48 Superior Hypogastric Plexus Block
Placement
Anatomy
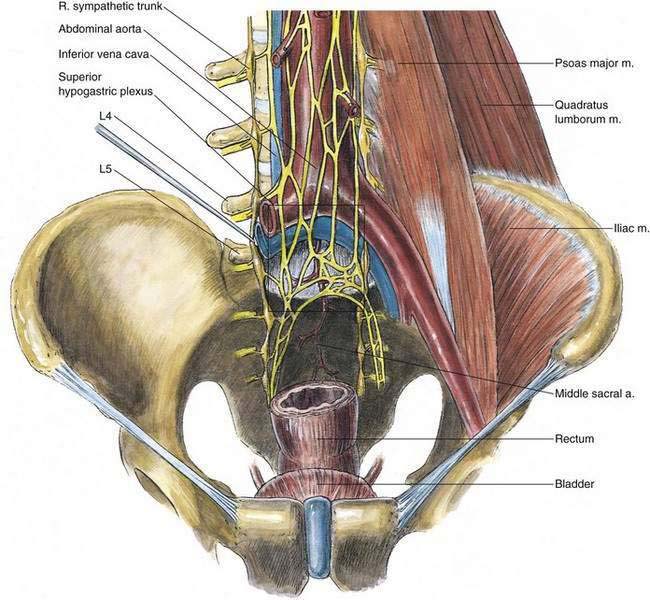
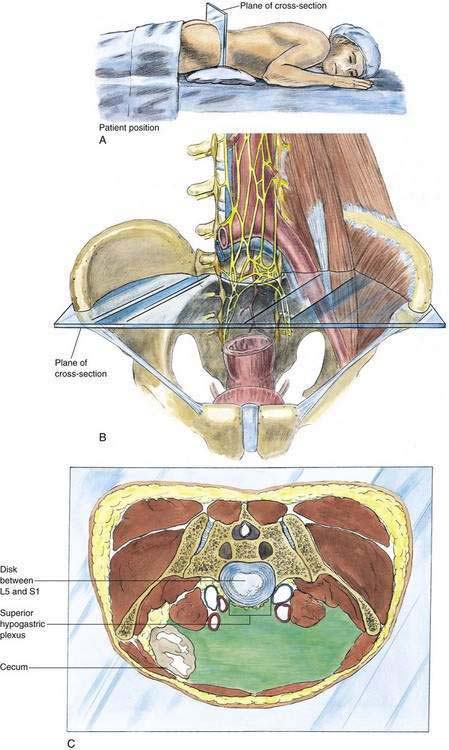
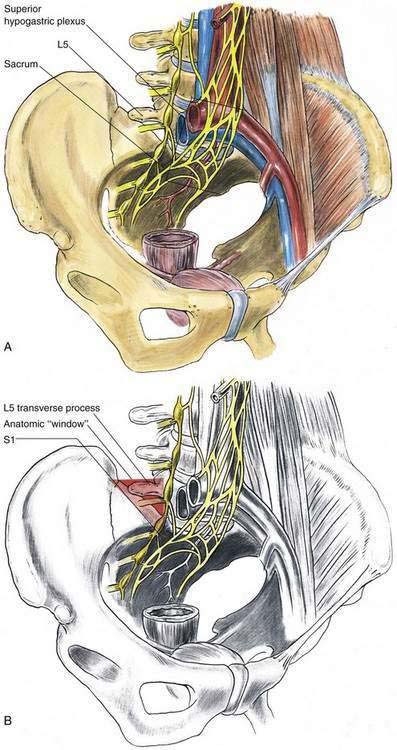
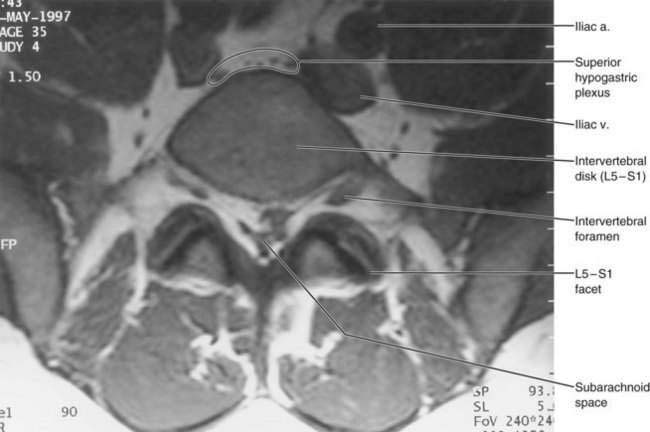
The superior hypogastric plexus is continuous with the intermesenteric plexus and is located retroperitoneally, caudad to the origin of the inferior mesenteric artery. It lies anterior to the lower part of the abdominal aorta, its bifurcation, and the middle sacral vessels; more specifically, it is anterior to the fourth and fifth lumbar vertebrae and the first sacral vertebra. The plexus is composed of a flattened band of intercommunicating nerve bundles that descend over the aortic bifurcation (Figs. 48-1 and 48-2). Broadening below, it divides into the right and left hypogastric nerves. In addition to its continuity with the intermesenteric plexus, the superior hypogastric plexus receives input from the lower two lumbar splanchnic nerves (Fig. 48-3). Figure 48-3 identifies with a red triangle a key concept in the superior hypogastric plexus nerve block. The red triangle highlights the anatomic window between the iliac crest, the L5 transverse process, and the L5-S1 vertebral bodies, which allows successful needle insertion.
Position
Patients undergoing superior hypogastric plexus block are placed prone on a radiographic imaging table with a pillow beneath the lower abdomen to reduce lumbar lordosis (see Fig. 48-2A). Ideally, biplane fluoroscopy is available to assess needle placement, for which oblique posteroanterior and lateral images are needed.
Needle Puncture
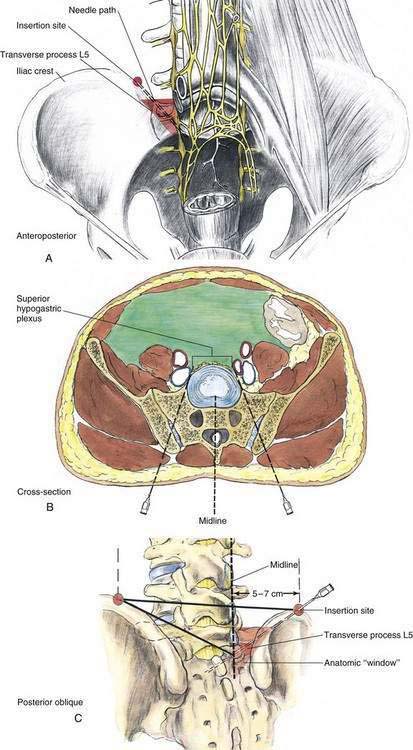
The L4-L5 interspace is identified fluoroscopically and skin marks are placed 5 to 7 cm lateral to the midline at the level of the L4-L5 interspace (Fig. 48-4). This preparation is needed for the insertion of the needles through the area of bony access (shown by the red triangle in Figs. 48-3 through 48-5) to the superior hypogastric plexus. After aseptic skin preparation, skin infiltration with local anesthetic is performed with a 30-gauge, 2-cm needle at the previously marked bilateral sites (Fig. 48-5). Local anesthetic infiltration is continued subcutaneously with a 22-gauge, 5- to 9-cm needle along the eventual caudomedial oblique needle path. The fluoroscopic beam is directed along the projected needle path to simplify needle insertion. The needle is then directed under fluoroscopic guidance to reach a point immediately anterior to the L5-S1 vertebral junction; the fluoroscopic beam is directed to minimize the needle hub’s radiographic size. If the fluoroscopic beam is directed properly, this approach should guide the needle tip to the correct position. The iliac crest and the L5 transverse process may obstruct passage of the needle; if this is the case, the needle is withdrawn and redirected in a cephalad or caudad angle to bypass the obstruction. As in the approach taken with either the celiac or lumbar sympathetic block, if the needle tip contacts the body of the vertebra (in this case, L5), the needle is simply redirected to “walk off” the body to its desired position immediately anterior to the L5-S1 junction (the sacral prominence).
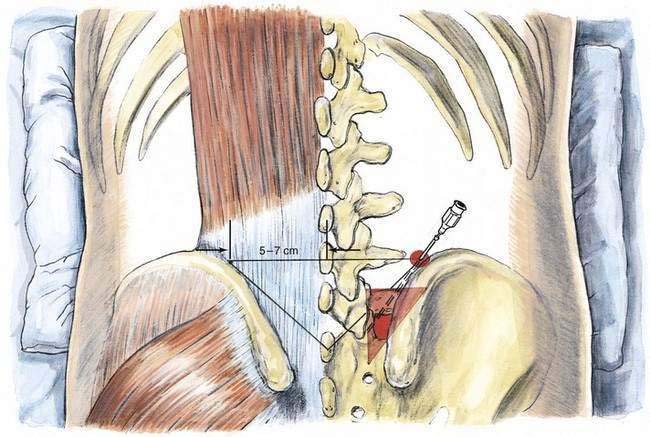
Figure 48-4. Surface anatomy and skin markings important for superior hypogastric plexus block: posteroanterior view.
Potential Problems
Owing to the proximity of the iliac vessels (arteries and veins) to the needle paths, care should be taken to minimize the potential for intravascular injection (Fig. 48-6). This anatomic relationship also makes hematoma formation possible. If the position of the needle tip is not accurately verified, both intramuscular and intraperitoneal injection are possible. Even when the needle is inserted correctly, paraspinous muscle spasm may result from needle-induced paraspinous muscle irritation. This usually lasts only a few days. Less frequent problems are lumbar or sacral somatic nerve injury and renal or ureteral puncture. It is advisable to caution the patient about the potential for bowel or bladder habit changes as well as decreases in sexual function after the neurolytic superior hypogastric plexus block, despite the rarity of these side effects.