29 Subaxial Cervical and Upper Thoracic Spine Fractures in the Elderly
KEY POINTS
Introduction
Although atlantoaxial fractures are more common than subaxial fractures in the elderly, there is considerable morbidity associated with subaxial cervical and upper thoracic spine fractures. These more caudal spine injuries are more likely to be associated with neurological deficits, in comparison to atlantoaxial injuries, and more likely to be associated with higher-energy mechanisms.1
Apart from the nearly ubiquitous osteoarthritic spondylosis seen in geriatric patients, other etiologies of severe cervical and thoracic spine ankylosis can alter the biomechanics of the cervical spine, causing increased susceptibility to fracture from minor traumatic events. These include ankylosing spondylitis (AS) and diffuse idiopathic skeletal hyperostosis (DISH). Both conditions result in a stiff and often osteoporotic spine. With injury, both the anterior and posterior columns may be completely disrupted, causing frank instability. Fractures of the ankylosed spine are associated with 50% morbidity and 30% mortality.2 For this reason, a high level of suspicion is required not to overlook potentially unstable fracture patterns.
The treatment of subaxial cervical and upper thoracic spine fractures continues to be evaluated. The subaxial cervical spine injury classification system (SLIC) has been established to provide clinicians with standardization for making nonoperative versus operative decisions and, ultimately, how to surgically approach the injuries.3 The traditional thinking regarding the most optimal timing of surgical treatment of injuries is also changing. Specifically, there is now good evidence that early surgical treatment of central cord injuries is superior to late treatment for certain categories of patients. Geriatric surgical techniques are also evolving; the complex and overlapping pathologies of osteoporosis and ankylosis present challenges for which meticulous preoperative planning may prevent certain postoperative complications.
Basic Science
The radiographic and clinical evaluation of the cervical spine in the patient following trauma continues to be evaluated. There are ongoing modifications of recommendations regarding the role of radiographs, multiplanar CT, and MRI to rule out cervical spine injuries in the trauma patient. Multiplanar CT and MRI have been shown to have very high sensitivity for detecting cervical spine injury. Despite a high sensitivity, there are reports of cervical spine injury in obtunded patients with an unremarkable multiplanar CT.4 Brandenstein and colleagues recently reported on four patients with negative cervical CT scans and MRIs who later had evidence of cervical instability.5 They estimated that 0.2% to 0.4% of their patients would have cervical spine instability despite normal CT and MRI findings. Not surprisingly, three of the four patients with instability were geriatric. It is prudent to have a high degree of suspicion for cervical spine injuries in the geriatric patient despite seemingly normal imaging.
Ankylosing Spondylitis
Ankylosing spondylitis (AS) is a seronegative (RF-negative) spondyloarthropathy that predominantly affects the sacroiliac joints and spine. It typically, but not exclusively, affects HLA-B27–seropositive patients. The prevalence ranges from 0.1% in African and Eskimo populations to as high as 6% in Haida Native Americans in northern Canada. The white populations of the USA and UK have a prevalence of 0.5% to 1.0%. AS typically has its onset in the third decade of life, with a mean age of onset of 26. It rarely begins after the age of 40, although the diagnosis may be made at a later age because earlier symptoms are ignored or benign. A juvenile form of AS is described, but it does not affect the spine.
Clinical Case Examples
CASE 1
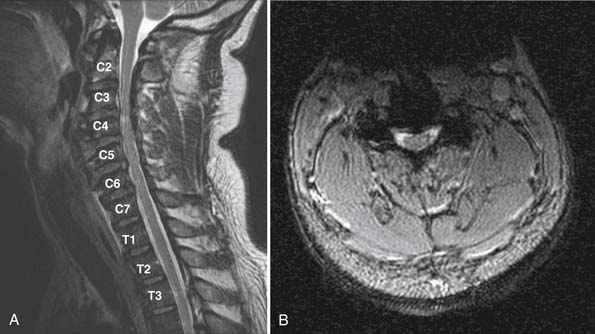
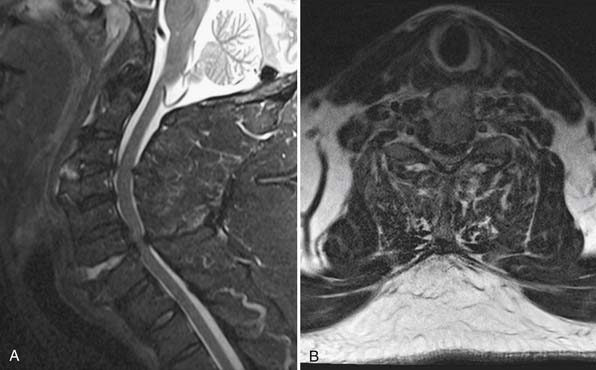
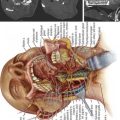
Imaging evaluation revealed extensive degenerative changes. Posterior osteophytes from C3 to C7 and calcification of the posterior longitudinal ligament were demonstrated on CT scanning. There was no fracture, malalignment, or prevertebral edema appreciated (Figure 29-1). An MRI revealed C3-4 disc osteophyte complex associated with spinal cord compression and T2 hyperintensity of the cord. Additional disc protrusions were seen at more caudal cervical levels (Figure 29-2).

FIGURE 29-1 Case 1: Midsagittal CT of cervical spine shows multilevel degenerative changes without evidence of fracture.
He was initially treated with cervical collar immobilization. His neurological examination was monitored. The patient showed no improvement in his neurological examination. The recommendation to decompress and stabilize the cervical spine was accepted by the patient. A posterior direct decompression with instrumented fusion was performed from C3 to T1 (Figure 29-3).
Case 2
Imaging evaluation demonstrated several disc osteophyte complexes. The largest was observed at C3/C4, where there was 50% narrowing of the central canal. Extensive flowing nonmarginal osteophytes were also well characterized by CT scan (Figure 29-4). While no obvious unstable injuries were appreciated on CT, a subsequent MRI revealed extension distraction fractures with three column disruption at both C3-4 and C6-7. Each level of injury was associated with dissociation of the anterior longitudinal ligament and osteophytes (Figure 29-5). The spinal cord was compressed at C3-4 and C6-7.
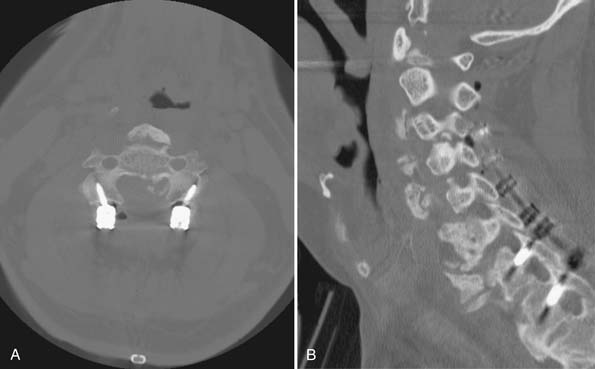
A C3 to C7 laminectomy and C3 to T1 instrumented fusion were performed. He tolerated the procedure well and was extubated in the operating room (Figure 29-6). Since the patient’s body habitus limited the adequacy of intraoperative radiographs, a CT scan was performed immediately postoperatively to evaluate the spinal alignment and instrumentation (Figure 29-7).

FIGURE 29-6 Case 2: Postoperative AP and lateral cervical spine x-rays with good sagittal and coronal alignment. Hardware in appropriate position without evidence of complications.
The hallmark spinal pathology seen in AS is due to enthesitis. The enthesis is the site of tendon and ligament attachment to bone. Local inflammation at the enthesis may lead to radiographic lysis of bone. AS affects the insertions and attachments of the discovertebral, costovertebral, and costotransverse joints, as well as the other interspinal ligaments. The reactive bone formation at the sites of inflammation and the remaining lysis result in a stiff and osteoporotic spine. This combination results in an increased susceptibility to spine fractures.6
Diffuse Idiopathic Skeletal Hyperostosis
The bone morphology in DISH is different than in AS. Whereas vertebrae with inflammation-induced osteolysis adjacent to affected entheses are commonly seen in AS, in DISH, bone quality is relatively well preserved. Both conditions, however, are associated with increased risk of fracture through or adjacent to ankylosed vertebral segments. These patients can present a challenge in correctly identifying a cervical fracture.7
Biomechanics and Classification of Subaxial Spine Fractures
In addition to classification is the question of subaxial spine instability after injury. White and Panjabi published a biomechanic study evaluating clinical and radiographic markers of cervical spine instability. Their work focused on the ligamentous structures surrounding the vertebral bodies. They developed a checklist with point values, with a score of five or more indicating instability. The radiographic markers on plain film are sagittal plane translation of >3.5 mm, sagittal plane rotation >11 degrees, positive stretch test, and abnormal disc narrowing. Clinical criteria are cord damage, root damage, and if dangerous loading is anticipated. There are two additional criteria: anterior elements unable to function and posterior elements unable to function. While this checklist, published in 1976, is a tool for evaluating spine instability, the commonplace use of CT and MRI has provided a level of detail and sensitivity that has made the point system infrequently used.
More recently, a classification system has been developed using the injury morphology, discoligamentous complex, and neurological status to classify injuries and to determine the need for surgical intervention. This subaxial cervical spine injury classification system (SLIC) by the Spine Trauma Study Group (STSG) was developed not only to classify subaxial spine fractures but also to predict the need for surgical stabilization and/or reduction. The system is based on assigning points according to the severity of injury in three categories: proposed mechanism of injury, discoligamentous complex injury, and neurological injury. If a patient’s SLIC score is 1 to 3, then nonsurgical treatment is recommended. If the score is 5 or more, then surgical treatment is recommended (Table 29-1). To assess the reliability and validity of this classification system, 20 surgeons in two different settings used the system to classify 11 different spine fractures and clinical scenarios. They found the reliability to be slightly lower than that of the Ferguson and Allen classification. The validity was good in comparison to the Ferguson and Allen classification system. Of note is that 93% of the time, the surgical versus nonsurgical treatment recommended by SLIC was the treatment recommendation of the practicing clinician.
TABLE 29-1 The Subaxial Cervical Spine Injury Classification System (SLIC)
| Points∗ | |
|---|---|
| Morphology | |
| No abnormality | 0 |
| Compression + burst | 1+1=2 |
| Distraction (e.g., facet perch, hyperextension) | 3 |
| Rotation or translation (e.g., facet dislocation, unstable teardrop or advanced-stage flexion-compression injury) | 4 |
| Discoligamentous complex | |
| Intact | 0 |
| Indeterminate (e.g., isolated interspinous widening, MRI signal change only) | 1 |
| Disrupted (e.g., widening of anterior disc space, facet perch or dislocation) | 2 |
| Neurological status | |
| Intact | 0 |
| Root injury | 1 |
| Complete cord injury | 2 |
| Incomplete cord injury | 3 |
| Continuous cord compression (neuro modifier in the setting of a neurological deficit) | +1 |
∗ A score of 3 or less indicates nonoperative management. A score of 5 or greater indicates need for surgical intervention.
Clinical Practice Guidelines
The importance of identifying cervical spine fracture, instability, or injury in the geriatric trauma patient cannot be overstated. Many characteristics of the geriatric population make identifying these injuries difficult. An accurate history of events surrounding the injury may be difficult, due to altered consciousness at the time of injury, associated head injuries, or baseline dementia. Additionally, a complete physical examination may be limited by altered mental status or by underlying medical conditions that alter the exam. Radiographic interpretation can, at times, be very difficult due to degenerative changes. Even when a diagnosis is made, there can be significant medical comorbidities that increase the morbidity and mortality related to these fractures.
The timing of surgery, especially in regards to central cord syndrome, remains controversial. All patients with central cord syndrome should be treated aggressively with medical therapies. These therapies include rigid cervical orthosis, intensive care unit admission for monitoring, mean arterial pressure >85 mm Hg, intravenous pressors if needed to maintain blood pressure, and early involvement of physical and occuptional therapy. Surgical intervention in central cord injury is indicated if there is progressive neurological deficit or overt spinal instability requiring reduction and fixation. If surgery is to be performed, there is new evidence that early surgical decompression (<24 hours after injury) improves neurological recovery more than late surgical decompression (>24 hours after injury). However, there is no current consensus on the timing of surgical intervention for central cord syndrome.8
Clinical Case Examples: Treatment, Clinical Challenges, and Future Treatments
Case 1
This patient had a low-energy mechanism resulting in central cord syndrome with no evidence of fracture or ligamentous injury on initial CT imaging. Historically, central cord syndrome has been treated medically with a limited role for operative decompression. Hadley reviewed the historical trends of central cord syndrome and showed that historical treatments are being revisited.9 The age-old nonoperative treatment strategy was based on the case series reported by Schneider in the early 1950s. His initial series reported 50% mortality rate in two central cord patients surgically decompressed. The other patient had recovery similar to the nonoperatively treated patients. Four years later, in 1958, he published a second series in which 20 patients were reviewed. Three of the patients were treated surgically; one patient was treated early, and two patients weeks after their injury. The patient treated early had dramatic neurological improvement. Of the patients surgically decompressed later, one of the two late patients had neurological recovery similar to those managed medically. The other suffered neurological injury and was quadriplegic. Despite the fact that these patients underwent agressive retraction of the injured spinal cord, with transdural approaches to resect anterior osteophytes, and with sectioning of the dentate ligaments, the conclusion from this series was to treat central cord syndrome medically. This guided much of the thinking toward treatment of central cord syndrome from that time forward. It was not until Brodkey, in 1980, published his results of seven operatively treated patients with traumatic central cord syndrome that surgical management was again revisited. These patients were selected for surgery because their neurological recovery had plateaued and myelography showed anterior compression of the spinal cord. Of the seven patients, all patients’ trajectories of neurological recovery improved, and three patients had full neurological recovery. After reviewing the most recent data with regard to treatment of central cord syndrome, Hadley et al. concluded that early reduction of fracture-dislocation is recommended, and surgical decompression of the compressed spinal cord is warranted, especially if the compression is focal and anterior.
The operative technique highlights a well-reported complication of posterior cervical decompression. The incidence of C5 nerve palsy after posterior decompression is approximately 5%. Half of the patients have sensory deficits or pain, and the other 50% have motor weakness only. It is generally unilateral, but is seen bilaterally in about 10% of cases. A recent study showed the cervical spinal cord drifted posteriorly approximately 2.8 mm at 24 hours after surgery and then decreased to 1.9 mm, 2 weeks after surgery. Interestingly, the absolute posterior drift was at the C5-6 level. In their study of 19 patients, two patients developed C5 nerve palsy. These two patients had the largest degree of posterior drift seen at 24 hours and 2 weeks.10 This C5 nerve palsy associated with posterior decompression generally has a good prognosis. Nearly all patients with a C5 palsy with 3/5 or 4/5 strength regain their strength by 6 months, with half having full recovery by 3 months.
Case 2
The degree of osteophyte formation made interpretation of the CT scan difficult. It was unclear to both the consulting spine surgeon and the interpreting radiologist whether there had been a bony injury to the cervical spine. An MRI demonstrated the fracture through the C3-4 and C6-7 disc spaces. The degree of injury is significant, and even after further review, difficult to see on CT scan. In patients with degenerative spines that preclude accurate assessment by x-ray or CT, it may be warranted to perform dynamic cervical spine x-rays or an MRI. Clinical clearance of the ankylosed cervical spine should be done with caution, as evaluation of neck pain in the DISH patient is not a reliable clinical tool; many DISH patients have neck pain at baseline.
1. Sokolowski M.J., et al. Acute outcomes of cervical spine injuries in the elderly: atlantaxial vs subaxial injuries, J. Spinal Cord Med.. 2007;30(3):238-242.
2. Whang P., et al. The management of spinal injuries in patients with ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis: a comparison of treatment methods and clinical outcomes. J Spinal Disord. Tech.. 2009;22(2):77-85.
3. Vaccaro A.R., et al. The subaxial cervical spine injury classification system. Spine. 2007;32:2365-2374.
4. Como J.J., et al. Practice management guidelines for identification of cervical spine injuries following trauma: update from the eastern association for the surgery of trauma practice management guidelines committee. J. Trauma. 2009;67(3):651-659.
5. Brandenstein D., et al. Unstable subaxial cervical spine injury with normal computed tomography and magnetic resonance initial imaging studies: a report of four cases and review of the literature. Spine. 2009;34(20):E743-E750.
6. Kubiak E.N., et al. Orthopedic management of ankylosing spondylitis. Journal of the American Academy of Orthopaedic Surgeons. 2005;13:267-278.
7. Belanger T.A., et al. Diffuse idiopathic skeletal hyperostosis: musculoskeletal manifestations. JAAOS. 2001;9:258-267.
8. Nowak D., et al. Central cord syndrome. Journal of the American Academy of Orthopaedic Surgeons. 2009;17(12):756-765.
9. Hadley M.N., et al. Management of acute central cervical spinal cord injuries. Neurosurgery. 2002;50(3):S166-S172.
10. Shiozaki T., et al. Spinal cord shift on magnetic resonance imaging at 24 hours after cervical laminoplasty. Spine. 2009;34(3):274-279.