Chapter 93 Subaxial Cervical Deformities
A deformity of the cervical spine may result from a variety of etiologies, including trauma, degenerative disease, congenital anomaly, infection, tumor, muscle denervation and neuromuscular disease,1 as well as iatrogenic causes such as surgery and irradiation. Cervical deformities may also occur in patients with systemic arthritides such as ankylosing spondylitis and rheumatoid arthritis.2 Likewise, patients with primary neurologic disorders such as athetoid cerebral palsy, spasmodic torticollis, and other movement disorders, as well as patients with neuromuscular disorders, are predisposed to develop cervical deformity due to degeneration. Patients with bone disorders such as osteogenesis imperfecta and spondyloepiphyseal dysplasia may also develop deformity involving the cervical region. Patients often present with complaints of neck pain, myelopathy, radiculopathy, or neck deformity with loss of mobility.
Subaxial cervical deformities most commonly occur in the sagittal plane, primarily as kyphosis, although hyperlordosis or a mixed swan-neck deformity can also be observed. Deformity in the coronal plane, manifesting as a scoliosis or angulation, is uncommon in the cervical region when compared with the thoracic and lumbar regions.3 Most cervical coronal deformities are the result of congenital vertebral anomalies.
Significance of Cervical Kyphosis
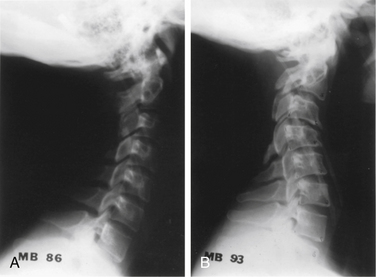
A considerable variation in the degree of cervical lordosis can be observed in the average patient population. Degenerative changes associated with aging typically produce a straightening of the spine, but the limits of normality are not established.4 After examining a group of asymptomatic patients, Gore et al. concluded that the normal cervical spine has a lordotic curve measuring approximately 15 to 20 degrees from C1 to T1.5 Generally, cervical kyphosis is defined as a ventral or kyphotic angulation of 5 degrees or more. The incidence of straightening or kyphosis increases with age for two reasons: (1) the cervical discs contribute to the normal lordotic curve, and (2) the loss of disc height and formation of osteophytes associated with degenerative changes produce a straightening of the spine. In some patients, increases in thoracic kyphosis associated with aging may produce a compensatory increase in cervical lordosis. Load transmission in the cervical spine is thought to be mostly in the posterior column; loss of sagittal alignment may occur if this axis is shifted ventrally.
After performing cadaver studies, Breig first called attention to the motion and degree of elongation of the spinal cord that occur during flexion and extension movements of the cervical spine.6 According to his measurements, there may be as much as a 45- to a 75-mm change in length of the spinal cord as a result of flexion and extension. Furthermore, there is relative motion of the cord in relation to the underlying vertebrae. Flexion movements produce tensile forces within the cord and elongation, whereas extension causes shortening or compression of the cord. Flexion also produces a decrease in the anteroposterior dimension of the spinal cord, but because of straightening of the dura and ligamenta flava, the available canal diameter is actually increased. Extension has the opposite effect. Changes in the normal configuration of the spinal canal caused by osteophyte formation, disc changes, or facet hypertrophy have the potential to compress or stretch the cord. Instability that results from ligamentous laxity, particularly when associated with a short, angular kyphotic segment, has an increased likelihood of inducing trauma to the spinal cord or adjacent nerve roots. The vascular supply could be decreased, leading to ischemia, which could in turn lead to neuronal loss and myelomalacia. Frequently, examination of the spinal cord in the axial projection demonstrates flattening that is most marked at the kyphotic segment. The potential for neurologic deficit arising from kyphosis without actual compression is small but certainly not nonexistent.
The degree to which these dynamic changes are clinically manifest is difficult to determine. Current imaging studies are performed with the patient recumbent and with the cervical spine in a neutral or slightly extended position, and the images produced are static. Although flexion-extension MRI has been advocated, especially to evaluate craniocervical junction instability, it has yet to receive widespread clinical use.
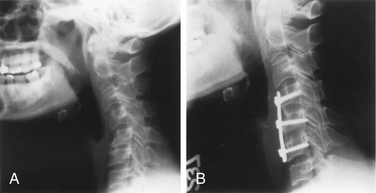
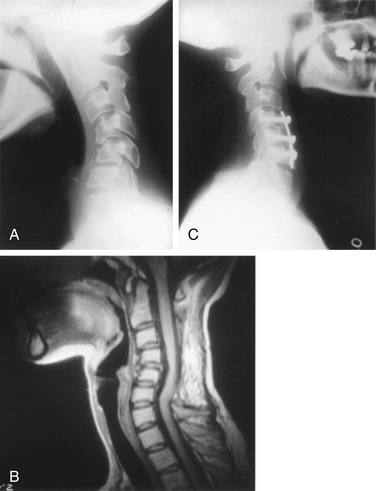
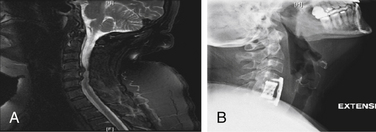
The significance of cervical kyphosis in the production of chronic muscle fatigue and dorsal neck pain is unclear. Although many patients demonstrate reversal of normal cervical lordosis on plain radiographs, a very small number actually have refractory neck pain as a result of the deformity per se. Nonetheless, an occasional patient appears to have pain on this basis and requires careful evaluation and consideration for deformity correction and fusion (Fig. 93-1).
Postlaminectomy Kyphosis
Kyphosis is a well-recognized complication of laminectomy of the cervical spine.7–15 The detachment of the dorsal paraspinous muscles, removal of the dorsal osseoligamentous complex, and occasional disruption of the facet complexes have all been recognized as potential causes of the development of a kyphotic deformity after laminectomy.16
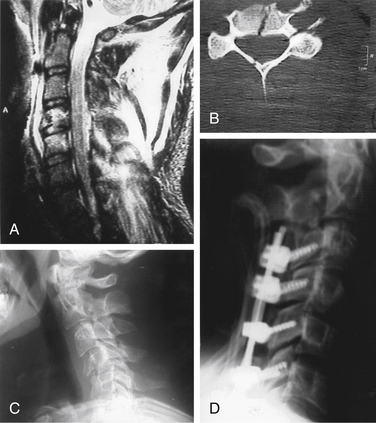
The reported incidence of kyphosis after cervical laminectomy has been quite variable, although it is considerably more common in the pediatric group. The incidence of postlaminectomy kyphosis in series of pediatric patients ranges from 33% to 100%. Many of these patients, however, have other factors that predispose them to spinal deformity, such as bony tumors, neurofibromatosis, or irradiation. A recent series, which excluded these confounding factors, noted an incidence of kyphotic deformity of 53% in children.7 Although the data are mixed, it appears that a younger age and a greater number of segments treated with laminectomy are associated with higher rates of deformity. Injury or resection of the facet joints also increases the probability of kyphosis. Laminectomy of C1 has a relatively low tendency to result in spinal deformity. Although it has not been conclusively demonstrated that the performance of laminoplasty, as recommended by Raimondi et al.,17 reduces the likelihood of postlaminectomy kyphosis in children, many neurosurgeons who routinely perform cervical procedures on children perform laminoplasty, and some report evidence suggestive of benefit.18 Prophylactic fusion should also be considered for patients undergoing laminectomy who are at high risk for developing kyphosis.15 Dorsal fusions are much more effective at preventing kyphosis than at correcting it (Fig. 93-2).
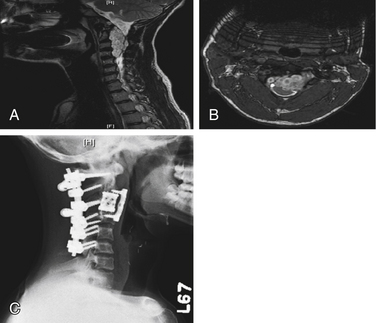
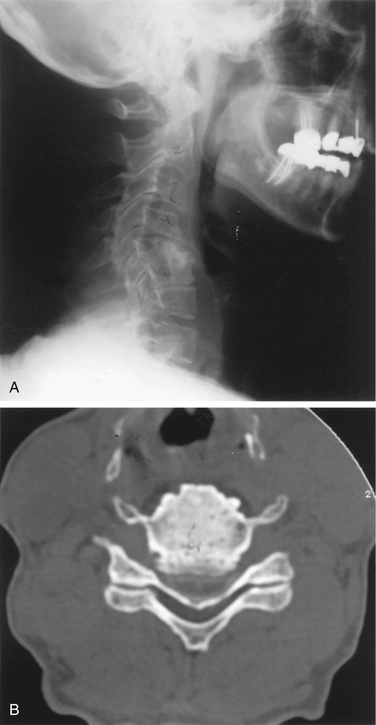
The incidence of postlaminectomy kyphosis in adults is relatively uncommon in the absence of an additional predisposing factor such as facet joint damage, prior ligamentous instability, ventral column compromise, neurologic deficit, or irradiation.19,20 Adult cases are, nonetheless, seen in any busy practice specializing in spinal problems (Fig. 93-3). A recognition of the significance of this finding in terms of the probability of progression, the potential for symptoms, and the appropriate therapeutic options is essential for optimal management. Patients with the greatest risk of postlaminectomy kyphosis are those that have preoperative instability as well as those with straightening of the cervical spine. Additional risk factors include multilevel laminectomy, extensive facetectomy, and resection of the musculature at C2. Iizuka noted that removal of the semispinalis cervicis muscle attachment at C2 could lead to loss of alignment and kyphosis.21
Surgical Correction of Cervical Kyphosis
Preoperative Assessment
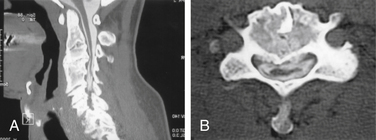
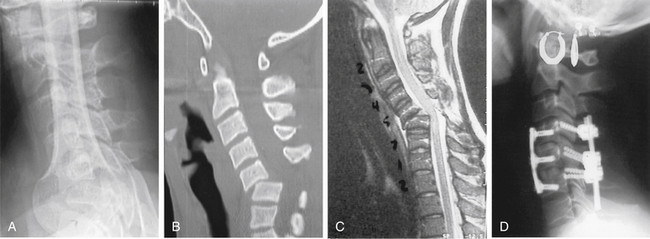
The preoperative evaluation of all such patients should include a careful neurologic assessment to look for subtle signs of myelopathy or radicular involvement. Plain cervical spine radiographs with flexion-extension views provide information about the deformity, including the levels involved, the severity, and whether it appears fixed or rigid. Neuroradiologic imaging with MRI or myelography and postmyelographic CT is important for evaluating spinal cord compression and the dimensions of the spinal canal. Assessment of the bony and ligamentous anatomy is also possible with these studies. Three-dimensional reconstructive CT has also been useful in assessing kyphosis, because bony detail, amount of deformity, and spinal canal encroachment can be visualized on one image (Fig. 93-4). The degree of spinal instability can also be assessed. Standing long-cassette films are helpful for evaluating overall sagittal spinal balance in patients with severe deformity. Concomitant thoracic kyphosis or fixed flexion contracture of the hip must be evaluated before consideration is given to “lordosing” a cervical kyphosis.
Surgical Techniques
Ventral Surgery
A ventral approach is preferred for cases in which there is insufficient anterior column height or insufficient ability to bear an axial load, such as with collapse of a ventral bone graft or compression fracture, with ventral pathology such as tumor or associated spondylotic bars producing myelopathy, or with a deformity that is rigid or incompletely reducible. Anterior surgery may also be indicated for focal areas of deformity. In addition, ventral surgery may be safer for the treatment of postlaminectomy kyphosis because surgery can be performed through an unoperated field (Fig. 93-5). The ventral approach has other advantages, including the ability to decompress the spinal cord ventrally and to use ventral interbody strut grafts that are loaded in compression, thereby enhancing fusion.22
In these cases, a ventral release, with or without ventral decompression of the spinal canal, is performed. If appropriate, the kyphotic deformity is then reversed, with reestablishment of some lordotic curve. Reversal of kyphosis should not be attempted in the face of significant radiologic evidence of spinal cord impingement unless surgical decompression is first performed (Fig. 93-6). As noted previously, extension of the cervical spine decreases the anteroposterior dimension of the spinal canal while increasing the thickness of the spinal cord. With a severe, rigid angular kyphotic deformity, dorsal decompression by means of laminectomy and foraminotomy should be considered before ventral osteotomy.
The surgical techniques for ventral decompression and fusion of deformity are quite similar to those used in the treatment of trauma or degenerative disease. Fiberoptic nasotracheal intubation is preferred to allow dental occlusion and maximal proximal exposure that is unimpeded by the mandible. The patient is positioned supine in traction with as much extension as is possible, as determined preoperatively. This may be facilitated by a roll placed dorsally in the cervical region. In cases in which spinal cord compression is observed, methylprednisolone as a 30-mg/kg IV bolus over 15 minutes followed by 5.4 mg/kg per hour continuous IV infusion can be given, although this is a controversial issue. If the patient awakens neurologically intact, the infusion is stopped. Otherwise, the infusion is continued for 23 hours. Prophylactic antibiotics are administered. When bicortical ventral fixation plates are used, C-arm fluoroscopy is routine. Plain radiography or fluoroscopy is also invaluable for assessing the degree of reduction and for graft placement. An intraoperative radiograph is performed at this time to assess spinal alignment. Significant deformity reduction is often evident following the placement of tong traction and general anesthesia. If autologous bone graft is to be used, the donor site and cervical region are prepared simultaneously. The incision is centered at the middle of the deformity to be treated. A transverse incision placed in a skin crease is preferred for short (one to three) segment fusions or in people with short, thick necks. An incision along the ventral margin of the sternocleidomastoid muscle is used for longer fusions. Exposure of the ventral aspect of the spine is accomplished as described by Cloward23 and Smith and Robinson.24
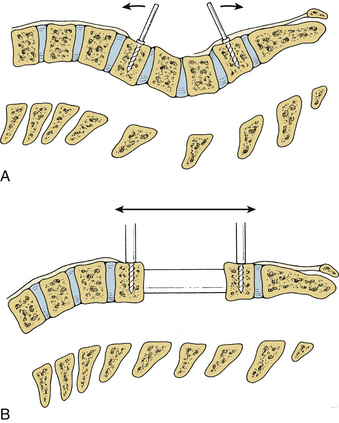
Dissection of the medial attachments of the longus colli muscles and placement of self-retaining retractors is followed by incision of the anulus fibrosus at the affected disc levels. The Caspar vertebral body distractor (Aesculap, San Francisco, CA) that uses screw posts placed into the vertebral bodies is a useful aid for reducing the kyphosis and placing ventral strut grafts (Fig. 93-7). Excess intervertebral traction, however, may be injurious to the compromised spinal cord and thus should be used judiciously. The distraction posts are placed parallel to the vertebral end plates. After osteotomy or ventral release of anular attachments, the posts are used to effect reduction by positioning them in a parallel configuration. This maneuver realigns the spine and allows application of the retractor.25 The retractor then maintains the reduction and allows further distraction force to be applied. After a bone graft is inserted, the retractor is removed and a plate is applied. This technique should not be used if there is evidence of dorsal compression by laminae, ligaments, or other pathology.
The decompression is tailored according to the results of preoperative imaging. In some cases, multilevel discectomy with multiple interbody bone grafts is preferred. This is useful for kyphotic deformities extending over several motion segments. Plate fixation can then be segmental to provide greater rigidity. Alternatively, when there is a bony encroachment on the canal, trough corpectomy with strut grafting is performed. A strut graft spanning two disc spaces with an additional ventral interbody graft at the level above or below can also be used when required (Fig. 93-8). Alternatively, the cancellous bone obtained from the decompression can be morselized and placed in a cage, allowing anterior column reconstruction with the associated morbidity of iliac crest grafting or the small risks associated with allograft (Fig. 93-9). This type of mixed construct provides the maximum number of sites for screw placement and allows for greater fixation and optimal reestablishment of lordosis. If two or more vertebral bodies are replaced, consideration should be given to adding dorsal fixation.26
Locking and nonlocking plates and slotted plates are used. For multisegment constructs, the latter system often provides more flexibility and is easier to apply. The variability in screw angulation allowed by the Caspar plate is helpful when plates are extended to C2 or C3. Fluoroscopy can be an aid to kyphosis reduction and plate application regardless of which system is used. Fluoroscopic control is highly desirable when screws are placed into the dorsal vertebral body cortex. Steinmetz et al. recently reported a series of 14 patients treated ventrally for postsurgical kyphosis. They used intraoperative neck extension, as well as a dynamic, ventrally placed implant with multiple fixation points, to restore lordosis. They corrected 11 of 12 patients with this method (average 20-degree correction) with minimal complications.27
In most cases, postoperative immobilization is achieved with a rigid cervical collar that is worn for 6 weeks to 3 months. A halo vest or Minerva jacket may be used in cases in which fixation is suboptimal or when fusion is expected to be delayed. Patients with severe osteoporosis, high-grade instability noted preoperatively, or failed prior attempts at fusion perhaps should be included in this group. Herman and Sonntag also noted the occasional need for halo immobilization in some high-risk patients after this type of procedure.28
Complications
The potential complications associated with the ventral approaches are well known and include vocal cord palsy, hoarseness or dysphagia, injury to visceral structures (such as the esophagus or trachea), graft displacement, screw loosening or fracture, wound complications (such as infection), hematoma (which may be sufficient to cause respiratory embarrassment), and dehiscence.29 The incidence of a number of complications can be reduced by periodically releasing or removing the retraction during the operation. Also, for procedures involving the lower cervical spine, a left-sided approach may reduce the likelihood of vocal cord paralysis in the event that there is a nonrecurrent right inferior laryngeal nerve.
Dorsal Fixation and Fusion Techniques
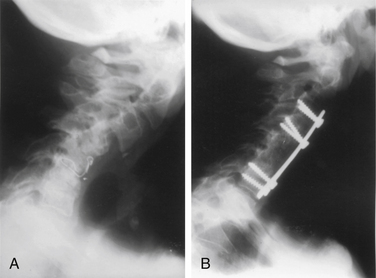
Dorsal fusion for cervical kyphotic deformity is primarily indicated as a prophylactic measure after laminectomy or when the deformity is the result of dorsal ligamentous insufficiency associated with the preservation of axial integrity of the anterior column, such as is seen acutely after ligamentous trauma (Fig. 93-10). Posterior surgery is also indicated in patients requiring a posterior osteotomy, as in cases of ankylosing spondylitis. In these cases, usually performed at the cervicothoracic junction, the C7 lamina and pedicles are removed.30 In these cases, the kyphosis usually significantly or completely reduces with neck extension. Dorsal fusion is accomplished via standard techniques, including interspinous wiring or lateral mass wire or plate fixation. Abumi et al.31 recently reported a series of patients with cervical kyphosis who underwent placement of cervical pedicle screws to maintain correction. Dorsal surgical approaches for rigid or incompletely reducible kyphotic deformities have limited application and are biomechanically less sound. Nevertheless, certain circumstances may warrant their use as the sole operative treatment, especially if fusion in situ is being performed. More often, dorsal fusions are performed in conjunction with a dorsal decompression and ventral procedures when treating severe deformity associated with spinal cord compression.11,32
Postlaminectomy kyphosis is corrected less well by dorsal fixation and fusion than by ventral techniques. If this approach is to be used, lateral mass plates or interfacet wiring, combined with iliac strips or rib grafts, are used. In the early 1990s, lateral mass fixation became the preferred fixation method because it provided greater rigidity than wire fixation.33 Complications associated with screw placement are uncommon if meticulous care is used to select screw entry points and the screws are angled appropriately rostrally and laterally to avoid the nerve root and vertebral artery. However, it must be cautioned that a deformity or prior surgery may obscure the anatomic landmarks so that great care is required for satisfactory screw placement. Frameless stereotaxy may be used in patients with previous surgery where standard landmarks may be lost. Bicortical purchase does not appear to be necessary for successful fixation in most cases. Fehlings et al. obtained successful fusion results using lateral mass plates without additional bone graft.33 This study, however, was heavily weighted with posttraumatic cases, so careful consideration should be given to the use of autologous bone graft in deformity cases. Patients with cervical spine trauma and injury to the posterior ligamentous complex may also benefit from a posterior cervical procedure. Injury reduction can occur with the use of traction or in the operating room. The facets may need to be drilled off to achieve reduction. Lateral mass or pedicle screw fixation may be used to achieve fixation and fusion, and these constructs have been found to be biomechanically superior to ventral procedures.34
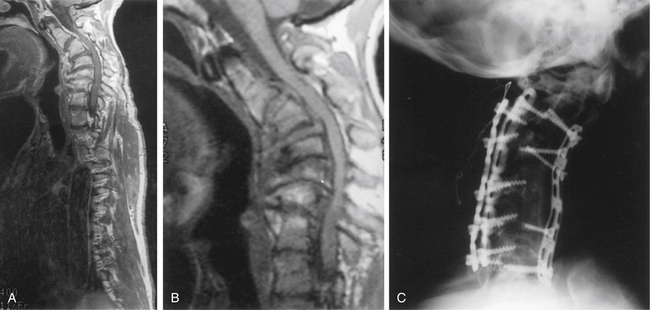
Combined Ventral and Dorsal Decompression and Fusion
Combined procedures involving both an anterior and a posterior approach are occasionally indicated, especially for the correction of rigid deformities (Fig. 93-11). Other indications include cases of both anterior and posterior compression with radiculopathy secondary to foraminal stenosis as a prominent feature, cases in which severe slippage is associated with incompetent posterior ligamentous structures, and cases of trauma when there is compromise of the anterior and posterior columns (Fig. 93-12). Mummaneni et al. had good results in a series of 30 patients who underwent circumferential fusion for a variety of etiologies causing multilevel cervical kyphosis, including fractures, tumors, and degenerative disease.35
Patients with ankylosing spondylitis may present with a severe, rigid cervical kyphosis that limits the ability to look forward, and in some severe cases, this kyphosis may limit jaw opening secondary to contact with the chest. Correction of this type of deformity requires osteotomy with resection of a portion of the posterior elements. Different methods have been described for this procedure,36–38 the most notable being the one advocated by Simmons,30,38 in which a posterior decompression is performed under local anesthesia at the C7-T1 level, with the patient in the seated position. The spine is fractured by forcibly extending the neck, which is held in traction by a halo ring. Usually, the fracture in these patients occurs at the junction between the vertebral end plate and the disc. Simmons advocates that the procedure be performed with the patient awake to provide for patient feedback during kyphosis reduction. Other surgeons have performed the procedure using a general anesthetic and have monitored evoked potentials.
Arnold P.M., Bryniarski M., McMahon J. Posterior stabilization of subaxial cervical spine trauma: indications and techniques. Injury. 2005;36:S36-S43.
Deutsch H., Haid R.W., Rodts G.E., et al. Postlaminectomy cervical deformity. Neurosurg Focus. 2003;15:1-5.
Fassett D.R., Clark R., Brockmeyer D.L., et al. Cervical spine deformity associated with resection of spinal cord tumors. Neurosurg Focus. 2006;20:1-7.
Hoh D.J., Khoueir P., Wang M.Y. Management of cervical deformity in ankylosing spondylitis. Neurosurg Focus. 2008;24:1-10.
Kaptain G.J., Simmons N., Replogle R.E., et al. Incidence and outcome of kyphotic deformity following laminectomy for cervical spondylotic myelopathy. J Neurosurg Spine. 2000;93:199-204.
Mummaneni P.V., Dhall S.S., Rodts G.E., et al. Circumferential fusion for cervical kyphotic deformity. J Neurosurg Spine. 2008;9:515-521.
Simmons E.D., DiStefano R.J., Zheng Y., et al. Thirty-six years experience of cervical extension osteotomy in ankylosing spondylitis: techniques and outcomes. Spine (Phila Pa 1976). 2006;31:3006-3012.
Steinmetz M.P., Kager C.D., Benzel E.C. Ventral correction of postsurgical cervical kyphosis. J Neurosurg Spine. 2003;98:1-7.
Stewart T.J., Steinmetz M.P., Benzel E.C. Techniques for the ventral correction of postsurgical cervical kyphotic deformity. Neurosurgery. 2005;56(1):191-195.
1. Fassett D.R., Clark R., Brockmeyer D.L., et al. Cervical spine deformity associated with resection of spinal cord tumors. Neurosurg Focus. 2006;20:1-7.
2. Hoh D.J., Khoueir P., Wang M.Y. Management of cervical deformity in ankylosing spondylitis. Neurosurg Focus. 2008;24:1-10.
3. Smith M.D. Congenital scoliosis of the cervical or cervicothoracic spine. Orthop Clin North Am. 1994;25:301-310.
4. Gay R.E. The curve of the cervical spine: variations and significance. J Manip Physiol Ther. 1993;16:591-594.
5. Gore D.R., Sepic S.B., Gardner G.M. Roentgenographic findings of the cervical spine in asymptomatic people. Spine (Phila Pa 1976). 1986;11:521-524.
6. Breig A. Biomechanics of the central nervous system. Stockholm: Almquist and Wiskell; 1960.
7. Bell D.F., Walker J.L., O’Connor G., et al. Spinal deformity after multiple-level laminectomy in children. Spine (Phila Pa 1976). 1994;19:406-411.
8. Butler J.C., Whitecloud T.S. Postlaminectomy kyphosis: causes and surgical management. Orthop Clin North Am. 1992;23:505-511.
9. Callahan R.A., Johnson R.M., Margolis R.N., et al. Cervical facet fusion for the control of instability following laminectomy. J Bone Joint Surg [Am]. 1977;59:991-1002.
10. Cattell H.S., Clark G.L.Jr. Cervical kyphosis and instability following multiple laminectomies in children. J Bone Joint Surg [Am]. 1967;59:991-1002.
11. Kaptain G.J., Simmons N., Replogle R.E., et al. Incidence and outcome of kyphotic deformity following laminectomy for cervical spondylotic myelopathy. J Neurosurg Spine (Phila Pa 1976). 2000;93:199-204.
12. Katsumi Y., Honma T., Nakamura T. Analysis of cervical instability resulting from laminectomy for removal of spinal tumor. Spine (Phila Pa 1976). 1989;14:1172-1176.
13. Mikawa Y., Shikata J., Yamamuro T. Spinal deformity and instability after multilevel cervical laminectomy. Spine (Phila Pa 1976). 1987;12:6-11.
14. Sim F.H., Svien H.J., Bickel W.H., Janes J.M. Swan neck deformity following extensive cervical laminectomy: a review of twenty-one cases. J Bone Joint Surg [Am]. 1974;56:564-580.
15. Yasuoka S., Peterson H.A., Laws E.R., et al. Pathogenesis and prophylaxis of postlaminectomy deformity of the spine after multiple level laminectomy: difference between children and adults. Neurosurgery. 1981;9:145-152.
16. Saito T., Yammamuro T., Shikata J., et al. Analysis and prevention of spinal column deformity following cervical laminectomy. I. Pathogenetic analysis of postlaminectomy deformities. Spine (Phila Pa 1976). 1991;16:494-502.
17. Raimondi A.J., Gutierrez F.A., Di Rocco C. Laminotomy and total reconstruction of the posterior spinal arch for spinal canal surgery in childhood. J Neurosurg. 1976;45:555-560.
18. Abbott R., Feldstein N., Wisoff J.H., et al. Osteoplastic laminotomy in children. Pediatr Neurosurg. 1992;18:153-156.
19. Zdeblick T.A., Zou D., Warden K.E., et al. Cervical stability after foraminotomy. A biomechanical in vitro analysis. J Bone Joint Surg [Am]. 1992;74:22-27.
20. Zdeblick T.A., Abitbol J.J., Kunz D.N., et al. Cervical stability after sequential capsule resection. Spine (Phila Pa 1976). 1993;18:2005-2008.
21. Iizuka H., Shimizu T., Tateno K., et al. Extensor musculature of the cervical spine after laminoplasty: morphologic evaluation by coronal view of the magnetic resonance image. Spine (Phila Pa 1976). 2001;26:2220-2226.
22. Zdeblick T.A., Bohlman H.H. Cervical kyphosis and myelopathy. J Bone Joint Surg [Am]. 1989;71:170-182.
23. Cloward R.B. The anterior approach for removal of ruptured cervical discs. J Neurosurg. 1958;15:602-617.
24. Robinson R.A., Smith G.W. Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. Bull Johns Hopkins Hosp. 1955;96:223-224.
25. Stewart T.J., Steinmetz M.P., Benzel E.C. Techniques for the ventral correction of postsurgical cervical kyphotic deformity. Neurosurgery. 2005;56(1):191-195.
26. Deutsch H., Haid R.W., Rodts G.E., et al. Postlaminectomy cervical deformity. Neurosurg Focus. 2003;15:1-5.
27. Steinmetz M.P., Kager C.D., Benzel E.C. Ventral correction of postsurgical cervical kyphosis. J Neurosurg Spine. 2003;98:1-7.
28. Herman J.M., Sonntag V.K.H. Cervical corpectomy and plate fixation for postlaminectomy kyphosis. J Neurosurg. 1994;80:963-970.
29. Heller J.G., Silcox D.H.III, Sutterlin C.E. Complications of posterior plating. Spine (Phila Pa 1976). 1995;20:2442-2448.
30. Simmons E.D., DiStefano R.J., Zheng Y., et al. Thirty-six years experience of cervical extension osteotomy in ankylosing spondylitis: techniques and outcomes. Spine (Phila Pa 1976). 2006;31:3006-3012.
31. Abumi K., Shono Y., Taneichi H. Correction of cervical kyphosis using pedicle screw fixation systems. Spine (Phila Pa 1976). 1999;24:2389-2396.
32. Miyazaki K., Tada K., Matsuda Y., et al. Posterior extensive simultaneous multi-segment decompression with posterolateral fusion for cervical instability and kyphotic and/or S-shaped deformities. Spine (Phila Pa 1976). 1989;14:1159-1170.
33. Fehlings M.G., Cooper P.R., Errico T.J. Posterior plates in the management of cervical instability: long-term results in 44 patients. J Neurosurg. 1994;81:341-349.
34. Arnold P.M., Bryniarski M., McMahon J. Posterior stabilization of subaxial cervical spine trauma: indications and techniques. Injury. 2005;36:S36-S43.
35. Mummaneni P.V., Dhall S.S., Rodts G.E., et al. Circumferential fusion for cervical kyphotic deformity. J Neurosurg Spine. 2008;9:515-521.
36. Lin S.Y., Wu H.J., Chien S.H. Correction osteotomy of flexion deformity of cervical spine in ankylosing spondylitis, case report. Kaohsiung J Med Sci. 1990;6:454-460.
37. Savini R., DiSilvestre M., Gargiulo G. Cervical osteotomy by the Simmons method in the treatment of cervical kyphosis due to ankylosing spondylitis, case report. Ital J Orthop Traumatol. 1988;14:377-383.
38. Simmons E.H. The surgical correction of flexion deformity of the cervical spine in ankylosing spondylitis. Clin Orthop. 1972;86:132-143.