134 Submersion Injuries
• Drowning is the second leading cause of death in children.
• Inadequate supervision is the main risk factor for drowning in children.
• Some patients with relatively mild symptoms initially can deteriorate.
• Cardiopulmonary resuscitation at the scene is the most important factor in improving survival.
• Most drowning victims should be transferred to the emergency department regardless of the initial appearance at the scene.
• The degree of hypoxia determines the outcome.
• Cervical spine immobilization is unnecessary unless trauma is suspected.
• Asymptomatic patients should be observed for at least 4 to 6 hours before being discharged.
Epidemiology
Submersion simply means going under water. To avoid confusion, especially in reporting, the International Liaison Committee on Resuscitation recommends that the following previously used terms no longer be used: dry and wet drowning, active and passive drowning, silent drowning, secondary drowning, and drowned versus near-drowned.1 In 2002, the World Congress on Drowning adopted a uniform definition of drowning: “the process resulting in primary respiratory impairment from submersion/immersion in a liquid medium.”2
Drowning is an important cause of childhood morbidity and is among the top 10 causes of mortality (Fig. 134.1). Drowning is estimated to kill 500,000 people every year worldwide. Eighty percent of these episodes take place in low-income countries and low-income groups. About 80% of drowning episodes are deemed preventable.3,4
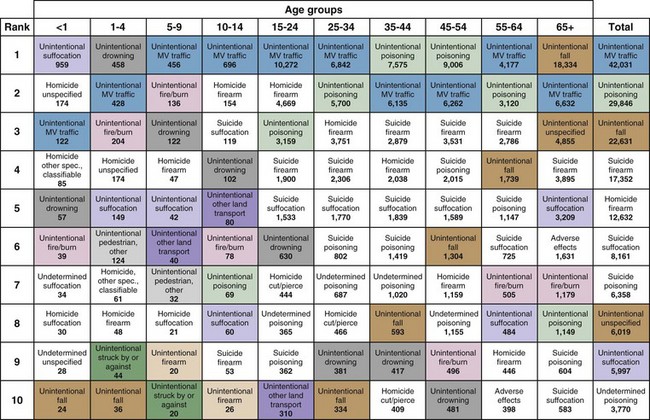
(Adapted from National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System [database]. Available at http://www.cdc.gov/ncipc/wisgars/.)
Overall rates of drowning have dropped in all age groups, probably as a result of improved awareness, use of preventive measures, and other factors (Box 134.1). Inadequate supervision is the main risk factor for drowning in children. Most toddlers who drown do so in their own home pools, most infants drown in bathtubs, and adults and older children drown in fresh water. Fencing of private pools reduces the risk for drowning.5
Pathophysiology
Injuries from drowning result mainly from asphyxia and subsequent hypoxic-ischemic damage to vital organs. The event starts with panic because of air hunger and, eventually, aspiration of fluid into the hypopharynx. Reflex laryngospasm occurs but is usually brief before the victim aspirates large amounts of fluid into the lungs. Further aspiration can occur if the victim vomits and aspirates gastric contents. Aspiration is the end result of all drowning, and the old terminology of dry and wet drowning should not be used.6,7 Changes in intravascular volume, hematocrit, and electrolyte concentration as a result of aspiration are usually mild and not clinically significant. Both salt water and fresh water cause lung injury. The effect of tonicity on the intravascular compartment is minimal.8,9
Prognostic Factors
At the Scene
Performance of cardiopulmonary resuscitation (CPR) at the scene has been documented to improve survival in some cases, especially after cold water submersion. Generally, hypothermia is a poor prognostic sign unless the victim has fallen into extremely cold water (<10° C) or has undergone rapid cooling. Several case reports of survival of victims in such circumstances were attributed to a protective effect of cooling on the brain, which has led some authorities to recommend continuing CPR in hypothermic victims while actively rewarming them before declaring them dead.10
Treatment
Prehospital Management
CPR at the scene is the most important initial step. It can be started even if the victim is still in the water. After the airway is secured and oxygenation and ventilation are ensured, the patient should be transferred to the nearest hospital. Further management at the scene depends on the availability of personnel experienced in advanced life support (Fig. 134.2). Most drowning victims should be transferred to an emergency department (ED) regardless of the initial appearance at the scene. Exceptions are those with obvious rigor mortis, lividity, and decay.
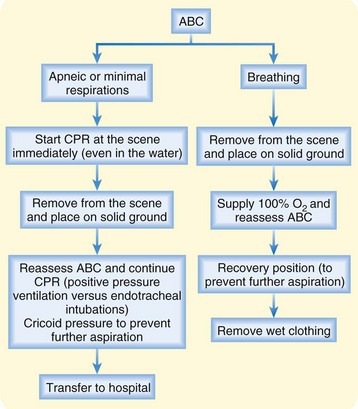
Fig. 134.2 Algorithm for prehospital treatment of drowning victims.
ABC, Airway, breathing, and circulation (ABCs of resuscitation); CPR, cardiopulmonary resuscitation.
Emergency personnel dealing with a drowning victim should avoid the following:
Emergency Department Management
The main aims of treatment of a drowning victim in the ED are to avoid further hypoxia and restore effective ventilation and circulation (Table 134.1). ED personnel should assume the triad of hypoxia, acidosis, and hypothermia to be present in every drowning victim until proved otherwise. The need for cervical spine immobilization should be assessed, but in atraumatic drowning, immobilization is not mandatory. Vomiting occurs frequently, so early airway protection should be considered in distressed patients.
Table 134.1 Summary of Emergency Department Management of Drowning
| ASPECT | INTERVENTION |
|---|---|
| Airway |
Airway
• For breathing patients, the FIO2 value should be kept at 1.0.
• For patients in respiratory distress, emergency personnel should have a low threshold for intubation. Treatment may start with positive pressure and positive end-expiratory pressure (PEEP) ventilation with a nasal cannula or mask.
• Indications for intubation are as follows: unconsciousness, respiratory insufficiency, and high O2 requirements to keep the oxygen saturation value higher than 90% or PO2 higher than 60 to 90 mm Hg (or both).
Circulation
• Vascular access, either intravenous or intraosseous, should be established.
• Arrhythmia, which can be the inciting event or a complication of hypoxia and hypothermia, should be ruled out.
• Fluid and electrolyte management and inotropic support are important to reverse depressed myocardial function, shock, and acidosis.
Management of Hypothermia
For a detailed discussion of hypothermia, refer to Chapter 131. Hypothermia is defined as a core body temperature lower than 35° C. Depending on the temperature, hypothermia may be mild, moderate, or severe. This condition should be anticipated and treated in drowning victims. Notably, standard thermometers may not accurately measure low temperatures. Rewarming techniques are discussed in Chapter 131.
Next Steps in Care and Patient Education
Some reports suggest that therapeutic hypothermia can improve neurologic outcome after out-of-hospital cardiac arrest and therefore recommend induction of hypothermia in drowning victims after restoration of spontaneous circulation as a neuroprotective therapy. Further studies of this approach are needed, especially regarding its use in children.11,12
![]() Documentation
Documentation
Prehospital
Patient demographics (e.g., age, sex)
Description of the accident (rule out trauma, abuse, suicide)
Nature of the fluid (e.g., temperature, level of cleanliness)
If the drowning is witnessed, estimated duration of submersion
Initial cardiorespiratory status
![]() Patient Teaching Tips
Patient Teaching Tips
Prevention of Drowning
Using personal flotation devices
Minimizing alcohol and substance abuse at beaches and around water
Counseling new parents about the importance of supervision, as well as the safety of bathtubs, buckets, and other vessels
Educating parents about safe bathing of babies: a child can drown in just a few inches of water
Recommending cardiopulmonary resuscitation courses for the public
Recommending swimming lessons with adult supervision
Identifying risk factors to help prevent a second incident if the victim survived
Bierens JJ, ed. Handbook on drowning: prevention, rescue, treatment. Amsterdam: Springer, 2004.
Bierens JJ, Knape JT, Gelissen HP. Drowning. Curr Opin Crit Care. 2002;8:578–586.
Ibsen L, Koch T. Submersion and asphyxial injury. Crit Care Med. 2002;11(Suppl):S402–S408.
National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (database). Available at http://www.cdc.gov/ncipc/wisqars/.
Olshaker J. Submersion. Emerg Med Clin North Am. 2004;22:357–367. viii
Zuckerbraun N, Saladino R. Pediatric drowning: current management strategies for immediate care. Clin Pediatr Emerg Med. 2005;6:49–56.
1 Idris AH, Berg RA, Bierens J, et al. Recommended guidelines for uniform reporting of data from drowning: the “Utstein style.”. Resuscitation. 2003;59:45–57.
2 Bierens JJ, ed. Handbook on drowning: prevention, rescue, treatment. Amsterdam: Springer, 2004.
3 National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (database). Available at http://www.cdc.gov/ncipc/wisqars/
4 Zuckerbraun N, Saladino R. Pediatric drowning: current management strategies for immediate care. Clin Pediatr Emerg Med. 2005;6:49–56.
5 Brenner RA, Trumble AC, Smith GS, et al. Where children drown, United States, 1995. Pediatrics. 2001;108:85–89.
6 Modell JH, Bellefleur M, Davis JH. Drowning without aspiration: is this an appropriate diagnosis? J Forensic Sci. 1999;44:1119–1123.
7 Olshaker J. Submersion. Emerg Med Clin North Am. 2004;22:357–367. viii
8 Bierens JJ, Knape JT, Gelissen HP. Drowning. Curr Opin Crit Care. 2002;8:578–586.
9 Ibsen L, Koch T. Submersion and asphyxial injury. Crit Care Med. 2002;11(Suppl):S402–S408.
10 Modell J, Idris A, Pineda J, et al. Survival after prolonged submersion in freshwater in Florida. Chest. 2004;125:1948–1951.
11 Nolan JP, Soar J. Mild therapeutic hypothermia after cardiac arrest: keep chilling. Crit Care Med. 2011;39:206–207.
12 Nolan JP, Morley PT, Vanden Hoek TL, et al. Therapeutic hypothermia after cardiac arrest. An advisory statement by the Advancement Life support Task Force of the International Liaison committee on Resuscitation. Resuscitation. 2003;57:231–235.


