Chapter 2 Surgical Anatomy of the Elbow
Osteoarticular anatomy
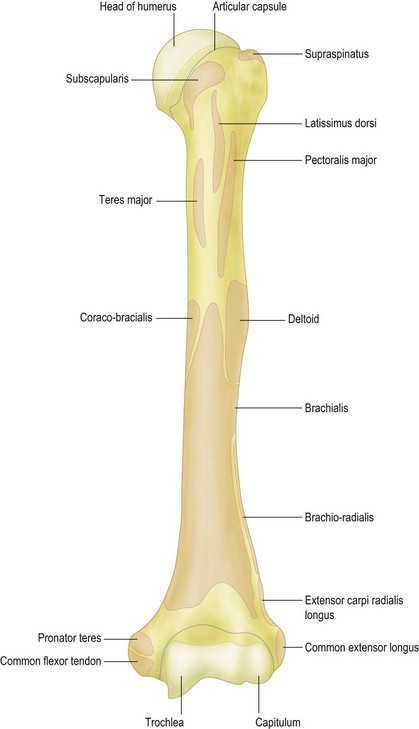
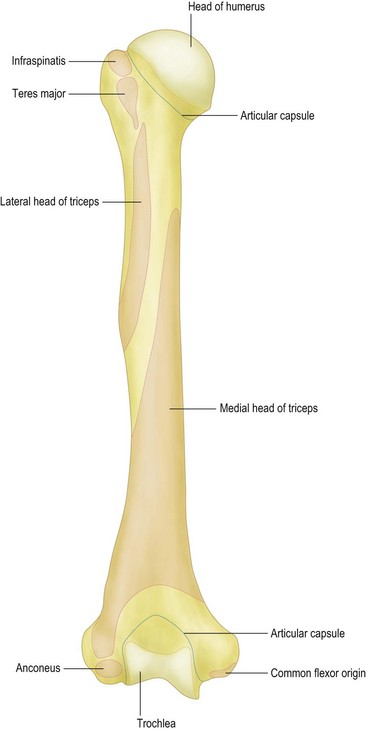
Humerus
The shaft of the humerus ends distally in both lateral and medial ridges. Thereafter lateral and medial epicondyles are formed (Figs 2.1 and 2.2). They can be inspected and palpated during clinical examination, the medial part being better defined than its lateral counterpart. The flexion crease of the skin on the anterior aspect of the elbow is at the same level as a line joining the two epicondyles, 1 cm proximal to the elbow joint. The presence of an accessory origin of the pronator teres muscle, approximately 5 cm superior to the medial epicondyle on the anterolateral side of the humeral shaft, can be found in 1–3% of individuals. In these cases, the ligament of Struthers attaches to a bony prominence and can sometimes cause compression of the median nerve that travels beneath the ligament along with the brachial artery.
Redrawn with permission of http://www.graysanatomyonline.com, Elsevier Ltd. Chapter II. Osteology. 6a.3 Fig. 207.
Redrawn with permission of http://www.graysanatomyonline.com, Elsevier Ltd. Chapter II. Osteology. 6a.3 Fig. 208.
Two indentations on the anterior side of the humerus prevent impingement of the coronoid process and the radial head during flexion: the coronoid fossa is located medial to the smaller radial fossa. The olecranon fossa is located on the posterior side to allow space for the olecranon during extension of the elbow (Fig. 2.2).
The lateral epicondyle forms the capitellum. This is hemispheric in shape and articulates with the concave head of the radius. It is separated from the trochlea by a groove, which articulates with the rim of the radial head throughout flexion/extension and pronation/supination. The trochlear–capitellar articular axis is oriented approximately 5–7° internally rotated in relation to the humeral epicondyles; in addition, this axis has an approximately 6–8° valgus tilt in relation to the humeral axis.1 The capitellum is oriented anteriorly and cannot therefore be observed when the elbow is visualized posteriorly. When fixing transverse distal humeral fractures it allows the application of a plate more distally on the posterior side of the lateral column. The distal part of the humerus is angulated 30° anteriorly, such that the centres of the two condyles are collinear with the anterior humeral cortex on a lateral radiograph.
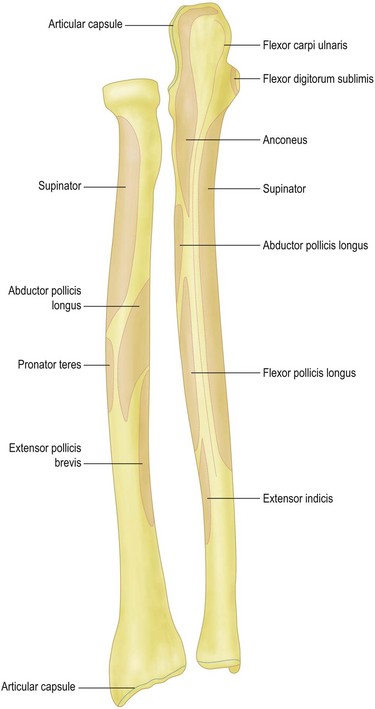
Ulna
The olecranon is the subcutaneous portion of the ulna and therefore the most prominent bony surface landmark of the elbow (Figs 2.3–2.5). It forms the trochlear notch (incisura semilunaris) on its anterior side with the coronoid process, a protuberance that demarcates the articular surface anteriorly. This coronoid process can fracture during dislocation of the elbow. The trochlear notch forms an arc of approximately 190°. While most of this articular surface is covered with cartilage, there is an area in the centre where either the cartilage is thin or absent. This is a normal finding and should not be interpreted as osteochondral damage. It is, however, a safe area through which an olecranon osteotomy can be performed. The shape of this notch is elliptical, with a longitudinal ridge articulating with a deeper portion of the trochlea. This affords bony stability.
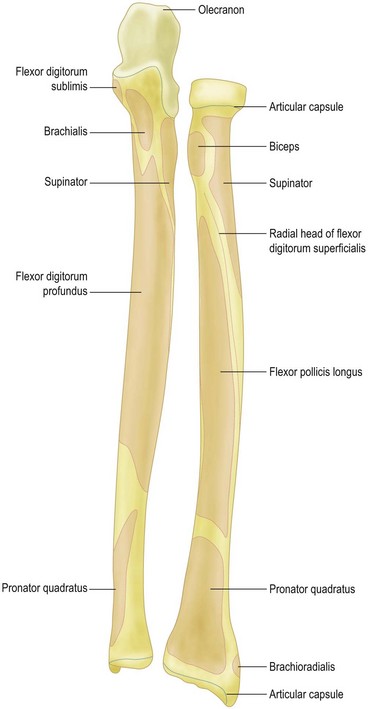
Redrawn with permission of http://www.graysanatomyonline.com, Elsevier Ltd. Chapter II. Osteology. 6a.4 Fig. 213.
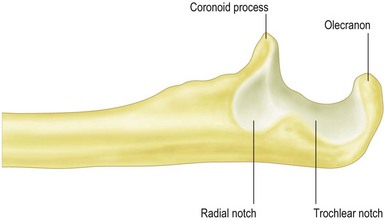
Figure 2.4 Left ulna, lateral view.
Redrawn with permission of http://www.graysanatomyonline.com, Elsevier Ltd. Chapter II. Osteology. 6a.4 Fig. 212.
Redrawn with permission of http://www.graysanatomyonline.com, Elsevier Ltd. Chapter II. Osteology. 6a.4 Fig. 214.
The long axis of the ulna and the humerus determines the overall carrying angle of the elbow. Studies report a valgus angle ranging from 11° to 14° in men and from 13° to 16° in women.2
Radius
The radial head is shaped like a concave disc and is attached to the radial shaft by the radial neck (Figs 2.3 and 2.5). The proximal end articulates with the capitellum and the circumferential surface articulates with the lesser sigmoid notch. Therefore not only is the proximal end covered with articular cartilage but also a 280° arc about the circumference. The 80° arc that remains uncovered can be used to place screws in case of displaced radial head fractures. The angle between radial head and shaft is 13°. The radial head is not a perfect circle and is variably offset from the axis of the neck. This has important implications for reconstruction of the radial head.3,4 On the anteromedial side just distal of the radial neck lies the bicipital (also called radial) tuberosity: a bony tuberance into which is inserted the biceps tendon.5,6
Articulations
The elbow is one of the most congruent joints in the body. As mentioned before, there are three articulations in the elbow: ulnohumeral, radiohumeral (or radiocapitellar) and proximal radio-ulnar joint. The elbow has been called the trochleogingylomoid joint: the ulnohumeral is a hinge (ginglymus) joint that allows flexion and extension and the radiohumeral (or radiocapitellar) and proximal radio-ulnar joint are trochoid joints, allowing axial rotation or pivoting.1 The radial head and the ulna articulate during pronation and supination of the forearm at the proximal radio-ulnar joint.
Clinical Pearl 2.1
Capsuloligamentous anatomy
Joint capsule
The three elbow joints are surrounded by a joint capsule. The capsule attaches along the articular margin of the elbow. It includes the olecranon, the coronoid and radial fossae, but not the humeral epicondyles. On the anterior side of the elbow, it originates above the coronoid and radial fossae and inserts distally onto the anterior border of the coronoid and the annular ligament on the lateral side (Figs 2.1, 2.2, 2.3 and 2.5). Distal to the radial annular ligament, the joint capsule forms a recess to allow rotation of the radius. The posterior part attaches above the olecranon fossa proximally and distally along the medial and lateral articular margins of the greater sigmoid notch. Medial and lateral collateral ligaments reinforce the capsule.
Fat pads
Fat pads lie within the joint capsule in the coronoid, radial and olecranon fossae. These can become displaced from their respective fossae by intra-articular fluid accumulation. This displacement of the intra-articular fat pads results in positive radiographic fat pad signs.7
Medial collateral and the lateral collateral ligament complexes
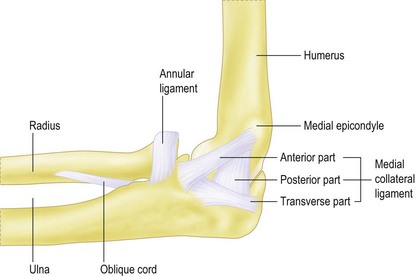
The medial collateral ligament consists of an anterior and a posterior bundle. In between lies a transverse ligament (Fig. 2.6). The anterior bundle is the primary restraint to valgus stress. It originates on the central two-thirds of the antero-inferior aspect of the medial humeral epicondyle. The anterior bundle inserts at the base of the coronoid on average 18 mm posterior from the tip. The width of its origin averages about 10 mm and involves 67% of the epicondyle In the coronal plane.8,9 Knowledge of the insertion sites is clinically important: for example, when medial epicondylectomy is being performed, only 20% of the epicondyle can be removed without violating the origin of the anterior medial collateral ligament. Also, its deep origin allows elevation of the flexor tendons off the medial epicondyle without detaching the ligament. The posterior location of the insertion site prevents damage to the ligament from fractures of the tip of the coronoid, although it does become detached with fractures at the base of the coronoid. The mean length of the anterior bundle is about 27 mm, with a width of 4–5 mm. Some studies have also shown that the anterior medial collateral ligament can be subdivided into anterior and posterior bands. These bands demonstrate a different tension in various positions of the elbow, due to a ‘cam effect’.10 Finally, some authors claim a third central portion which remains isometric throughout elbow movement. The latter can be used as a guide for ligament reconstruction.11 This deep bundle runs from 5 mm anterior to the distal tip of the medial epicondyle to the most prominent part of the sublime tubercle on the ulna. The posterior bundle of the medial collateral ligament inserts slightly posterior to the anterior medial collateral ligament and fans out along the base of the greater sigmoid notch. It has an average width of 8 mm and a thickness of 4–8 mm. The function of this ligament is to restrain valgus stress, especially during flexion.1,10,12
Microscopic evaluation has revealed distinct collagen bundles within the capsular layers. The anterior bundle has an additional ligament complex superficial to the capsular layer confluent with the flexor muscle mass.13
Four distinct bundles comprise the lateral collateral ligament complex: the lateral ulnar collateral ligament, the radial collateral ligament, the annular ligament and the accessory lateral collateral ligament (Fig. 2.7). It is a key stabilizer for varus stress and posterolateral stability.
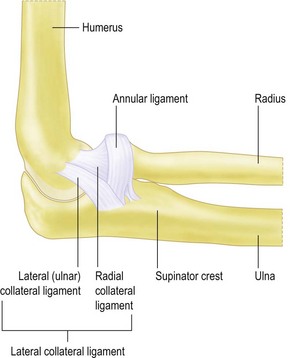
Figure 2.7 Lateral collateral ligament complex.
Reprinted with permission of Lockard L, J Hand Ther.20
The ulnar insertion of this ligament complex varies, being described as either a broad insertion blending the lateral and annular ligaments, or as being bilobed with more distinct insertions.14
Additional structures
The interosseous membrane between the ulna and the radius prevents divergence of the radius or ulna and regulates the forces acting on these two bones.10 Together with the distal radio-ulnar joint it is a key component in forearm rotation and stability.
Clinical Pearl 2.2
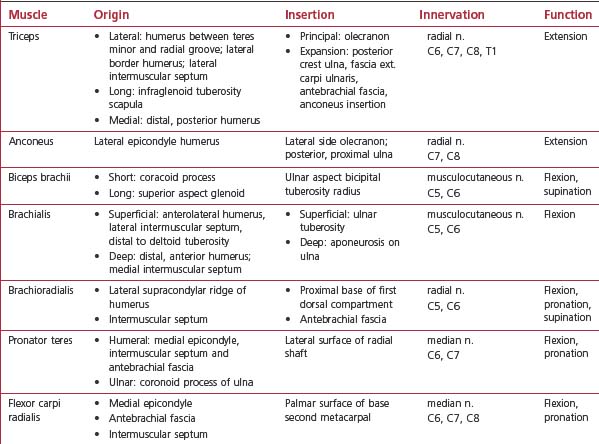
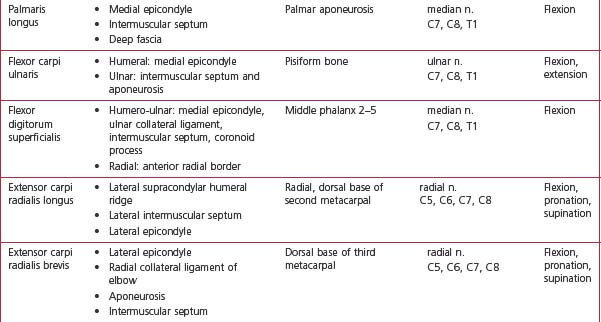
Muscular anatomy
The extensor apparatus contains both the triceps and anconeus muscles. Proximally, the triceps possesses three origins: the lateral, long and medial heads. The three heads meet and end as one tendon distally (Fig. 2.8). The lateral head has three origins, including the humerus between the teres minor insertion and the proximal part of the radial groove, the lateral border of the humerus, and the lateral intermuscular septum. The long head originates from the infraglenoid tuberosity of the scapula. The medial head originates from the posterior humerus distal to the spiral groove. Distally the extensor mechanism of the triceps consists of two components: the principal part and the expansion part. The principal part is the larger tendon, which inserts onto the olecranon. This insertion consists of both tendon and muscle. The expansion inserts onto four different sites: the posterior crest of the ulna medially, the fascia of the extensor carpi ulnaris origin laterally, the antebrachial fascia distally, and the anconeus insertion deeply. The principal part seems to be able to compensate for the expansion part in case of injury. However, the reverse does not appear possible.
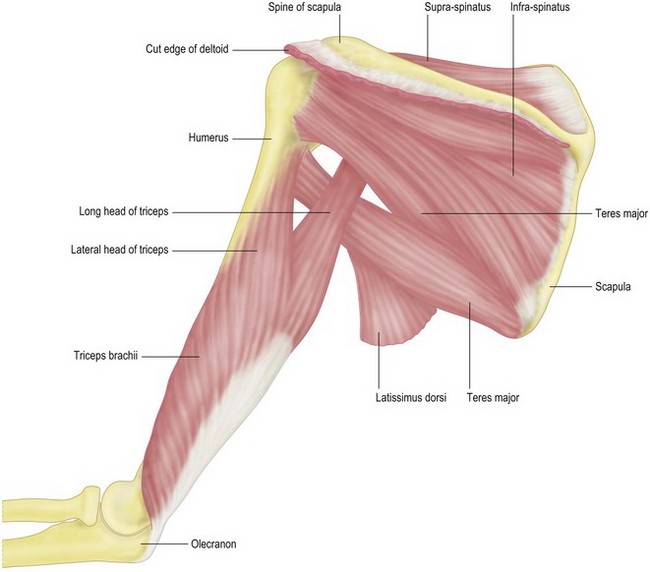
Figure 2.8 Posterolateral view of the musculus triceps brachii.
Redrawn with permission of http://www.graysanatomyonline.com, Elsevier Ltd. Chapter IV. Myology. 7c Fig. 412.
Madsen et al discovered that the tendon of the triceps consists of two components: a superficial part which originates from the lateral and long head of the triceps, and a deep part which originates from the medial head. Both merge prior to insertion.15 The deep tendon seems to be responsible for most of the strength generated when the arm is extended between maximum flexion and 90°, whereas both generate the maximum amount of force near terminal extension.
The anconeus muscle is a small triangular muscle that arises from the lateral epicondyle of the humerus and inserts onto the lateral side of the olecranon as well as the posterior surface of the proximal ulna (Fig. 2.9). The exact function of the anconeus muscle is still a point of discussion: some believe it functions as an abductor of the ulna in pronation,16 while others claim that it has a joint-stabilizing effect. The anconeus muscle receives its blood supply from the recurrent posterior interosseous artery, the medial collateral artery and the posterior branch of the radial collateral artery. This muscle is often used as a transposition flap to cover defects around the elbow, the size of the defect ranging from 6 to 25.5 cm2.17
Redrawn with permission of http://www.graysanatomyonline.com, Elsevier Ltd. Chapter IV. Myology. 7e Fig. 418.
The flexor apparatus contains the biceps brachii, the brachialis and the brachioradialis muscles.
The biceps brachii consists of two parts: the short and long heads (Fig. 2.10). The short head originates from the coracoid process and the long head from the superior aspect of the glenoid. Initially both heads were thought to fuse into a single tendon and insert onto the ulnar aspect of the bicipital tuberosity of the radius. However, further recent research indicates that the distal biceps tendon can be divided into an anterior layer (linked to the short head) and a posterior layer (linked to the long head). An important landmark is the bicipital aponeurosis, which arises from the distal short head of the biceps tendon. Some cadaver studies, however, show that the two heads are not always separated at the distal tendon, and that it would be more accurate to describe the biceps as two fully independent muscles and tendons with a variety of connections between the two structures. Finally, the biceps rotates 90° externally from origin to insertion. This rotation is of relevance to the surgeon during the surgical repair of a ruptured biceps tendon.
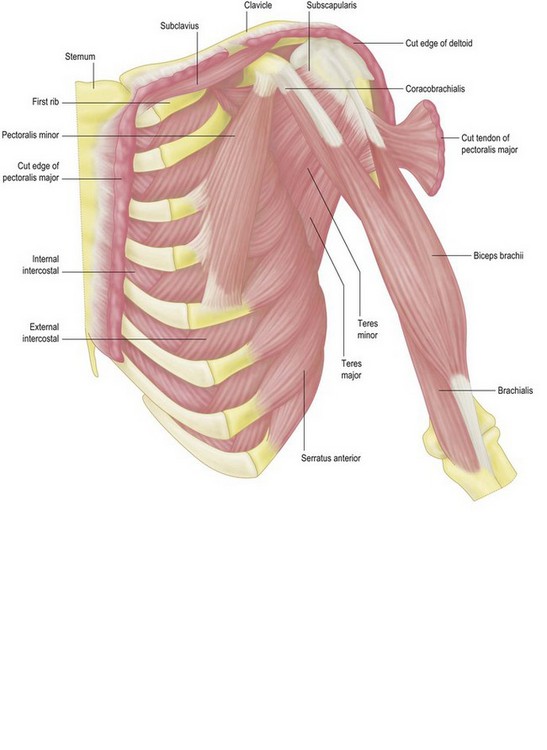
Figure 2.10 Anterior view of the musculus biceps brachii and the musculus brachialis.
Redrawn with permission of http://www.graysanatomyonline.com, Elsevier Ltd. Chapter IV. Myology. 7 Fig. 411.
The brachialis muscle is also divided into two heads: a superficial head and a deep head (Fig. 2.10). The superficial head, which is larger than the deep head, originates from the anterolateral aspect of the middle third of the humerus and the lateral intermuscular septum, distal to the deltoid tuberosity. The superficial head inserts as a circular tendon on the ulnar tuberosity. The deep head originates from the distal third of the anterior aspect of the humerus and the medial intermuscular septum. The deep muscle head ends as a sagittally oriented aponeurosis that inserts on the ulna. This aponeurosis covers the space between the ulnar tuberosity and the coronoid process.
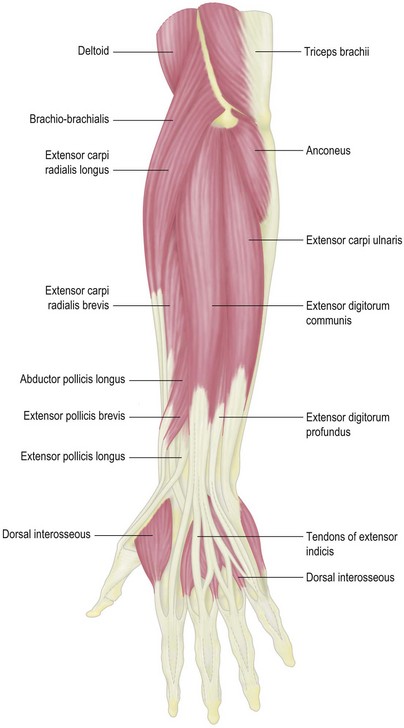
The brachioradialis muscle originates from the proximal part of the lateral supracondylar ridge of the humerus and the adjacent intermuscular septum (Fig. 2.9). Distally, the conversion from muscle to tendon is situated between the proximal and middle thirds of the forearm. The brachioradialis muscle inserts at the base of the first dorsal compartment, beginning 17 mm from the radial styloid tip and extending 15 mm proximally. This compartment is surrounded by bony protuberances from which the fascial septa on the radial aspect of the distal part of the radius arise, resulting in a tunnel-like structure. The whole length of the tendon attaches firmly to the underlying antebrachial fascia, thus limiting possible excursion.
The superficial flexors of the forearm include all those muscles that originate at the medial epicondyle by a common tendon (Fig. 2.11). The pronator teres, flexor carpi radialis, palmaris longus, flexor carpi ulnaris and flexor digitorum superficialis muscles all belong to this group (superficial to deep).
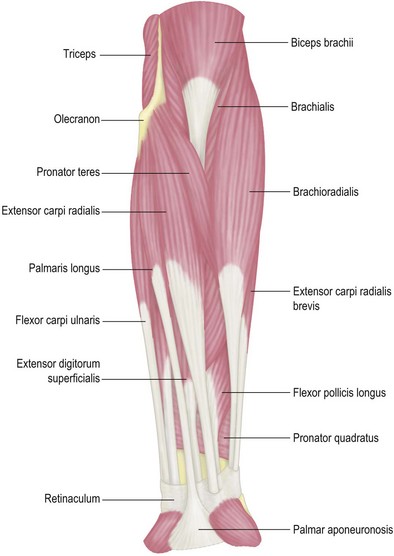
Figure 2.11 Flexors of the forearm, superficial muscles.
Redrawn with permission of http://www.graysanatomyonline.com, Elsevier Ltd. Chapter IV. Myology. 7e Fig. 414.
The palmaris longus originates from the medial epicondyle, medially to the flexor carpi radialis. It also springs from the adjacent intermuscular septa and the deep fascia. This structure has a long tendon, ending in a flat sheet, connecting the muscle with the palm. Distally, the tendon of the palmaris longus attaches to the flexor retinaculum. Here the tendon lies medial to the flexor carpi radialis and superficial to median nerve. The palmaris longus tendon is important in that it can be used as a graft for collateral ligament reconstruction. It is of note, however, that this tendon is absent in approximately 15% of people.18,19
The final muscle of the superficial forearm muscles group is the flexor digitorum superficialis (or flexor digitorum sublimis). This muscle is situated deep to the preceding muscles, and is the largest muscle of the group. Its origin is again formed by two heads: the humero-ulnar head and the radial head. The humero-ulnar head arises from the common tendon, the anterior band of the ulnar collateral ligament, the adjacent intermuscular septa and the medial side of the coronoid process (proximal to the origin of the pronator teres). The radial head arises from the anterior radial border, between the radial tuberosity and the insertion of pronator teres (Fig. 2.11).
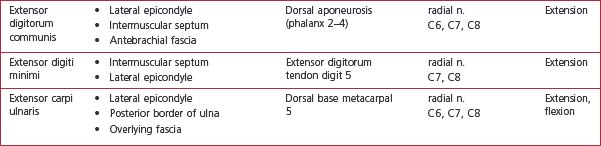
The superficial extensor group of the forearm contains the following structures: the extensor carpi radialis longus and brevis, the extensor digitorum communis, the extensor digiti minimi and the extensor carpi ulnaris (Fig. 2.9). All these muscles, except the carpi radialis longus, originate from the lateral humeral condyle through a common extensor tendon.
The last structure belonging to the superficial extensor group is the extensor carpi ulnaris. This extensor muscle arises via the common extensor tendon, the posterior border of the ulna (through an aponeurosis, shared with the flexor carpi ulnaris and flexor digitorum profundus muscles) and overlying fascia (Fig. 2.11).
Clinical Pearl 2.3
Clinical Pearl 2.4
Neurovascular structures
Neural structures
The most important nerves crossing the elbow are the median, the radial and the ulnar.
The place where the radial nerve pierces the lateral muscular septum is called the lower margin of the radial nerve. Here it runs from the lateral to the anterior aspect of the humerus. The lower margin is located at least 60 mm from the lateral epicondyle. This means that there is a safe zone for placing distal locking screws or fixator pins from lateral to medial within 60 mm of the lateral condyle.18
Vascular structures
Veins
The venous supply of the elbow can be divided into superficial and deep plexi.
The basilic vein is surrounded by branches of the medial cutaneous nerve as it is situated between the biceps and pronator teres muscle, anterior to the elbow. Just distal to the elbow, the median vein of the forearm forms the basilic vein.
1 Alcid JG, Ahmad CS, Lee TQ. Elbow anatomy and structural biomechanics. Clin Sports Med. 2004;23:503-517.
2 Steinberg BD, Plancher KD. Clinical anatomy of the wrist and elbow. Clin Sports Med. 1995;14:299-313.
3 Van Glabbeek F, van Riet RP, Baumfeld JA, et al. The kinematic importance of radial neck length in radial head replacement. Med Eng Phys. 2005;27:336-342.
4 van Riet RP, Van Glabbeek F, Baumfeld JA, et al. The effect of the orientation of the noncircular radial head on elbow kinematics. Clin Biomech (Bristol, Avon). 2004;19:595-599.
5 Miyasaka KC. Anatomy of the elbow. Orthop Clin North Am. 1999;30:1-13.
6 Van Riet RP, Van Glabbeek F, Neale PG, et al. Anatomical considerations of the radius. Clin Anat. 2004;17:564-569.
7 O’Dwyer H, O’Sullivan P, Fitzgerald D, et al. The fat pad sign following elbow trauma in adults: its usefulness and reliability in suspecting occult fracture. J Comput Assist Tomogr. 2004;28:562-565.
8 Cage DJ, Abrams RA, Callahan JJ, et al. Soft tissue attachments of the ulnar coronoid process: an anatomic study with radiographic correlation. Clin Orthop Relat Res. 1995;320:154-158.
9 O’Driscoll SW, Jaloszynski R, Morrey BF, et al. Origin of the medial ulnar collateral ligament. J Hand Surg (Am). 1992;17:164-168.
10 Regan WD, Korinek SL, Morrey BF, et al. Biomechanical study of ligaments around the elbow joint. Clin Orthop Relat Res. 1991;Oct:170-179.
11 Ochi N, Ogura T, Hashizume H, et al. Anatomic relation between the medial collateral ligament of the elbow and the humero-ulnar joint axis. J Shoulder Elbow Surg. 1999;8:6-10.
12 Callaway GH, Field LD, Deng XH, et al. Biomechanical evaluation of the medial collateral ligament of the elbow. J Bone Joint Surg Am. 1997;79:1223-1231.
13 Timmerman LA, Andrews JR. Histology and arthroscopic anatomy of the ulnar collateral ligament of the elbow. Am J Sports Med. 1994;22:667-673.
14 Cohen MS, Hastings HII. Rotatory instability of the elbow: the anatomy and role of the lateral stabilizers. J Bone Joint Surg Am. 1997;79:225-233.
15 Madsen M, Marx RG, Millett PJ, et al. Surgical anatomy of the triceps brachii tendon: anatomical study and clinical correlation. Am J Sports Med. 2006;34:1839-1843.
16 Duchenne GBA. Physiology of motion, demonstrated by means of electrical stimulation and clinical observation and applied to the study of paralysis and deformities. Philadelphia: JB Lippincott; 1949. p. 101–10
17 Hwang K, Han JY, Chung IH. Topographical anatomy of the anconeus muscle for use as a free flap. J Reconstr Microsurg. 2004;20:631-636.
18 Chou PH, Shyu JF, Ma HL, et al. Courses of the radial nerve differ between Chinese and Caucasians : clinical applications. Clin Orthop Relat Res. 2008;466:135-138.
19 Tsai P, Steinberg DR. Median and radial nerve compression about the elbow. J Bone Joint Surg Am. 2008;90:420-428.
20 Lockard M. Clinical biomechanics of the elbow. J Hand Ther. 2006;19:72-80.