Chapter 8 Supracondylar Fractures of the Humerus in Children
Introduction
Supracondylar fractures of the distal humerus are a commonly encountered injury in children. The association with neurovascular compromise and the potential problems of accurately reducing a displaced fracture can make treatment difficult particularly for the unwary surgeon. While outcome can still be poor following this injury, changes in the management of these fractures over the last three decades have significantly reduced the risks and morbidity with which they were previously associated. Non-operative treatment of displaced fractures has been replaced by fracture stabilization with wires and it is this that has resulted in improved outcomes.1,2
Background/aetiology
Ambulant children of any age are vulnerable to supracondylar humeral fractures but the peak incidence occurs between the ages of 5 and 7 years, with the left arm most commonly affected. Boys sustain the majority of fractures but the gender gap is narrowing, reflecting a change in childhood activity.3
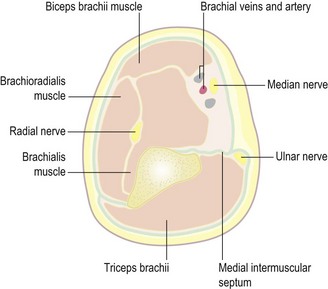
Coincidental injury to any of the three major peripheral nerves around the elbow can occur and has a reported incidence of up to 15%. It may be detected immediately following the injury or may not be noted until after the subsequent treatment.4 The anterior interosseous nerve appears to be the most susceptible to damage from the original injury and radial nerve dysfunction is slightly less common.5 The ulnar nerve is the most vulnerable to iatrogenic injury from medial wire fixation.
Associated ipsilateral fractures need to be excluded but are rare (5%).6 The vast majority of supracondylar fractures are closed (99%), with major vascular injury occurring in 3% or fewer children.7
Pathogenesis of injury
The fracture line is usually transverse in the sagittal and coronal planes but a more oblique fracture line in either plane should alert the surgeon to the potential for greater difficulty in obtaining and maintaining a sound reduction.8
The far less common (5%) flexion type supracondylar fracture results from a fall onto the point of the olecranon with the elbow flexed. Completely displaced flexion fractures can be very challenging to reduce and are associated with a risk of ulnar nerve damage (Fig. 8.1).
It is of interest to note that children who sustain a supracondylar fracture do not have a greater range of elbow hyperextension than those who sustain a fracture of the distal radius.9
Classification
Gartland10 grouped extension type fractures into undisplaced, moderately and severely displaced in his original paper in 1959. This was subsequently modified by Wilkins4 into types I to III as follows:
Leitch et al11 proposed adding a type IV to describe the rarer but highly challenging severely displaced fracture with no intact periosteal hinge. The resulting multidirectional instability only becomes apparent under anaesthesia. From a practical point of view the introduction of this additional category does not influence the management, which is the same as for a type III injury.
Presentation, investigation and treatment options
If there is no actual or imminent soft tissue or neurovascular compromise then a moderate delay before reduction of a displaced supracondylar fracture is permissible (see later section on timing of reduction of type III fractures). In this situation the splinted limb should be rested on a pillow to provide some elevation, with regular reassessment until reduction can be performed. Increasing pain despite normal amounts of analgesia should alert the surgeon to the possibility of compartment syndrome or deteriorating limb perfusion.
Displaced supracondylar fractures can be seen readily on standard AP and lateral radiographs. Undisplaced fractures may be harder to see but the presence of a posterior fat pad sign is suggestive of the diagnosis. Any suspicion of coincident fractures indicates the need for radiographs of the whole forearm or upper limb (Fig. 8.5).
Surgical techniques and rehabilitation
Type I fractures
These injuries are usually managed with a posterior splint or a collar and cuff sling. The elbow should be flexed to at least 90°, provided that swelling permits. Ballal et al12 found their patients were more comfortable in a plaster backslab and suggested that this was preferable to a simple sling. Whichever method is chosen, a follow-up radiograph at 5–7 days to ensure displacement has not occurred is recommended.
Type II fractures
Some controversy exists as to the indications for operative reduction and stabilization in this group. Extension of the fracture to a point where there is no intersection of the capitellum by the anterior humeral line would be considered by most to be an indication for reduction. Lesser degrees of extension may be remodelled by younger children but children beyond the age of 3–5 years have limited remodelling potential in the distal humerus. Some studies13 have suggested that splintage in flexion of more than 90° is all that is required in most cases of reduced type II fractures. Maintenance of the elbow in a splint at more than 90° is difficult, however, because of swelling, and loss of reduction can occur in a significant proportion. The risk of neurovascular complications also increases with flexion of the injured elbow beyond 90°. For these reasons many now advocate stabilization with K-wires after reduction of type II fractures.14
Type III fractures
The good results obtained with closed reduction and percutaneous pinning has meant that the majority of surgeons prefer this option for type III fractures. Olecranon pin or straight-arm traction has compared poorly with percutaneous pinning because of the higher rates of malunion.15 Others have reported reasonable results from traction, but the prolonged inpatient stay makes this option less desirable.16
Timing of reduction of type III fractures
Loizou et al17 identified five recent non-randomized retrospective studies18–22 that considered the effects of delay on the treatment of type III fractures. From these papers Loizou et al analysed 396 patients (243 in the early treatment group and 153 in the delayed treatment group). The distinction between early and delayed treatment was 8 h in the reports of Iyengar et al,18 Carmichael et al19 and Walmsley et al20, and 12 h in those of Gupta et al21 and Sibinski et al.22 Loizou et al found that the failure of closed reduction and conversion to open reduction was significantly higher in the delayed-treatment groups. They concluded that type III fractures should be treated within 12 h of injury. The Walmsley et al study originated from our department and the 8 h delay was defined from the patients’ arrival in the accident and emergency department. This time period was used because of the difficulty in identifying the timing of the injury. All fractures were either treated or supervised by a consultant, which was apparently not the case in the other papers considered by Loizou et al.
Closed reduction and fixation of displaced extension supracondylar fractures
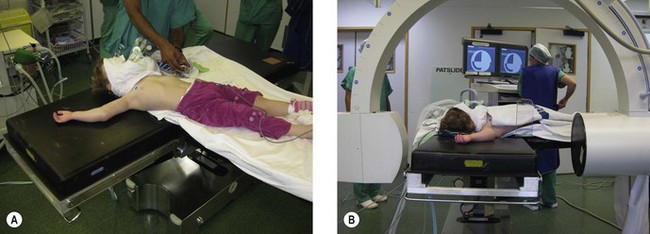
The operating table should be positioned in such a way that the surgeon has plenty of room and the image intensifier can gain easy access (Fig. 8.6). Children older than 3 or 4 years usually have sufficiently long arms to allow positioning in a conventional way with their arm extended on an arm table. Sufficient room must be available around the arm table for the image intensifier to swing through 90° to provide AP and lateral views without moving the injured arm. Rotation of the arm to obtain a lateral view can result in displacement of a reduced fracture and should be avoided.
Clinical Pearl 8.1
For younger children it can be more difficult to view the elbow on an arm table as the image intensifier cannot be positioned close enough to the operating table. For children under 4 years the authors therefore recommend the set-up shown in figure 8.6.
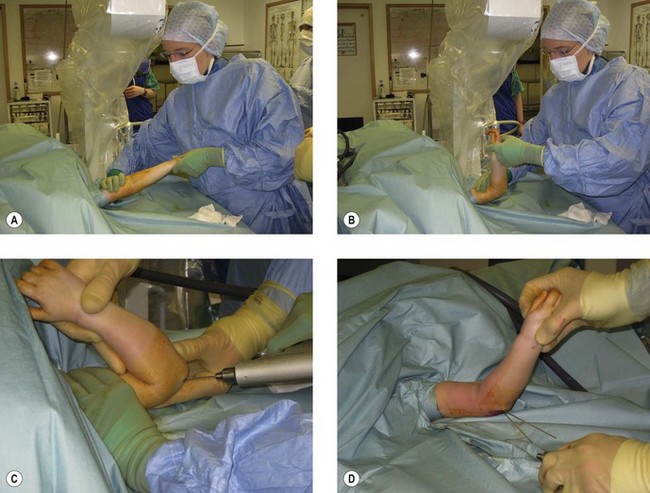
Perhaps the most important aspect of reduction is patience. Firm, continuous but gentle longitudinal traction should be applied to the supinated, extended arm for approximately 1 min as described by Charnley.23 Sufficient distraction of the fragments can then be assessed by obtaining an AP fluoroscopy view.
This will also allow the surgeon to assess the degree of any residual lateral or medial displacement of the distal fragment, which can be corrected at this point while the elbow is fully extended. Any puckering of the skin in the antecubital fossa should have disappeared by this stage. If it has not, traction should be relaxed as the bicipital aponeurosis or other structures may have been pulled tightly around the metaphyseal end of the proximal fragment and only relaxation of these tissues will allow this to be manipulated away from the subcutaneous tissues. An inability to reduce the metaphysis back through the anterior tissues is an indication for open reduction and flexion of the elbow should not be attempted. If incarceration of the metaphyseal end of the proximal fragment is not a problem the surgeon can continue with the reduction manoeuvre. Longitudinal traction is maintained as the elbow is gradually flexed while the olecranon is pushed forwards in relation to the humeral shaft (Fig. 8.7). The elbow should flex beyond 90° with little resistance. If resistance is encountered this may indicate inadequate reduction in the sagittal or coronal planes or soft tissue entrapment. In this situation the elbow should be returned to the extended position and reassessed.
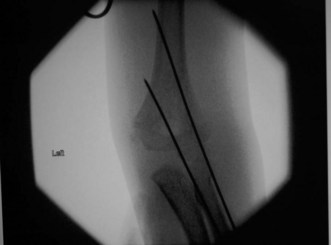
Pin configuration
Several recent studies have considered pin configuration for Gartland type III extension supracondylar fractures. Crossed K-wires are associated with an approximate 5% incidence of iatrogenic ulnar nerve injury.24. Brauer et al25 concluded from a systematic review comparing two laterally based pins with one medial and one lateral pin that the medial/lateral technique gave superior stability but a fivefold greater likelihood of iatrogenic ulnar nerve damage. Zenios et al26 used two lateral entry pins but at operation tested rotational stability and if this was lacking inserted a third laterally based pin. A medially based pin was inserted only if there was residual instability after inserting the third lateral pin. They concluded that fractures that were rotationally stable at operation were unlikely to displace postoperatively and only a small proportion of fractures were unstable with two lateral pins. Lee et al27 compared three lateral divergent pins with three lateral parallel pins and found that both methods were effective options. Bloom et al28 considered the problem of fracture stability after obtaining an acceptable, but not anatomical, reduction in a laboratory model. They recommended using three divergent lateral pins or two lateral and one medial pin when less than an anatomical reduction was obtained. Laboratory studies do not, however, take into account plaster immobilization and the effect of healing on increasing fracture stability. Sankar et al29 identified three errors of technique in pin fixation: failure to engage both fragments with two pins or more; failure to engage bicortical fixation with two pins or more; and failure to achieve adequate pin separation at the fracture site. They noted that loss of fixation was most likely when two lateral pins were used. Skaggs et al30 and Omid et al24 recommended the use of laterally inserted pins with maximal separation at the fracture site and with engagement of both medial and lateral columns. In addition they advised that the surgeon should have a low threshold for inserting a third lateral pin for additional stability.
Omid et al24 have drawn attention to the problem of medial column comminution in type II fractures and the potential for the later development of cubitus varus.
Elastic intramedullary nailing
The use of antegrade elastic nails introduced through the lateral cortex of the humeral shaft has been advocated by some as providing excellent stability for reduced type III supracondylar fractures. Schaffer et al31 suggested that this technique allowed early mobilization and reduced stiffness, although it should be noted that their series contained a high number of less severe type II fractures.
Authors’ preference for treatment of type II and III fractures
The child is positioned on the operating table as previously described.
For type III fractures a tourniquet is applied but not inflated, and the arm is prepared and draped. This set-up has the advantage that if an open reduction is necessary the tourniquet can be inflated and the patient’s upper limb does not have to be re-prepared and draped. Type II and III extension fractures are pinned using two laterally based diverging K-wires (Fig. 8.8). Rotational stability is checked and a third laterally based wire added if necessary. The upper limb is then placed in a backslab with the elbow at about 70° in case of swelling or vascular embarrassment. The elbow is elevated on a pillow and regular observations made of the limb’s circulation in order to check for evolving neurovascular problems that could be alleviated by early splitting of the backslab and gentle extension of the elbow. The cast is completed before the child is discharged.
Summary Box 8.1 Treatment of extension supracondylar fractures
Closed reduction and fixation of flexion type supracondylar fractures
The flexion pattern accounts for about 5% of all supracondylar fractures. Mahan et al32 reported on 58 patients in one of the largest retrospective case–control studies. All patients had their fracture fixed with K-wires and 31% needed an open reduction. The incidence of preoperative ulnar neuropathy was 19%, compared to 10% in their group of extension type supracondylar fractures. All neurological symptoms resolved fully.
Open reduction of an extension supracondylar fracture
The indications for open reduction include inability to achieve satisfactory reduction by closed methods or persistent vascular compromise following attempted closed reduction. The elbow can be approached anteriorly, medially, laterally or posteriorly, although the latter is less often used in children owing to concern about disrupting the blood supply to the distal humerus. The choice of approach is dependent on the surgeon’s preference and experience. The anterior approach is recommended if exploration of the brachial artery is intended. The anterior and medial approaches will be described (see Chapter 6 for approaches to the elbow).
Complications
Pin track infection
Iobst et al33 have reported an overall infection rate of 2.34% and a deep infection rate of 0.47% based on a literature review of 22 papers. They also reported a semi-sterile technique of percutaneous pinning where, after a reduction has been achieved, the elbow is held by an assistant and the surgeon puts on sterile gloves and prepares the skin around the elbow for percutaneous pinning using a cordless drill. The authors make the point that this is similar to inserting a traction pin at the bedside. They did not have any superficial or deep pin track infections when using this technique in 304 patients, of whom 68% did not receive antibiotics. This report suggests that routine antibiotic prophylaxis for percutaneous pinning of supracondylar fractures may not be necessary.
Vascular impairment
The literature reports about a 10–20% incidence of an absent radial pulse in children presenting with a type III fracture.24 This is not an emergency provided the hand is well perfused, but a pulseless, poorly perfused, mottled hand is an emergency and urgent reduction and fixation are required. Incarceration of the brachial artery should be suspected if there is a rubbery block to reduction, and open reduction and retrieval of the anterior cubital structures from the fracture site are indicated. If reduction and fixation are achieved but the hand remains poorly perfused, anterior exploration of the fracture and artery is indicated. Arterial spasm may improve after retrieval of the artery from the fracture. If circulation is not restored after retrieval of the artery, vascular repair by a vascular or plastic surgeon is indicated.
If the pulse does not return after reduction and fixation but the hand is well perfused (pink pulseless hand) it is reasonable to observe the child’s hand over the next 24–48 h and there is no indication for vascular exploration. Sabharwal et al34 reported on 13 children presenting with a type III fracture and a pink pulseless hand. Four underwent vascular repair and the authors found a high rate of asymptomatic occlusion in the 13 children at follow-up. In contrast, Luria et al35 did not observe late loss of pulse or reocclusion in 11 children reviewed after exploration and repair of the brachial artery. Both studies report on small numbers of children but they suggest that the collateral circulation at the elbow is sufficient to maintain limb viability in a child.
Other more recent papers have considered further the problem of the pink pulseless hand36,37 and have also suggested that it is reasonable to carefully monitor the hand for 24–48 h. If, however, perfusion deteriorates, pain worsens or signs of neurological compromise develop, exploration of the brachial artery and the affected nerve(s) is indicated.38
Neurological impairment
About 20% of children have some neurological impairment associated with a supracondylar fracture. The anterior interosseous nerve is most commonly injured in extension fractures. Nerve exploration is not indicated routinely and the majority recover within 3–7 months.39 Persisting symptoms are an indication for electrical studies and exploration. Ramachandran et al40 reported good results after either neurolysis or excision of neuroma and grafting in patients referred to a specialist referral centre for peripheral nerve injuries.
Compartment syndrome
This is a very rare complication, as evidenced by a recent retrospective report that identified only 11 patients collected from eight hospitals in three countries.41 The authors were not able to document the true incidence of compartment syndrome but stated that in their opinion patients presenting with ‘excessive swelling’ should be regarded as being at increased risk of this complication. Unfortunately, however, a definition of ‘excessive swelling’ was not provided.
Battaglia et al42 reported on factors affecting compartment pressures in supracondylar fractures and found that post-reduction pressures did not rise significantly until the forearm was flexed more than 90°. This suggests that the elbow may be safely immobilized in up to 90° of flexion after fracture fixation. There is, however, a paucity of data on normal forearm compartment pressures and these authors acknowledged this limitation in their study. Elapsed time after injury did affect pressures and the authors concluded that the decision for fasciotomy ‘should not be based solely on pressure values, but on the combination of pressure measurements and clinical evaluation’.
Dissolution of the trochlea
This is a rare sequel to supracondylar fracture and Bronfen et al43 reported six cases out of 280 supracondylar fractures. All children had severely displaced fractures and at follow-up had restriction of movement in their affected elbow and a characteristic fishtail deformity on X-ray. They concluded that, because of the delay between injury and the development of radiographic changes, the dissolution was consistent with avascular necrosis of the trochlea rather than of traumatic origin (Fig. 8.10).
Cubitus varus
Cubitus varus, the gunstock deformity, is the commonest complication of a supracondylar fracture but does not usually affect function (Fig. 8.11). The appearance is a result of a combination of medial rotation of the distal fragment and collapse into medial tilt. Although the angle of the deformity may not change, the increasing length of the child’s arm will give the appearance of a deteriorating deformity.
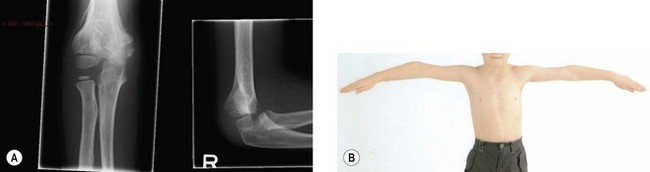
Figure 8.11 Radiograph and clinical picture of cubitus varus following malunion of supracondylar fracture.
The humerocondylar and Baumann’s angles are standard criteria used to assess the quality of reduction after supracondylar fracture. The humerocondylar angle (HCA) is said to be between 35° and 40°, and Simanovsky et al44 have pointed out that the literature concerning the angle is unexpectedly sparse. They performed a cross-sectional study of the HCA from paediatric X-rays and found that the value of the angle was the same (40°) in groups of children whose mean ages ranged from 3 to 12 years. Much of the emphasis of the quality of reduction for supracondylar fractures concerns the coronal and transverse plane components. It is generally assumed that fractures left to heal in some degree of extension, i.e. a loss of the normal 40° humerocondylar angle, are likely to remodel with time, as the deformity lies in the plane of sagittal motion of the elbow. Simanovsky et al45 identified 22 patients out of 223 who had an under-reduction of the extension component of their supracondylar fracture and were available for examination at skeletal maturity. Eleven patients had limited elbow flexion at final follow-up and the authors emphasized the importance of obtaining a satisfactory restoration of the HCA as approximately 80% of humeral growth occurs proximally after the age of 6 years. This leaves little opportunity for remodelling to occur at the elbow.
The Baumann angle (Fig. 8.12) is often used to evaluate coronal plane alignment after supracondylar fracture. Baumann had suggested that the angle derived from lines drawn perpendicular to the long axis of the humerus and the flat part of the distal humeral metaphysis could be related to the carrying angle of the elbow.46 It is often assumed that the Baumann angle has a constant relationship to the carrying angle of the elbow. Mohammad et al46 undertook an elegant mathematical study of the relationship between the Baumann angle and the carrying angle of the elbow. They found that the relationship between the two angles was nonlinear beyond10° of rotation. A coronal X-ray of the elbow in full extension after fracture reduction is necessary to evaluate the Baumann angle correctly and to avoid a misinterpretation.

Figure 8.12 AP radiograph with Baumann’s angle demonstrated. A line perpendicular to the long axis of the humerus and a line drawn along the flat part of the lateral aspect of the distal humeral metaphysic form the angle, which has a range of 64–81°.46 Note the supracondylar fracture.
Correction of the deformity is by a supracondylar osteotomy. One of the more commonly used methods is a closing wedge osteotomy. This has the disadvantage that it does not allow translation of the distal humerus and results in a prominence of the lateral side of the distal humerus and the impression of residual deformity even though the cubitus varus may have been corrected. Tien et al47 have also noted that the osteotomy is usually more proximal than the deformity and the tightness of the medial tissues after a closing wedge osteotomy tends to produce a strong varus moment. Tien et al reported on a dome osteotomy that did not increase the prominence of the lateral condyle after osteotomy and also gave satisfactory radiological and functional outcomes. Their results were confirmed by Pankaj et al’s48 later study. Other satisfactory solutions avoiding a post-osteotomy lateral condylar prominence have been proposed. For example, Laupattarakasem et al49 have described a pentalateral osteotomy which gave good results in 57 patients followed prospectively, and Karatosun et al50 have reported on their experience with the Ilizarov technique in seven children.
Authors’ preference for the correction of cubitus varus
We prefer not to use a closing wedge technique because of the problem of a prominence of the lateral side of the elbow. The dome method47 is technically straightforward and a good result can be anticipated, provided the centre of rotation is identified correctly.
Outcome
The vast majority of children have a good outcome following a supracondylar fracture of the humerus and return to normal function within 2 months of injury.51 Around 5% may have some degree of permanent deformity but in most of these there is no functional impairment.52 However, remodelling of the distal humerus after 5 years of age is limited, suggesting that any loss of motion due to malunion is likely to persist after this age.
1 France J, Strong M. Deformity and function in supracondylar fractures of the humerus in children variously treated by closed reduction and splinting, traction and percutaneous pinning. J Pediatr Orthop. 1992;12(4):494-498.
2 Tellisi N, Abusetta G, Day M, et al. Management of Gartland’s type 3 supracondylar fractures of the humerus in children: the role of audit and practice guidelines. Injury. 2004;35(11):1167-1171.
3 Houshian S, Mehdi B, Larsen MS. The epidemiology of elbow fracture in children: analysis of 355 fractures, with special reference to supracondylar humerus fractures. J Orthop Sci. 2001;6(4):312-315.
4 Kasser JR, Beaty JH. Supracondylar fractures of the distal humerus. In Rockwood and Wilkins’ fractures in children, 6th ed, Philadelphia, PA: Lippincott Williams & Wilkins; 2006:543-590.
5 Lyons ST, Quinn M, Stanitski CL. Neurovascular injuries in type 3 humeral supracondylar fractures in children. Clin Orthop Rel Res. 2000;July(376):62-67.
6 Roposch A, Reis M, Molina M, et al. Supracondylar fractures of the humerus associated with ipsilateral forearm fractures in children: a report of forty-seven cases. J Pediatr Orthop. 2001;21(3):307-312.
7 Noamann HH. Microsurgical reconstruction of brachial artery injuries in displaced supracondylar fracture humerus in children. Microsurgery. 2006;26(7):498-505.
8 Bahk MS, Srikumaran U, Ain MC, et al. Patterns of pediatric supracondylar humerus fractures. J Pediatr Orthop. 2008;28(5):493-499.
9 McLauchlan GJ, Walker CRC, Cowan B, et al. Extension of the elbow and supracondylar fractures in children. J Bone Joint Surg (Br). 1999;81-B:402-405.
10 Gartland JJ. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet. 1959;August:145-154.
11 Leitch KK, Kay RM, Femino JD, et al. Treatment of multidirectionally unstable supracondylar fractures in children: a modified Gartland type IV fracture. J Bone Joint Surg (Am). 2006;88-A:980-985.
12 Ballal MS, Garg NK, Bass A, et al. Comparison between collar and cuffs and above elbow backslabs in the initial treatment of Gartland type 1 supracondylar humerus fractures. J Pediatr Orthop B. 2008;17(2):57-60.
13 Hadlow AT, Devane P, Nicoll RO. A selective treatment approach to supracondylar fracture in children. J Pediatr Orthop. 1996;16(1):104-106.
14 Skaggs DL, Sankar WN, Albrektson J, et al. How safe is the operative treatment of Gartland type 2 supracondylar humerus fractures in children? J Pediatr Orthop. 2008;28(2):139-141.
15 Prietto CA. Supracondylar fractures of the humerus: a comparative study of Dunlop’s traction versus percutaneous pinning. J Bone Joint Surg (Am). 1979;54-A:425-428.
16 Gadgil A, Hayhurst C, Maffuli N, et al. Elevated, straight arm traction for supracondylar fractures of the humerus in children. J Bone Joint Surg (Br). 2005;87-B:82-87.
17 Loizou CL, Simillis C, Hutchison JR. A systematic review of early versus delayed treatment for type III supracondylar humeral fractures in children. Injury. 2009;40:245-248.
18 Iyengar SR, Hoffinger SA, Townsend DR. Early versus delayed reduction and pinning of type III displaced supracondylar fractures of the humerus in children: a comparative study. J Orthop Trauma. 1999;13:51-55.
19 Carmichael KD, Joyner K. Quality of reduction versus timing of surgical intervention for paediatric supracondylar humerus fractures. Orthopaedics. 2006;29:628-632.
20 Walmsley PJ, Kelly MB, Robb JE, et al. Delay increases the need for open reduction of the type-III supracondylar fractures of the humerus. J Bone Joint Surg (Br). 2006;88-B:528-530.
21 Gupta N, Kay RM, Leitch K, et al. Effect of surgical delay on perioperative complications and need for open reduction in supracondylar humerus fractures in children. J Pediatr Orthop. 2004;24(3):245-248.
22 Sibinski M, Sharma H, Bennet GC. Early versus delayed treatment of extension type-3 supracondylar fractures of the humerus in children. J Bone Joint Surg (Br). 2006;88-B:380-381.
23 Charnley J. Supracondylar fractures of the humerus in children. In The closed treatment of common fractures, 4th ed, Cambridge, UK: Colt Books; 1999:105-115.
24 Omid R, Choi PD, Skaggs DL. Supracondylar humeral fractures in children. J Bone Joint Surg (Am). 2008;90-A:1121-1132.
25 Brauer CA, Lee BM, Bae DS, et al. A systematic review of medial and lateral entry pinning versus lateral entry pinning for supracondylar fractures of the humerus. J Pediatr Orthop. 2007;27(2):181-186.
26 Zenios M, Ramachandran M, Milne B, et al. Intraoperative stability testing of lateral-entry pin fixation of pediatic supracondylar humeral fractures. J Pediatr Orthop. 2007;27(6):695-702.
27 Lee YH, Lee SK, Kim BS, et al. Three lateral divergent or parallel fixations for the treatment of displaced supracondylar humerus fractures in children. J Pediatr Orthop. 2008;28(4):417-422.
28 Bloom T, Robertson C, Mahar AT, et al. Biomechanical analysis of supracondylar humerus fracture pinning for slightly malreduced fractures. J Pediatr Orthop. 2008;28(7):766-772.
29 Sankar WN, Hebela NM, Skaggs DL, et al. Loss of pin fixation in supracondylar humeral fractures in children: causes and prevention. J Bone Joint Surg (Am). 2007;89-A:713-717.
30 Skaggs DL, Cluck MW, Mostofi A, et al. Lateral-entry pin fixation in the management of supracondylar fractures in children. J Bone Joint Surg (Am). 2004;86-A:702-707.
31 Schaffer K, Bohm RE, Dietz HG. Elastic intramedullary nailing (ESIN) of supracondylar fractures of the humerus in children. Unfallchirurg. 2007;110(10):852-858.
32 Mahan ST, May CD, Kocher MS. Operative management of displaced flexion supracondylar humerus fractures in children. J Pediatr Orthop. 2007;27(5):551-556.
33 Iobst CA, Spurdle C, King WF, Lopez M. Percutaneous pinning of pediatric supracondylar humerus fractures with the semi-sterile technique: the Miami experience. J Pediatr Orthop. 2007;27(1):17-22.
34 Sabharwal S, Tredwell SJ, Beauchamp RD, et al. Management of pulseless pink hand in pediatric supracondylar fractures of the humerus. J Pediatr Orthop. 1997;17(3):303-310.
35 Luria S, Sucar A, Eylon S, et al. Vascular complications of supracondylar humeral fractures. J Pediatr Orthop B. 2007;16:133-143.
36 Blakey CM, Biant LC, Birch R. Ischaemia and the pink, pulseless hand complicating supracondylar fractures of the humerus in childhood: long-term follow-up. J Bone Joint Surgery (Br). 2009;91:1487-1492.
37 Mangat KS, Martin A, Bache CE. The ‘pulseless pink’ hand after supracondylar fractures of the humerus in children: the predictive value of nerve palsy. J Bone Joint Surg (Br). 2009;91:1521-1525.
38 Robb JE. The pink, pulseless hand after supracondylar humeral fracture in children. J Bone Joint Surg (Br). 2009;91:1410-1412.
39 Culp RA, Osterman AL, Davidson RS, et al. Neural injuries associated with supracondylar fractures of the humerus in children. J Bone Joint Surg (Am). 1990;72-A:1211-1215.
40 Ramanchandran M, Birch R, Eastwood DM. Clinical outcome of nerve injuries associated with supracondylar fractures of the humerus in children: the experience of a specialist referral centre. J Bone Joint Surg (Br). 2006;88-B:90-94.
41 Ramachandran M, Skaggs DL, Crawford HA, et al. Delaying treatment of supracondylar fractures in children: has the pendulum sung too far? J Bone Joint Surg (Br). 2008;90-B:1228-1233.
42 Battaglia TC, Armstrong DG, Schwend RM. Factors affecting forearm compartment pressures in children with supracondylar fractures of the humerus. J Pediatr Orthop. 22(4), 2002. 431–429
43 Bronfen EB, Geffard B, Mallet JF. Dissolution of the trochlea after supracondylar fracture of the humerus in childhood. J Pediatr Orthop. 2007;27(5):547-550.
44 Simanovsky N, Lamdan R, Hiller N, Simanovsky N. The measurements and standardization of humerocondylar angle in children. J Pediatr Orthop. 2008;28(4):463-465.
45 Simanovsky N, Lamdan R, Mosheiff R, et al. Under-reduced supracondylar fracture of the humerus in children: clinical significance at skeletal maturity. J Pediatr Orthop. 2007;27(7):733-738.
46 Mohammad S, Rymaszewski LA, Runciman J. The Baumann angle in supracondylar fractures of the distal humerus in children. J Pediatr Orthop. 1999;19(1):65-69.
47 Tien YC, Chih HW, Lin GT, Lin SY. Dome corrective osteotomy for cubitus varus deformity. Clin Orthop. 2000;380:158-166.
48 Pankaj A, Dua A, Malhtra R, Bhan S. Dome osteotomy for post-traumatic cubitus varus: a surgical technique to avoid lateral condylar prominence. J Pediatr Orthop. 2006;26(1):61-66.
49 Laupattarakasem W, Mahaisavariya B, Kowsuwon W, et al. Pentalateral osteotomy for cubitus varus: clinical experience of a new technique. J Bone Joint Surg (Br). 1989;71-B:667-670.
50 Karatosun V, Aleberov C, Alici E, et al. Treatment of cubitus varus using the Ilizarov technique of distraction osteogenesis. J Bone Joint Surg (Br). 2000;82-B:1030-1033.
51 Wang YL, Chang WL, Hsu CJ, et al. The recovery of elbow range of motion after treatment of supracondylar and lateral condylar fractures of the distal humerus in children. J Orthop Trauma. 2009;23(2):120-125.
52 Mangwani J, Nadarajah R, Paterson JM. Supracondylar humeral fractures in children: 10 years experience in a teaching hospital. J Bone Joint Surg (Br). 2006;88(3):362-365.