37 Structural Osteoplasty: The Treatment of Vertebral Body Compression Fractures Using the OsseoFix Device
KEY POINTS
Introduction
The incidence of osteoporosis and osteoporotic vertebral compression fractures (VCFs) increases with advancing age with an estimated incidence of more than 50% in women over the age of 80 years.1 Adverse anatomical and biomechanical consequences of osteoporotic VCFs contribute substantially to the chronic morbidity and economic impact of osteoporosis.1 With increasing demand for improved quality of life, immediate pain relief, early mobilization, and preservation of function have become the goals for the management of osteoporotic VCFs.2
A single vertebral body compression fracture results in a sagittal plane deformity and greater flexion bending moment around the fractured vertebral body, thereby decreasing the force required to cause further increase in degree and number of additional VCFs with a corresponding increase in kyphosis.1 Spinal deformity resulting from the loss of vertebral body height also leads to loss of pulmonary capacity, malnutrition, decreased mobility, and depression.3 Kyphosis secondary to osteoporotic vertebral compression fractures is associated with a two to three times greater incidence of death due to pulmonary causes.3 Moreover, the pain associated with acute VCFs may be incapacitating and may become chronic in a significant number of cases.4 Interventions that restore fractured vertebral height and stabilize the fractured segment are presumed to improve spinal biomechanics and thereby mitigate these consequences.5,6
Description of the Osseofix Device
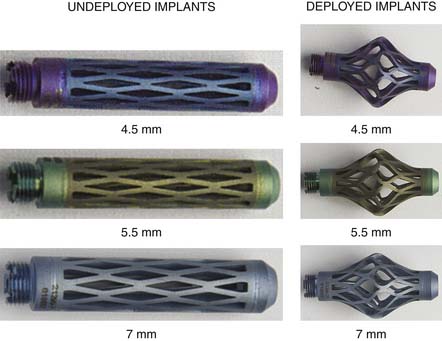
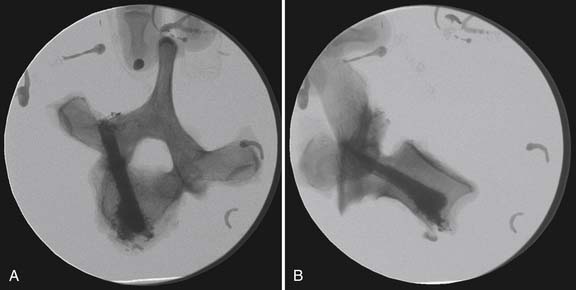
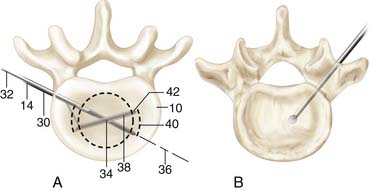
The OsseoFix device is a titanium implant composed of surgical grade titanium alloy (Ti-6Al-4V, ASTM F 136) and commercially pure titanium (Ti-CP2, ASTM F 67) with an electrolytic conversion coating. It is a cylindrical-shaped capsule, which expands in the middle after deployment and helps reduce the vertebral fracture and maintains the vertebral body height. Cement is then injected into the deployed implant. The implant is available in various sizes to provide versatility for individual anatomical dimension needs (Figure 37-1; Table 1).
Biomechanical Studies
The OsseoFix implant has undergone intense in vitro biomechanical testing in terms of stiffness, yield load, and ultimate load after insertion into a fractured vertebral body.7,8 These studies have evaluated the biomechanical stability of vertebral compression fractures repaired using kyphoplasty type repair techniques compared to several methods of using the OsseoFix repair technique.7,8
In the first reported in vitro biomechanical study evaluating the OsseoFix implant, four male human cadaveric (age 68 ± 9 yrs) spines from T2 to L5 were scanned for bone mineral density (BMD) using a 3-D computed tomography (CT) BMD measurement system (average BMD across spines and all levels = 119 ± 44 mg/ml). Individual vertebral bodies were sectioned from each spine and measured for anterior vertebral body height. Once measured, the intact vertebral bodies were mechanically tested using established techniques.5,6
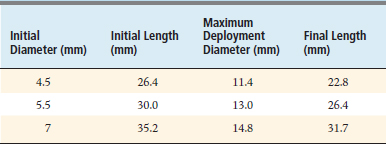
To summarize these techniques, the intact vertebral bodies were placed within a test frame with custom fixtures and epoxy resin that conformed to the upper and lower vertebral body endplates (Figure 37-2). Vertebral bodies were then compressed by 25% of the measured intact anterior vertebral body height (30-mm height × 25% = 7.5 mm compression). Following intact testing, data for stiffness (N/mm), yield load (N), and ultimate load (N) were calculated.
Fractured vertebral bodies were then randomly assigned to one of two repair groups: those using standard kyphoplasty or those using the smallest possible OsseoFix device (4.5 mm) (Figures 37-3 and 37-4). Both groups were injected with PMMA cement. Following repair, anterior column heights were remeasured to once again compress the vertebral bodies by 25% of the anterior column heights. The same data were calculated for the repair groups. Data between intact and repaired vertebral bodies as well as data between types of repairs were evaluated using a two-way ANOVA (p < .05). In addition, the volume of cement injected and the height maintained following testing of the repaired vertebral bodies were evaluated with a one-way ANOVA (p < .05).
Results – Study 1
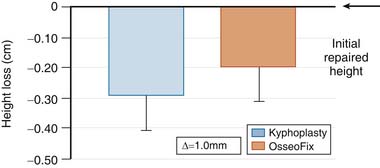
Data from this initial study found no differences in anterior column height between repair techniques in the intact or repaired phases. However, there was a statistically greater amount of height maintained following mechanical compression of the repaired vertebral bodies for the OsseoFix group compared to the kyphoplasty group (Figure 37-5). In addition, it was found that statistically less cement was injected (1 ml less) for the OsseoFix group compared to the kyphoplasty group.
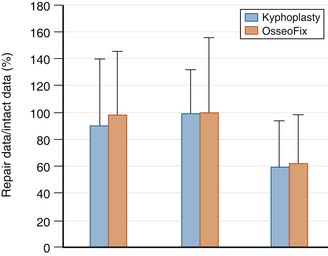
There were no differences found in any of the mechanical variables between OsseoFix or kyphoplasty repair groups. These data were then normalized to the intact data to evaluate the ability of each repair technique to restore the vertebral body to its intact mechanical strength (Figure 37-6). The normalized data were not statistically different between repair groups. The yield load and ultimate load were restored to intact values, but the stiffness did not reach intact values. This result is similar to data previously reported for vertebroplasty or kyphoplasty biomechanical restoration of fractured vertebral bodies.5,6
Results – Study 2
Because of the strength provided by the smallest possible implant with the lower injected cement volumes, a second biomechanical study was conducted to evaluate the inherent strength provided by the implant alone when compared to kyphoplasty and OsseoFix implants with cement.8 This study followed identical specimen preparation as the previous biomechanical study.7 However, in the second study, the OsseoFix implant repairs were selected based on pedicle width and height and the desired amount of repair height. In addition, the mechanical data were normalized to the BMD of individual vertebral bodies to understand how fractures may be stabilized by eliminating the effect of the inherent bone density.
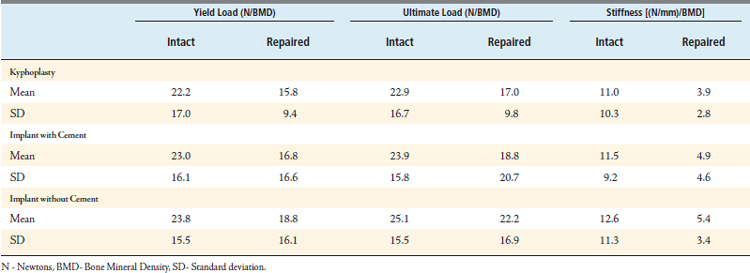
This study found no mechanical difference for any of the mechanical variables among the kyphoplasty type repair, the OsseoFix with cement repair, and the OsseoFix repair without cement (Table 37-2). Thus an OsseoFix implant alone (without cement) provides biomechanical strength that is equivalent to the other repair techniques evaluated. Whereas the definitive explanation remains unclear, it may be related to the compliance or elasticity of the commercially pure titanium expandable region deforming beneath the superior endplate when loaded. When using the cement, the bolus underneath the superior endplate may not be as elastic and thus causes more directed loading to the endplate and lower stability. Further visualization studies are needed to understand the deformation of the implant in real-time while being loaded. It also may be possible to use alternative injectable materials within the OsseoFix implant, because the implant provides stability and structural support that is not required from the injectable material. Again, further studies are warranted to understand the fracture stabilization provided in this scenario.
Clinical Data
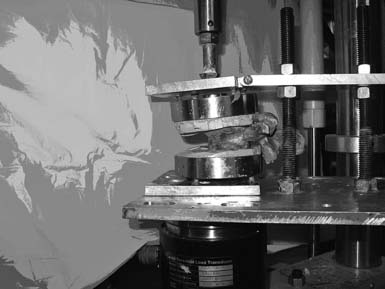
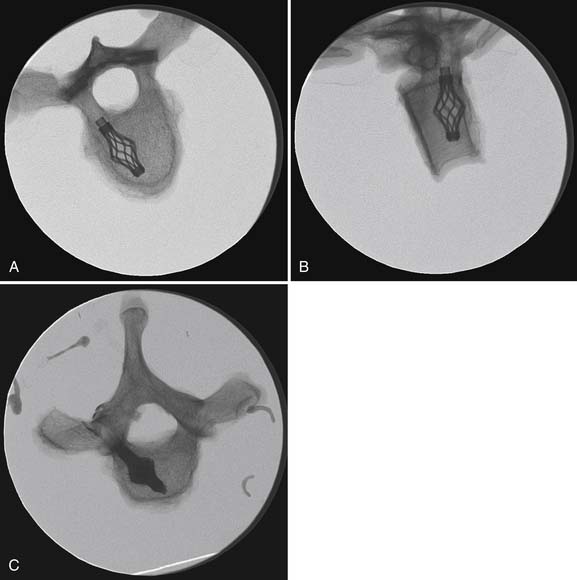
The first case of vertebral compression fracture reduction and internal fixation using OsseoFix fracture reduction system was done by Dr. Rudolf Bertagnoli on July 21, 2008, at Bogen center in Germany. Several hundred patients have received this treatment since then. The first patient was suffering from acute T12 vertebral compression fracture (Figure 37-7). The surgeon was able to achieve considerable height (Figure 37-8). The patient got immediate pain relief and did not require any external bracing or support. Two such cases have been done to date with good clinical outcomes, and no complications have been reported so far.
Operative Technique
Step 2: Creating an access channel into the vertebral body (Figure 37-9)
A 1-cm incision is then made over the bony prominences at the marked level. A targeting Jamshedi cannula with trocar is then placed into the vertebral body via transpedicular or extrapedicular approach. The trocar is then replaced with a guide wire through the Jamshedi cannula. The position of the guide wire must be verified using fluoroscopy at this stage. The Jamshedi cannula is then removed and replaced with a drill sleeve. A pathway is created into the anterior one third of the vertebral body by drilling over the guide wire through the drill sleeve (Figure 37-10). The pathway should end a few mm posterior to the anterior cortex. Position is reconfirmed with fluoroscopy, and the drill is removed, keeping the guide wire in place.
Step 4: Cement delivery
The cement powder is mixed with the liquid monomer in the mixing chamber at room temperature. The delivery gun is then loaded with the desired amount of cement. A bone biopsy cannula is inserted through the implant inserter into the most distal portion of the implant. The cement delivery gun is connected to the extension tube. The desired amount of cement is then injected through the bone biopsy cannula into the vertebral body under live AP and lateral fluoroscopy. The cement should never be inserted directly through the implant inserter tube. The cement injection is stopped when a sufficient amount has been placed to stabilize the fracture, if cement reaches cortex or an endplate, or leakage is noted. The bone biopsy and the insertion cannula are removed after the cement delivery has been completed. Final fluoroscopic images are taken and the skin is closed.
Treatment Alternatives
Vertebroplasty, or augmentation of the vertebral body with cement, was first used in the 1980s for the management of vertebral hemangioma, and later its use was extended to the management of painful osteoporotic VCFs and osteolytic metastasis of spine. The success rate of vertebroplasty for relief of pain is very high as reported in various studies.9 Cement interdigitates with the trabecular bone of vertebra and thus strengthens the vertebra. However, vertebroplasty does not correct the sagittal alignment, which is important for better biomechanics and to prevent the progression of kyphosis.10 Moreover, some studies have reported cement leakage and embolism with vertebroplasty, possibly a result of cement injection under high pressure.11
Kyphoplasty is a minimally invasive procedure involving the insertion of a bone tamp “pump” via a small cortical window, allowing the low-pressure injection of bone cement (PMMA) into a compression fracture to restore vertebral body height. Kyphoplasty is supposed to correct the vertebral deformity and thus improve the sagittal alignment of spine. It is also argued that cement is injected under low pressure in kyphoplasty, because a cavity is usually created with the bone tamp before the cement is injected. Recent studies have shown that injection pressures depend on the size of the cannula and rate of injection rather than creation of intravertebral cavity. One of the problems with kyphoplasty is that some of the restored height is lost on removal of the balloon tamp before insertion of cement. Also, because the cement bolus does not interdigitate with the cancellous bone in kyphoplasty, it compresses the adjacent cancellous bone with progressive loading and leads to some loss of regained height.
1. Kado D.M., Browner W.S., Palermo L., et al. Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch. Intern. Med. 1999;159(11):1215-1220.
2. Garfin S.R., Buckley R.A., Ledlie J. Balloon kyphoplasty for symptomatic vertebral body compression fractures results in rapid, significant, and sustained improvements in back pain, function, and quality of life for elderly patients. Spine. 2006;31(19):2213-2220.
3. Schlaich C., Minne H.W., Bruckner T., et al. Reduced pulmonary function in patients with spinal osteoporotic fractures. Osteoporos. Int. 1998;8(3):261-267.
4. Silverman S.L., Minshall M.E., Shen W., et al. The relationship of health-related quality of life to prevalent and incident vertebral fractures in postmenopausal women with osteoporosis: results from the Multiple Outcomes of Raloxifene Evaluation Study. Arthe. Rheum. 2001;44(11):2611-2619.
5. Kim C., Mahar A., Perry A., et al. Biomechanical evaluation of an injectable radiopaque polypropylene fumarate cement for kyphoplasty in a cadaveric osteoporotic vertebral compression fracture model. J. Spinal. Disord. Tech. 2007;20(8):604-609.
6. Perry A., Mahar A., Massie J., et al. Biomechanical evaluation of kyphoplasty with calcium sulfate cement in a cadaveric osteoporotic vertebral compression fracture model. Spine J. 2005;5(5):489-493.
7. V. Upasani, C. Robertson, D. Lee, et al. Biomechanical comparison of kyphoplasty versus a titanium mesh implant for stabilization of vertebral compression fractures. Spine (Accepted, In Press).
8. Ghofrani H., Nunn T., Robertson C., et al. Biomechanical evaluation of a titanium mesh implant compared to kyphoplasty: is bone cement necessary for vertebral body fracture stabilization?. San Francisco, Calif.: Presented: at meeting of North American Spine Society; 2009.
9. Garfin S.R., Yuan H.A., Reiley M.A. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine. 2001;26(14):1511-1515.
10. Kasperk C., Hillmeier J., Noldge G., et al. Treatment of painful vertebral fractures by kyphoplasty in patients with primary osteoporosis: a prospective nonrandomized controlled study. J. Bone Miner. Res. 2005;20(4):604-612.
11. Majd M.E., Farley S., Holt R.T. Preliminary outcomes and efficacy of the first 360 consecutive kyphoplasties for the treatment of painful osteoporotic vertebral compression fractures. Spine J. 2005;5(3):244-255.