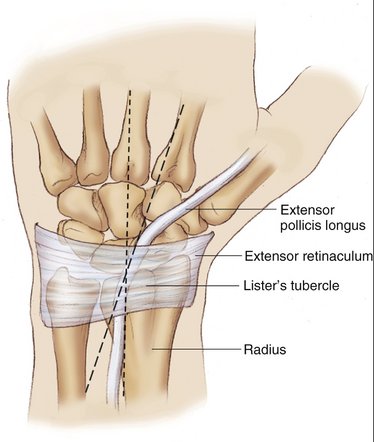
FIGURE 9-14 Dorsal Approach.
(From Cooney WP, Linscheid RL, Dobyns JH: The Wrist: Diagnosis and Operative Treatment. St Louis: Mosby, 1998, p 127.)
If the dorsal radiocarpal joint capsule is opened, and the DRCA is divided, collateral flow is sustained by the DICA. The joint capsule can be opened many ways, including a linear, triangular flap sparing the dorsal radiocarpal and dorsal intercarpal ligaments or extending this triangular flap with a back cut along the radiocarpal joint (Fig. 9-15).
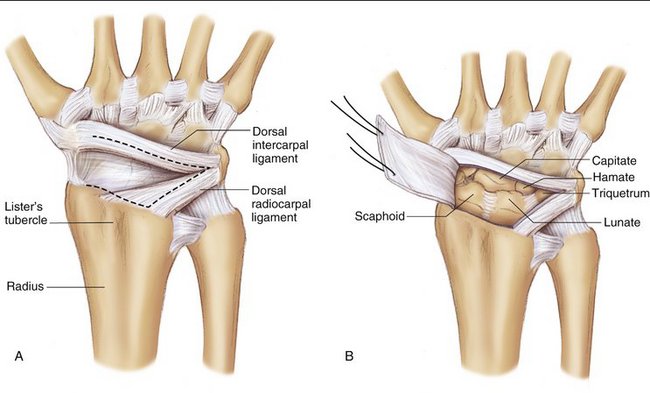
FIGURE 9-15 Capsular Incision.
(From Cooney WP, Linscheid RL, Dobyns JH: The Wrist: Diagnosis and Operative Treatment. St Louis: Mosby, 1998, p 130.)
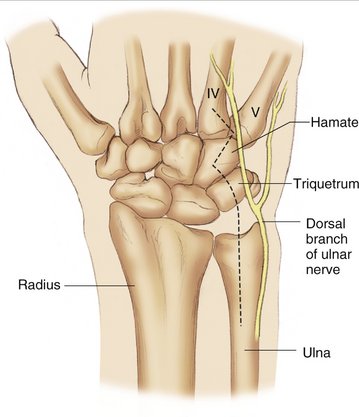
The ulnar dorsal approach uses a variable skin incision from the triquetral tuberosity and extending proximally down the shaft of the ulna (Fig. 9-16). Care is taken not to injure the ulnar sensory nerve traveling dorsally 1 to 2 cm distal to the ulnar head. The DSRA is cauterized, and the extensor retinaculum is entered between the fifth and sixth compartments. Bowers21 uses a radially based flap of extensor retinaculum, taking care not to enter the fourth compartment and the 4th ICA. The 5th ICA is likely to need to be cauterized, but, as mentioned previously, the 5th ICA rarely nourishes the underlying radius serving as a conduit between the dorsal AIA and the DICA. At this point, the radioulnar joint capsule or the dorsal ulnar wrist capsule may be opened, exposing the distal radioulnar joint or ulnocarpal joint. The DRCA is divided in exposing the distal radioulnar joint, but the dorsal vascularity to the triangular fibrocartilage complex is kept largely intact if the 4th ICA is not entered. As the dissection is extended proximally, the oblique dorsal artery from the ulnar artery is likely to be divided, but this is of little significance to the distal vascularity.
Palmar Approaches
As the dissection is performed near the radiocarpal joint, especially on the medial column of the radius, the volar RCA is likely to be encountered if the dissection plane is above the periosteum as the radial volar RCA arises from the palmar AIA coursing obliquely and distally toward the radial artery. The superficial arch as it arises from the radial artery also may need to be divided if the incision is carried distal in an oblique fashion toward the scaphoid tubercle across the volar wrist crease, as in Russe’s approach22 to the scaphoid. If the radiocarpal joint needs to be exposed, the floor of the FCR sheath is opened, the FCR is retracted, and the volar RCA is visualized and controlled. Caution should be exercised not to injure the volar RCA at its origin at the volar AIA and at the radial artery, or there would be a segment of devascularized distal volar radius. To expose the scaphoid fully, the radioscaphocapitate and long radiolunate ligaments need to be incised, but care should be taken to note their location because repair is mandatory. This approach provides access to the entire volar radius, volar scaphoid, and scapholunate ligament.
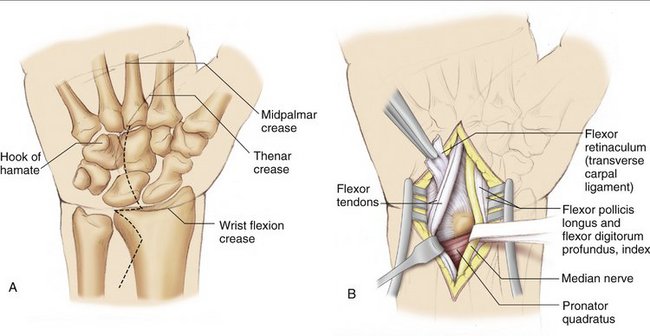
The midline approach skin incision may begin in the palm as for a carpal tunnel release, or at the wrist crease just ulnar to the palmaris tendon to avoid damage to the palmar cutaneous nerve (Fig. 9-17). It remains on the ulnar side of the forearm until the mid forearm, at which point it may be directed radially if needed; this is to ensure adequate coverage of the median nerve in the distal forearm where it is not protected by the muscle bellies of the FDS tendons. The median nerve is identified, and the flexor retinaculum is divided from proximal to distal just radial to the hook of the hamate. The median nerve and flexor tendons are retracted, and the pronator quadratus is exposed. The pronator may be taken down from the radius and elevated ulnarly in the subperiosteal plane. Generally, this approach is used for a volar fasciotomy and complex carpal dislocations, and it likely would be combined with a carpal tunnel release. This approach tends to spare the vasculature, but is not easily extendable to reach the radial border.
Combined Approaches
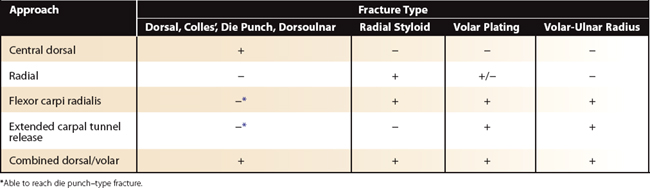
An exhaustive description of all possible approaches would be enervating to read; we focus on the principles that should guide surgical judgment. Most clinical scenarios can be planned using Figure 9-3 and Table 9-1, which show where the skin perforators arise, and what structures can be exposed using the described approaches.
With regard to the skin incision, one should not make two parallel incisions between skin perforators because the skin between the incisions would be ischemic. Referencing Figure 9-3 showing where the perforators arise in the distal forearm, we observe that we could make two incisions on either side of the radial artery/lateral intermuscular septum (FCR and dorsal radial approaches) because there is collateral flow on the volar side from the ulnar artery and on the dorsum from the AIA. Alternately, if the FCR and volar midline approaches are used, there are no perforators arising to the skin between the incisions resulting in ischemia. Undermining between incision lines above the plane of the vessels also should be limited or avoided because this would transect perforating vessels to the overlying skin bridge.
Panagis and coworkers23 classified carpal bone vascularity into three groups based on number and location of perforating branches, presence of intraosseous vascular anastomosis, and existence of a large portion of the bone supplied by a single perforator. Group 1 included bones with perforators only on one surface, or a large portion of bone supplied by a single perforator. Group 1 included the scaphoid, in which the dorsal vessel enters at the dorsal ridge and travels proximally to supply the proximal bone without intraosseous connection to the palmar perforator; the capitate, in which in 50% of their series the head was supplied only via a palmar perforator; and some lunates, 20% of their series, which had only a single palmar perforator. Group 2 had at least two perforators at different sites, but lacked intraosseous anastomosis. This group included the trapezoid, which has dorsal and volar perforators, but no anastomosis, and the hamate, which has a volar perforator for the hook and a dorsal perforator for the body without anastomosis. Group 3 had at least two perforators with intraosseous anastomosis and included the trapezium, triquetrum, pisiform, and most lunates.
Discussion and Conclusion
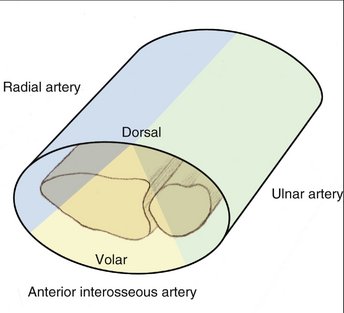
It is important to be able to visualize the angiosomes of the distal forearm and wrist as a three-dimensional structure. The radial artery supplies the skin of the radial side of the forearm, and the ulnar artery supplies the ulnar side of the forearm. There is a dorsal strip of skin that is supplied distally by the dorsal branch of the AIA and proximally by the PIA. When these skin boundaries are segmented three-dimensionally, they form an elongated pyramid with the base of the pyramid on the dorsal skin and the tip at the volar skin flanked on either side by a semicircular tube (Fig. 9-18). The intersecting lines roughly divide the bone into angiosome segments.
1. Taylor GI, Palmar JH. The vascular territories (angiosomes) of the body: experimental study and clinical applications. Br J Plast Surg. 1987;40:113141.
2. Inoue Y, Taylor GI. The angiosomes of the forearm: anatomic study and clinical implications. Plast Reconstr Surg. 1996;98:195-210.
3. Dhar SC, Taylor GI. The delay phenomenon: the story unfolds. Plast Reconstr Surg. 1999;104:2079-2091.
4. Martin D, Bakhach J, Casoli V, et al. Reconstruction of the hand with forearm island flaps. Clin Plast Surg. 1997;24:33-48.
5. Rohrich RJ, Ingram AEJr. Brachioradialis muscle flap: clinical anatomy and use in soft-tissue reconstruction of the elbow. Ann Plast Surg. 1995;35:70.
6. Braun FM, Haong PH, Merle M, et al. Technique and indications of the forearm flap in hand surgery: a report of thrity-three cases. Ann Chir Main. 1985;4:85-97.
7. Govila A, Sharma D. The radial forearm flap for reconstruction of the upper extremity. Plast Reconstr Surg. 1990;86:920-927.
8. Soucacos PN, Beris AE, Xenakis TA, et al. Forearm flap in orthopaedic and hand surgery. Microsurgery. 1992;13:170-174.
9. Muhlbauer W, Herndl E, Stock W. The forearm flap. Plast Reconstr Surg. 1982;70:336-342.
10. Sheetz KK, Bishop AT, Berger RA. The arterial blood supply of the distal radius and ulna and its potential use in vascularized pedicled bone grafts. J Hand Surg [Am]. 1995;20:902-914.
11. Haerle M, Schaller HE, Mathoulin C. Vascular anatomy of the palmar surfaces of the distal radius and ulna: its relevance to pedicled bone grafts at the distal palmar forearm. J Hand Surg [Br]. 2003;28:131-136.
12. Shibata M, Ogishyo N. Free flaps based on the anterior interosseous artery. Plast Reconstr Surg. 1996;97:746-755.
13. Hu W, Martin D, Baudet J. Thumb reconstruction by the anterior interosseous osteocutaneous retrograde island flap. Eur J Plast Surg. 1994;17:10.
14. Chen HC, Tang YB, Chuang D, et al. Microvascular free posterior interosseous flap and a comparison with the pedicled posterior interosseous flap. Ann Plast Surg. 1996;36:542-550.
15. Zancolli EA, Angrigiani C. Posterior interosseous island forearm flap. J Hand Surg [Br]. 1988;13:130-135.
16. Cavadas PC, Mir X. Single-stage reconstruction of the flexor mechanism of the fingers with a free vascularized tendon flap: case report. J Reconstr Microsurg. 2006;22:37-40.
17. Gelberman RH, Panagis JS, Taleisnik J, et al. The arterial anatomy of the human carpus, part I: the extraosseous vascularity. J Hand Surg [Am]. 1983;8:367-375.
18. Millender LH, Nalebuff EA. Arthrodesis of the rheumatoid wrist: an evaluation of sixty patients and a description of a different surgical technique. J Bone Joint Surg Am. 1973;55:1026-1034.
19. Potts H, Noble J. Surgical approaches to the dorsum of the wrist: brief report. J Bone Joint Surg Br. 1988;70:328-329.
20. Weil C, Ruby LK. The dorsal approach of the wrist revisited. J Hand Surg [Am]. 1986;11:911-912.
21. Bowers WH. The distal radioulnar joint. In Green DP, editor: Operative Hand Surgery, 2nd ed, New York: Churchill Livingstone, 1988.
22. Russe O. Fracture of the carpal navicular: diagnosis, non-operative treatment, and operative treatment. J Bone Joint Surg Am. 1960;42:759-768.
23. Panagis JS, Gelberman RH, Taleisnik J, et al. The arterial anatomy of the human carpus, part II: the intraosseous vascularity. J Hand Surg [Am]. 1983;8:375-382.