22 Supraventricular Tachycardia
I. CASE
A. Fetal echocardiography findings
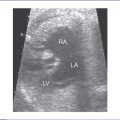
1. Fetal echocardiography reveals situs solitus of the atria, levocardia, and left aortic arch.
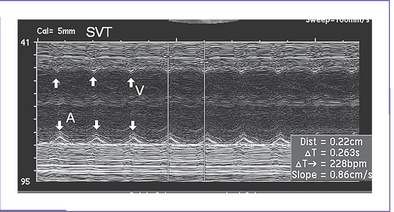
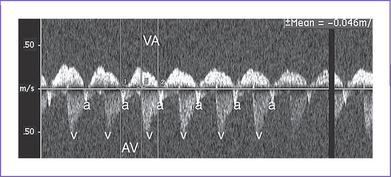
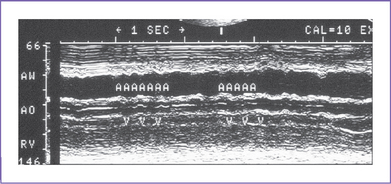
2. Heart rate is 228 bpm, with equal atrial and ventricular rates (Fig. 22-1), suggesting 1:1 ventriculoatrial (VA) or atrioventricular (AV) conduction with a short VA interval (86 ms).
3. Cardiac size is normal (cardiothoracic ratio = 0.33), and cardiac axis and position are normal.
4. The four-chamber view is normal, and ventricles are of equal size.
5. There is no evidence of structural congenital heart disease.
6. The aortic and ductal arches are leftward and of similar size.
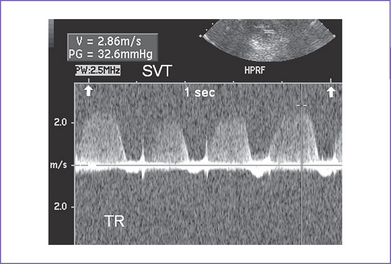
7. Outflow velocities are decreased (0.4 m/s) due to the decreased filling time in tachycardia.
8. The pulmonary venous flow pattern is abnormal (large a wave reversal).
9. Tricuspid and mitral valve holosystolic regurgitation is present (Fig. 22-2), with the additional finding of ascites fluid.
10. Tei indices (myocardial performance index) were not calculated due to the rapid heart rate.
11. The umbilical artery Doppler is normal in the free loop of the umbilical cord with persistent rapid, regular rate.
12. Other venous sites near the heart had large a wave reversal (hepatic vein, ductus venosus), with tachycardia, but the umbilical vein blood velocity has no pulsations.
13. Simultaneous superior vena cava (SVC) and ascending aortic Doppler confirm 1:1 VA association, with a shorter VA than AV interval.
C. Associated syndromes and extracardiac anomalies
None. The detailed level-2 obstetric ultrasound scan was completely normal.
D. Fetal management and counselling
1. Amniocentesis is not indicated. The risk from this procedure is higher than the chance of trisomy with SVT.
2. Initial management of the fetal SVT.
a. Hospital admission was advised for monitoring the fetal heart rate and the mother’s health during administration of antiarrhythmic medications.
b. The mother was fully evaluated by adult cardiology with a baseline electrocardiogram (ECG) and echocardiogram to exclude obvious cardiac pathology that would place her at risk in administering antiarrhythmic medications. Thyroid function testing was normal.
c. Management of the fetal SVT was discussed with the mother and her partner. It was explained that in more than 80% of patients, control of the dysrhythmia is possible, but occasionally this requires more than one medication and monitoring until the mother is on a sufficient dose of the medication that controls the fetal dysrhythmia.
d. With or without rhythm control, there is a small risk of a sudden fetal event or the development of fetal hydrops (particularly without control) as well as risks of other morbidities (e.g., stroke).
3. Daily fetal echo assessments included:
a. Progression of hydrops signs (pleural effusion, ascites, increasing pericardial fluid).
b. Increasing size indicating compromise of heart function.
c. Valve function for increasing degrees of tricuspid and mitral regurgitation. The dP/dt (change in pressure per change in time) can be assessed on AV valve regurgitation jets. Normal is greater than 1000 mm Hg per second, and a poor prognosis is associated with values less than 400 mm Hg per second.
d. Semilunar valve regurgitation, which is a sign of progression in myocardial dysfunction.
e. Myocardial function, which can be measured with the Tei index in sinus rhythm after conversion.
f. Venous Doppler assessment for signs of improvement.
a. Baseline maternal 12-lead ECG was performed, which showed a prolonged PR interval of 0.25 seconds with no other abnormality and normal QTc.
b. The mother was tested (hematology) for hyperthyroidism and infection. Consultation with adult cardiology was obtained, and her exam and echocardiogram were normal.
F. Neonatal management
1. On admission, the neonate was active, with no obvious malformation and normal vital signs.
2. The baby was normal and had a normal ECG with preexcitation.
3. Endocrinology consultation was obtained, and thyroid studies were performed; results were normal.
4. A 24-hour Holter monitor was normal.
H. Outcome of this case
a. The newborn had appropriate birth weight and Apgar scores of 9 at 1 minute and 9 at 5 minutes.
b. The baby was monitored in the intensive care unit (ICU) for 24 hours, and the rhythm was normal at 130 to 150 bpm.
d. Postnatal echocardiogram confirmed a structurally normal heart. The rhythm was normal sinus rhythm.
e. He was started on digoxin 5 mg/kg PO twice daily, and feeding was started.
f. He was discharged after 2 days.
g. Cord blood digoxin level was 80% for the newborn postnatal value.
h. The ECG was normal at all visits with no sign of a delta wave.
i. The baby was followed in cardiology every 2 months with ECG and Holter monitor, and digoxin dose adjustments were made based on weight increase.
j. At 1 year of age the digoxin was stopped.
II. YOUR HANDY REFERENCE
A. Prevalence
1. The actual prevalence of fetal tachyarrhythmia is not known.
a. The most common fetal tachycardia is SVT, which accounts for 90% of fetal tachycardia.
b. The second most common form of fetal tachycardia is atrial flutter and is seen in 10% to 30% of patients. Atrial pulsations in the IVC at greater than 400 bpm are a clue to the diagnosis.
c. Ventricular tachycardia in the fetus is relatively rare and accounts for less than 5% of fetal tachycardia. One clue to this diagnosis is a tachycardia rate of less than 225 bpm with signs of congestive heart failure (CHF).
2. Fetal arrhythmia can occur at any gestational age, but it is most commonly seen after 24 weeks of pregnancy. Tachycardia before 20 weeks of gestation raises the likelihood of infection or maternal drug ingestion or hyperthyroidism.
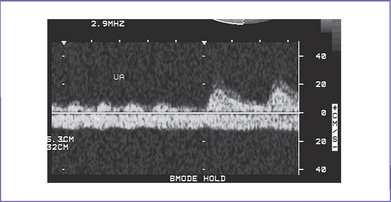
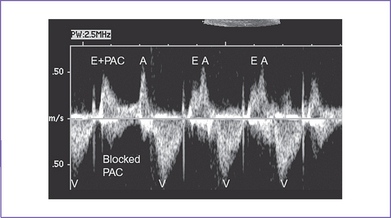
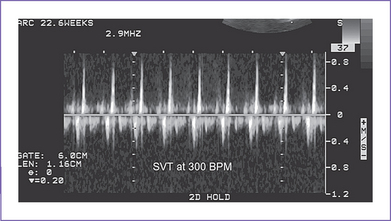
3. The risk of tachycardia is highest in fetuses with multiple blocked atrial premature beats leading to a low ventricular rate (atrial bigeminy). The vast majority of fetuses with atrial and ventricular premature beats without tachycardia have uneventful prenatal and postnatal outcome. Intermittent SVT should be monitored to assess what portion of the whole day the fetus is in SVT (Fig. 22-3).
4. Fetal tachycardia is associated with structural cardiac anomalies in 1% to 5% of cases.
a. The most commonly described associations with SVT are Ebstein’s anomaly and myocardial tumors, particularly rhabdomyoma.
b. Myocardial tumors and cardiomyopathy may be present in fetal ventricular tachycardia.
B. Outcome
1. In fetuses with SVT who were treated in utero, the postnatal outcome is complicated by recurrence of tachyarrhythmia in about 50% of the neonates.
2. In only 10% to 20% of infants does the tachycardia persist beyond the first year of life.
3. Fetal atrial ectopic (AET) and permanent (paroxysmal) junctional reciprocal tachycardia (PJRT) often persist after birth, and long-term antiarrhythmic therapy or electrophysiologic intervention may be necessary.
4. At 1 year of age, roughly one third of fetal SVT patients remain clinically symptomatic. One third do not have clinical tachycardia, but tachycardia can be induced using esophageal stimulation. In one third, tachycardia can no longer be induced, and presumably the bypass tract no longer conducts.
C. In utero diagnosis of fetal tachyarrhythmia
1. The majority of fetal tachyarrhythmias are detected during Doppler assessment of the fetal heart beat at routine obstetrics clinic visits in the second and third trimesters of pregnancy.
2. If monitoring of the fetal heart rate by ultrasound, continuous wave Doppler, or cardiotocography reveals, at any point, fetal arrhythmia (an irregular, rapid, or slow fetal heart rate), one should consider referring the mother for further evaluation by fetal ultrasound and fetal echocardiography. For persistently high or low rates at assessment, the referral should be immediate, given the potential risk of compromise and need for accurate diagnosis to plan management and intervention where possible.
3. Polyhydramnios and fetal hydrops can lead to detection of an underlying fetal tachyarrhythmia and should be considered in the setting where there is unexplained fetal hydrops. One might even consider continuous fetal heart rate monitoring or frequent Doppler assessment every day to exclude or confirm fetal tachyarrhythmia as a primary cause.
D. Mechanisms of fetal arrhythmias
1. The definition of an abnormally fast heart rate depends on the gestational age of the fetus.
a. The fetal heart rates that have been observed in normal pregnancy are 90 bpm at 6 weeks, increasing to 160 to 180 bpm by 9 weeks.
b. The heart rate falls to 140 bpm ± 20 bpm by 20 weeks, and again to 130 bpm ± 20 bpm near term.
c. A fetal heart rate in excess of 180 bpm is abnormal.
2. The high incidence of atrioventricular reentry tachycardia (AVRT) or, similarly, unidirectional reciprocating accessory pathway tachycardia (URAP) during fetal and neonatal life and its decrease due to the spontaneous disappearance of SVT can suggest immaturity of the myocardium. In particular, these tachycardias suggest a delayed development of the annulus fibrosus and/or prolonged persistence of accessory AV pathways.
3. Fetal atrial flutter is rare, and atrial fibrillation to date has not been reported in a fetus.
a. Atrial flutter is generated within the atria by an atrial reentrant circuit and is observed mainly during the third trimester. This supports the hypotheses of an atrial macroreentry as an underlying mechanism of fetal atrial flutter.
b. It might resolve spontaneously or progress to hydrops and death.
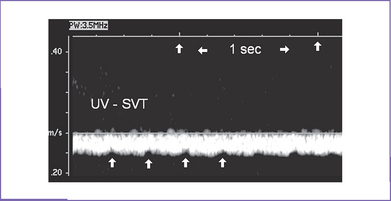
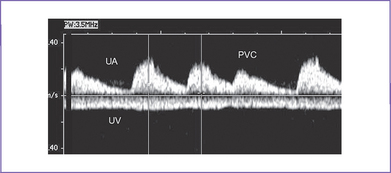
c. Incessant heart rates as high as 300 bpm can lead to hydrops in 2 to 3 days (Fig. 22-4) and manifest umbilical venous pulsations.
4. The pathophysiology in SVT of the human fetus includes an impeded ventricular filling due to a short, inadequate diastolic period. This can alter the ventricular filling either directly or by changes in diastolic ventricular function due to inadequate oxygen supply by the reduced myocardial flow. Both mechanisms can elevate the venous pressure, resulting in increased rates of transcapillary fluid filtration into the interstitial space and significant reduction of lymphatic flow. This inadequate reduction in lymphatic drainage results in interstitial edema and finally hydrops (Box 22-1).
E. Classification of arrhythmias
1. Irregular fetal heart rhythms.
a. Irregular fetal heart rhythms are usually detected during routine auscultation of the fetal heart. Mothers most of the time are asymptomatic.
b. The auscultatory findings are usually reported as “missed beats” or “extra beats.”
c. An irregular fetal rhythm is usually due to the presence of premature atrial or ventricular beats that are intermittent. With premature atrial contractions (PACs) there may be conduction or lack of conduction to the ventricle.
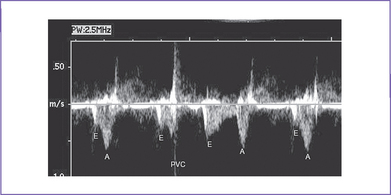
d. Premature ventricular contractions (PVCs) are much less common. A premature atrial contraction may be followed by a premature ventricular contraction.
a. The definition of an abnormally fast heart rate depends on the gestational age of the fetus.
b. The fetal heart rates that have been observed in normal pregnancy are:
a. Bradycardia is defined as rhythms that are slower than normal for gestation.
b. In general, these rhythms may be intermittent, as is true for transient sinus bradycardia or sustained bradycardia (e.g., heart block) (see Chapter 23).
F. Classification of premature beats
1. An irregular fetal heart rate usually represents PACs or, less commonly, PVCs, which are beats that originate from the atrium or ventricle, respectively, from a site other than the normal central conduction system (e.g., sinus node).
2. PACs might or might not be conducted to the ventricle through the AV node.
a. When there is conduction through the AV node following a PAC, the pause that seems to occur between the PAC and the next sinus beat has the same time interval as two sequential sinus beats.
b. The PAC is thought to reset the pace of the sinus rhythm. Alternatively, the PAC may be blocked at the AV node as a result of the AV node’s having not fully recovered from the previous beat.
c. PACs can occur frequently, every two or three beats (atrial bigeminy or trigeminy, respectively).
d. Although there is beat-to-beat variability in sinus rhythm, it does not have such a distinct pattern as observed in atrial bigeminy or trigeminy.
3. PVCs are occasional extra systoles of ventricular origin in the fetus.
a. In premature ventricular beats, the ventricular contraction occurs before the atrial contraction by M-mode and can be easily documented.
G. Classification of fetal tachycardias
a. In extrauterine life, narrow QRS supraventricular tachycardia (SVT) is classified according to the relation of P waves to QRS complexes.
b. During intrauterine life, such classification is not possible due to the very low voltage of P waves on the currently available transmaternal fetal ECG. Thus, we rely on flow signals and mechanical action of the atria and ventricles to provide indirect clues to the arrhythmia mechanism.
c. Tachyarrhythmias can be divided into supraventricular (short and long VA tachycardias and atrial flutter), junctional (junctional ectopic tachycardia), and ventricular types.
2. Supraventricular tachyarrhythmias.
a. Fouron and colleagues (2003) suggest an echocardiographic classification using the measurement of AV and VA time intervals (Doppler velocimetry) (Fig. 22-5). This measurement shows the relationship between the atrial (beginning of the a wave on the SVC or mitral inflow Doppler) and ventricular contractions (beginning of the aortic wave).
3. Junctional ectopic tachycardia.
a. In this tachyarrhythmia, the atrial contractions can occur simultaneously with the ventricular contractions.
b. There is usually a warm-up and slow-down period.
c. This is a very rare form of fetal SVT.
a. Prenatal ventricular tachycardia is very rare but occasionally may be seen in isolation, in association with cardiomyopathies and tumors, long QT syndrome, and in myocardial ischemia.
b. It may be a manifestation of long-QT syndrome, although this diagnosis is more often associated before birth with persistent fetal bradycardia.
c. There may or may not be 1:1 conduction in ventricular tachycardia. If there is not, which is most common, the atrial rates are slower than the ventricular rates.
H. Ultrasound and echocardiographic assessment of dysrhythmias
a. To evaluate cardiac rhythm by M-mode, the cursor is placed across the wall of the right atrium (particularly the right atrial appendage) and through one of the ventricles.
b. This technique demonstrates the relationship of atrial to ventricular contractions, and from this mechanical assessment the atrial and ventricular activation can be inferred.
c. This method is used to evaluate all types of fetal arrhythmias.
2. Doppler assessment of fetal dysrhythmias.
a. Pulsed Doppler interrogation may be used to determine the mechanism of an arrhythmia.
b. At times, simultaneous Doppler interrogation of the LV inflow and outflow can also assist in defining the mechanism of an arrhythmia, but there is potential for error in this technique when there is no flow through the AV valve as a consequence of ventricular contraction.
c. Doppler assessment of umbilical artery flow is a rapid method for determining ventricular rate.
d. Doppler assessment of systemic veins or ductus venosus is a rapid way to determine atrial rate.
e. Doppler assessment of umbilical vein: Normally, this blood flow velocity pattern is flat, but in SVT with heart failure, pulsations may be transmitted back to the cord vein.
3. Ultrasonographic investigation of fetal arrhythmia.
a. With M-mode, atrial and ventricular depolarizations are identified by their mechanical consequences.
c. With Doppler, atrial and ventricular depolarizations are identified by their hemodynamic consequences.
d. Drawbacks with both M-mode and Doppler approaches in electromechanical delay and isometric contraction time are included in the AV interval measurement.
e. For more details on ultrasonographic investigation of fetal arrhythmia, see Table 22-1 and Figures 22-6 to 22-9.
a. This system can detect the minute magnetic fields set up by the electrical discharge from the conducting tissue.
b. Processing of the signal allows separation of the maternal and fetal signals.
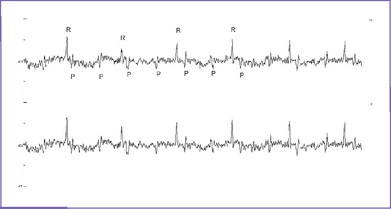
c. AV dissociation can be confirmed by identifying the P and R waves (Fig. 22-10).
5. Fetal electrocardiography: With current technology, about 60% of fetuses can have averaged ECG tracings to determine the AV relation and the Q-T interval.
6. Fetal ECG monitor (FEMO) and Qnetics data.
a. With irregular arrhythmias, this technique performs poorly.
b. At ventricular rates greater than 200 bpm or within the range of the maternal heart rates, assessment of dysrhythmias is not always possible with programs that are currently available.
TABLE 22-1 ULTRASONOGRAPHIC INVESTIGATION OF FETAL ARRHYTHMIA II
| Arrhythmia | M-Mode | Doppler Sampling Site |
|---|---|---|
| PAC | Early atrial wall contraction | LV inflow/outflow: Increase in E wave amplitude (E+PAC) and pause (Fig. 22-6). SVC-Ao Doppler shows an early a wave, occurring earlier than previous sinus beat a waves With (conducted) or without (blocked) ventricular outflow or aortic flow signals |
| PVC | Early ventricular wall contraction (with or without ejection); normal atrial wall movement |
Early MV closure with early ventricular contraction causes shortened E wave PVC could be identified by the continued presence of regular A contractions in the presence of early activation of the ventricle using LV inflow/outflow Doppler (Fig. 22-7). The resultant effect of the PVC can be seen in the umbilical artery tracing (Fig. 22-8). SVC-Ao Doppler shows early aortic outflow signals without a preceding a wave |
| SVT | 1:1 atrial-ventricular wall movements; high rate >220 bpm |
Ao, aorta; AV, atrioventricular; CHB, complete heart block; PAC, premature atrial contractions; PVC, premature ventricular contractions; SVC, superior vena cava; SVT, supraventricular tachycardia.
I. Cardiovascular profile score
1. Serial assessment of the cardiovascular profile score can be used to monitor the fetus and the state of congestive heart failure. This could be important in timing of delivery and level of intensity of antiarrhythmic therapy.
a. Mortality postnatally is high when the fetus is delivered with a cardiovascular profile score of 5/10 or less.
b. The mortality of fetal SVT and hydrops is 10%. This should be clearly stated to the patient.
c. Sudden fetal demise can occur at any time in the context of such severe disease, with or without complete conversion of the dysrhythmia.
3. The goal of therapy is to convert the tachycardia and to observe improved cardiac function and rising cardiovascular profile score.
4. Support for the myocardium in the form of digoxin therapy prenatally may be indicated with cardiovascular profile scores less than 8/10.
5. Hydrops fetalis can take weeks to resolve after conversion to sinus rhythm, even after improvement in cardiac function.
6. The presence of umbilical venous atrial pulsations is a sign of CHF (see Fig. 22-4).
J. Progression in utero
a. This might resolve spontaneously or progress to hydrops and death.
b. In progression to death, SVT in the fetus leads to a reduction in the diastolic or filling time of the ventricle.
c. Further compromise can occur as myocardial perfusion (which also occurs largely in diastole) is jeopardized, resulting in worsening of ventricular function.
d. Eventually, the central venous pressures might become critically elevated, resulting in increased rate of transcapillary fluid filtration into the interstitial space and significant reduction of lymphatic flow.
e. This inadequate reduction in lymphatic drainage results in interstitial edema and evolution of hydrops.
f. Critically elevated central venous pressures ultimately affect umbilical venous return, leading to placental edema and dysfunction.
g. This results in progressive hypoxemia and further compromise of the fetus.
2. In 1–3% of fetuses with frequent PACs, SVT occurs later in pregnancy so that monitoring of the fetal heart rate is indicated at least twice weekly.
K. Antenatal treatment of fetal tachyarrhythmias (Box 22-2)
1. A multidisciplinary team effort is strongly recommended in the treatment of fetal tachyarrhythmias involving excellent collaboration between perinatal and obstetric, pediatric and fetal cardiology, and neonatal staff. This ensures not only better prenatal care but also anticipation of postnatal issues.
2. Intervention for fetal tachyarrhythmias should be considered in fetuses with:
a. Evidence of cardiovascular compromise (some degree of hydrops). In such fetuses, immediate initiation of therapy is critical because they are at the highest risk for mortality and morbidity.
b. Risk of cardiovascular compromise.
a. Maternal–transplacental therapy is the treatment strategy of choice for most cases because it is effective in the majority of hydropic fetuses.
c. Fetal intramuscular therapy.
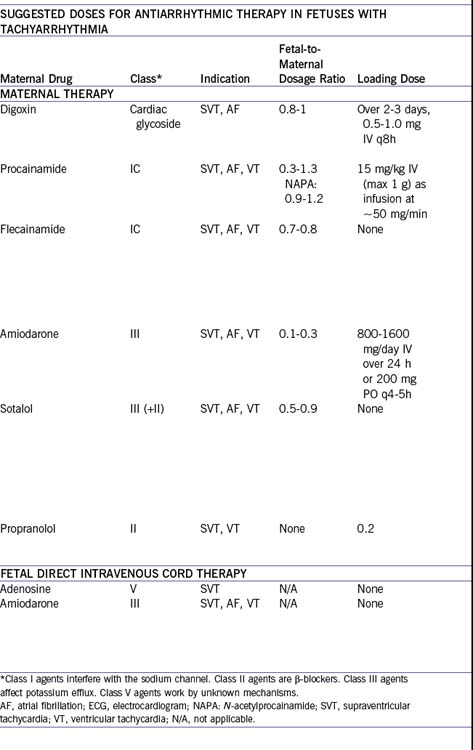
4. Medications that can be used in fetal tachyarrhythmias.
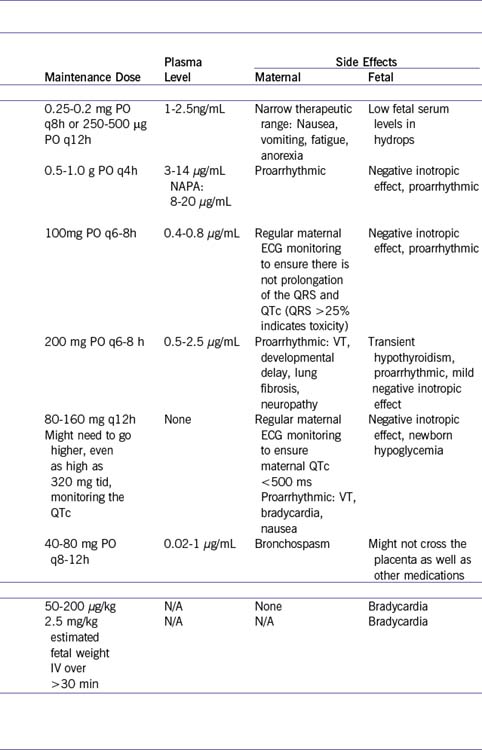
a. Table 22-2 outlines the various medications that have been used successfully to treat fetal tachyarrhythmias. As observed postnatally, no one mediation is effective for all fetuses.
b. In determining which medication to use, one should consider its efficacy for a given dysrhythmia as well as the degree of fetal compromise.
c. Hydropic fetuses can require two or more medications. Often digoxin is used in addition to a stronger medication, such as sotalol, amiodarone, or flecainide, given the negative inotropic effects of these stronger medications.
d. Because there is conversion to sinus rhythm, the fetus might have episodes of bradycardia. Documentation of the mechanism of bradycardia is critical because often it is due to atrial premature beats with AV block (which suggests the medication is working), is usually well tolerated, and should not be an indication for urgent delivery.
5. Immediate perinatal and postnatal management of newborn arrhythmias.
a. Delivery of an affected infant with SVT should be planned through the collaborative efforts and communication among the perinatologist or obstetrician, neonatologists, and cardiologist to be certain the best timing and approach are chosen and the immediate neonatal management is appropriate.
b. With persistent SVT, it may be difficult to monitor the fetus before delivery, given the lack of beat-to-beat variability, and thus some obstetricians consider cesarean section. Early delivery or preterm delivery may be necessary if, despite reasonable attempts at maternal–transplacental or transumbilical therapy, there is inadequate control of the SVT, particularly if the fetus is becoming increasingly compromised.
c. With therapeutic conversion to sinus rhythm, delivery should probably still take place where the infant can be best managed by pediatricians and pediatric subspecialists because the infant could spontaneously convert back into the SVT at delivery or within hours of delivery.
d. At delivery, if the infant is in SVT, the treatment should depend on how compromised the infant is from a cardiovascular standpoint.
e. Once the baby is stable, a baseline 12-lead ECG in and out of the tachyarrhythmia is important to further document the mechanism. For instance, the p wave axis can be very useful in diagnosing concealed pathway SVT, which is usually the reverse of a normal p wave axis in sinus rhythm due to the retrograde conduction, and in diagnosing ectopic atrial tachycardia.
f. SVT (heart rate on monitor of 220-300 bpm).
g. In atrial flutter, the flutter wave might not be visible.
h. Frequent premature contraction.
L. Follow-up
1. Most fetal tachycardia treatment plans include postnatal medication for 6 to 12 months, particularly if the fetus or infant had significant associated cardiovascular compromise. The most common drug is digoxin. Once SVT recurs and is persistent, particularly in childhood, then catheter ablation is indicated.
2. Patients with prolonged QT syndrome should be managed by a pediatric electrophysiologist. Serial monitoring and treatment are indicated because of the risk of ventricular tachycardia and sudden death.
M. Risk of recurrence
1. The familial occurrence of the WPW syndrome has been reported many times.
2. Patients with familial preexcitation had a higher incidence of multiple accessory pathways and possibly an increased risk of sudden cardiac death.
3. Vidaillet and colleagues (1987) suggested that an autosomal dominant factor is involved.
III. TAKE-HOME MESSAGE
A. Diagnosis
1. M-mode and Doppler interrogation can indirectly assist in defining the mechanism of the dysrhythmia.
2. The most common cause of fetal tachyarrhythmia is SVT, usually due to URAP or concealed accessory pathway with a shorter VA interval than AV interval.
3. Atrial flutter is the second most common fetal tachyarrhythmia encountered.
4. Consider serial assessment of pregnancies with frequent fetal PACs given the risk of SVT.
5. SVT can occur with Ebstein’s anomaly and other causes of significant AV valve regurgitation or in any situation in which there is atrial enlargement and tumors.
6. In unexplained fetal heart failure or nonimmune hydrops, fetal heart rate monitoring over a prolonged period can assist in confirming this potentially treatable diagnosis.
7. Venous Doppler velocimetry should be assessed with caution in the fetus with SVT or atrial flutter because often there is significant a wave reversal even to the ductus venosus. Umbilical vein pulsations, however, may be most consistent with significantly elevated central venous pressures and impending hydrops or heart failure.
8. After cardioversion to sinus rhythm, assessment of venous Doppler indices is the best method to assess cardiac function.
B. Treatment
1. Transplacental therapy is effective and converts SVT (even with hydrops) in more than 80% of cases.
2. Given the success of maternal–placental therapy even in the presence of hydrops, an aggressive trial of therapy for fetal SVT, particularly when the fetus is preterm, is warranted.
3. There are several mechanisms of fetal SVT. Treatment strategies should take into consideration the likelihood of success for a given mechanism and the degree of fetal compromise. Although digoxin is an easily administered medication, it might not be effective for every case and might not act rapidly enough in isolation for the grossly hydropic fetus.
4. In the treatment of fetal SVT, the mother’s health should be monitored very closely.
Fouron JC, Fournier A, Proulx F, et al. Management of fetal tachyarrhythmia based on superior vena cava/aorta Doppler flow recordings. Heart. 2003;89(10):1211-1216.
Frohn-Mulder IM, Stewart PA, Witsenburg M, et al. The efficacy of flecainide versus digoxin in the management of fetal supraventricular tachycardia. Prenat Diagn. 1995;15(13):1297-1302.
Hansmann M, Gembruch U, Bald R, et al. Fetal tachyarrhythmias: Transplacental and direct treatment of the fetus—a report of 60 cases. Ultrasound Obstet Gynecol. 1991;1(3):162-168.
Li Z, Strasburger JF, Cuneo BF, et al. Giant fetal magnetocardiogram P waves in congenital atrioventricular block: A marker of cardiovascular compensation? Circulation. 2004;110(15):2097-2101.
Massumi RA. Familial Wolff–Parkinson–White syndrome with cardiomyopathy. Am J Med. 1967;43:951-955.
Schade RP, Stoutenbeek P, de Vries LS, Meijboom EJ. Neurological morbidity after fetal supraventricular tachyarrhythmia. Ultrasound Obstet Gynecol. 1999;13(1):43-47.
Simpson JM, Sharland GK. Fetal tachycardias: management and outcome of 127 consecutive cases. Heart. 1998;79(6):576-581.
Sonesson SE, Fouron JC, Wesslen-Eriksson E, et al. Foetal supraventricular tachycardia treated with sotalol. Acta Paediatr. 1998;87(5):584-587.
Strasburger JF, Cuneo BF, Michon MM, et al. Amiodarone therapy for drug-refractory fetal tachycardia. Circulation. 2004;109(3):375-379.
Van Engelen AD, Weijtens O, Brenner JI, et al. Management outcome and follow-up of fetal tachycardia. J Am Coll Cardiol. 1994;24(5):1371-1375.
Vidaillet HJJr, Pressley JC, Henke E, et al. Familial occurrence of accessory atrioventricular pathways (preexcitation syndrome). N Engl J Med. 1987;317:65-69.
Wheeler T, Murrills A. Patterns of fetal heart rate during normal pregnancy. Br J Obstet Gynaecol. 1978;85(1):18-27.
Zales VR, Dunnigan A, Benson DWJr. Clinical and electrophysiologic features of fetal and neonatal paroxysmal atrial tachycardia resulting in congestive heart failure. Am J Cardiol. 1988;62(4):225-228.