41 Structural Kyphoplasty: The StaXx FX System
KEY POINTS
Introduction
Hadjipavlou et al1 provided a thorough review of the existing literature for these procedures. The reported success rates for these procedures is consistently above 80% (defined as patient-reported good to excellent pain response) with risk for certain complications. These complications include a transient increase in pain, infection, leakage of cement, and secondary vertebral compression fractures. With kyphoplasty, there have been a small number of reports of balloon rupture, but the failed balloons were withdrawn without incident. Cement leakage is the most common cause of pulmonary or neurological complications. The comparison of cement leakage risk between kyphoplasty and vertebroplasty remains controversial. Some reports suggest a clinically insignificant difference in risk, whereas others suggest that kyphoplasty is associated with less leakage.
Both vertebroplasty and kyphoplasty may increase the risk of subsequent vertebral fractures, particularly at the adjacent level. Some have hypothesized that this may be due to changes in load distribution across the endplate that occur when disc is pressure lost after endplate fracture. Fracture of the endplate increases the volume for the nucleus pulposus and reduces its ability to hydrostatically resist compressive load. In flexion, the reduced load on the nucleus causes greater load on the annulus and the anterior cortex of the vertebral body adjacent to the fractured endplate. This mechanism is being investigated by Patwardhan et al.2 Some have speculated that the addition of cement to the vertebral body increases the stiffness of the vertebral body and that this may play a role in subsequent fractures. The effect of cement on the treated and adjacent levels is still being studied, but it appears that this effect is small compared to bone mineral density.3
Advocates of kyphoplasty believe that the procedure actually reduces the rate of adjacent level fractures, compared to vertebroplasty, because it more effectively reduces the fracture. However, no randomized studies have been conducted to compare the two techniques, and the natural history of adjacent level fractures has been difficult to quantify. Frankel and Vandergrift4 reviewed the results of 2,000 patients enrolled in a trial evaluating bisphosphonate in patients with vertebral compression fractures. The authors noted that the rates of new fractures were 7.9% and 15% in patients treated with bisphosphonate and placebo, respectively. Moreover, in the bisphosphonate group, only 3.4% of new vertebral compression fractures were at the adjacent level, compared to 7.1% in the placebo group.4 Frankel and vandergrift review of the literature found the rates of subsequent adjacent level fractures following kyphoplasty to be 13% compared to 10% with vertebroplasty, suggesting that cement implantation with both of these techniques increased the risk of subsequent fractures compared to natural history.4
Frankel et al5 compared outcomes in a series of 17 patients (20 fractures) undergoing kyphoplasty and 19 patients (26 fractures) undergoing vertebroplasty. The authors reported an average of 4.65 ml and 3.78 ml of cement per vertebral body with kyphoplasty and vertebroplasty, respectively. There were five adjacent level fractures in three kyphoplasty patients (3/17 [18%]) and none in the vertebroplasty group.5 Fribourg et al6 published a retrospective review of 38 patients (47 fractures) treated with kyphoplasty. Patients received between 1.5 and 6.0 ml cement per vertebral body. The authors reported that 10 patients (26%) had a subsequent fracture during the follow-up period (average 8 months), and 8 of those patients had a subsequent fracture within 2 months. The 8 patients with early “new fractures” all had a fracture at the adjacent level and the 2 patients with later “new fractures” all had fractures that were not adjacent to the index fracture.6
A larger study was performed by Harrop et al6 in which 115 patients were treated with kyphoplasty. All patients had at least 3 months follow-up. In this group, 26 patients (22.6%) developed 34 new compression fractures. The authors then classified patients as having primary osteoporosis (80 patients) or secondary steroid-induced osteoporosis (35 patients) and calculated at the rate of subsequent fractures in each group. They reported that the incidence of postkyphoplasty compression factures in primary osteoporosis patients was 11%, and the incidence in the steroid-induced osteoporosis group was 49% (p < .00001).7 There was no mention of the use of bisphosphonates in these patients.
The Frankel4,5 and Harrop7 papers demonstrate that both bisphosphonates and steroids have a significant effect on bone quality and should be considered in any analysis of adjacent-level fractures following vertebroplasty or kyphoplasty. Each of these papers reported subsequent fractures in 18% to 26% of patients, with the best case being 11% in patients specifically with primary osteoporosis. Because the natural history of adjacent level fractures is likely between 8% and 15%, standard vertebroplasty and balloon kyphoplasty may actually increase the risk of subsequent compression fractures, despite the success in reducing a patient’s pain from the index fracture.4–7
Cadaver testing has been used to test the hypothesis that kyphoplasty is more efficacious for deformity correction than standard vertebroplasty. Belkoff et al8 experimentally created compression fractures in 16 osteoporotic vertebral bodies and treated them with either balloon kyphoplasty or vertebroplasty. The vertebral bodies were compressed to 25% of their initial height; however, there was an initial elastic recovery of about 15%. The authors measured the change in height with the application of cement and then subjected those vertebral bodies to compressive failure. The authors reported that 97% of the height loss was regained with kyphoplasty, whereas only 30% of height loss was regained with vertebroplasty.8 These results may not reflect the in vivo situation, because muscle forces and body weight will resist height restoration, as measured clinically by Voggenreiter.8 The vertebral bodies in both groups were found to be stronger after the application of cement. However, those treated with kyphoplasty were found to return to their initial stiffness, whereas those treated with vertebroplasty did not.9 Kim et al10 performed a similar cadaver evaluation with the addition of cyclic loading to determine how vertebral fracture correction was maintained over time. They reported that balloon kyphoplasty was able to restore vertebral height, but there was significant loss of height over 100,000 cycles of compressive load. Vertebroplasty was better able to maintain height under dynamic loading. Ultimately, after the cyclic testing regimen, the vertebrae treated with kyphoplasty had less height than those treated with vertebroplasty.10 In contrast to Belkoff,8 the vertebral bodies treated with vertebroplasty were more stiff than with kyphoplasty.
Cadaver studies of isolated vertebral bodies cannot capture the interaction between vertebral bodies or in vivo loads. Clinical data are necessary to realistically measure the ability to achieve reduction of a vertebral compression fracture. Pradham et al11 evaluated a series of 65 consecutive patients treated with kyphoplasty between 1 to 3 levels. Kyphoplasty reduced the local kyphotic deformity by an average of 7.3 degrees (63% of preoperative kyphosis), but this did not translate into a similar correction of overall sagittal alignment. Angular correction decreased to 2.4 degrees when measured from the level above to the level below. Similarly, the reductions decreased to 1.5 and 1.0 degree at spans of 2 and 3 levels above and below the index level, respectively. The authors concluded that it was unrealistic to expect a 1- or 2 -level kyphoplasty to significantly improve sagittal alignment after vertebral compression fracture.11
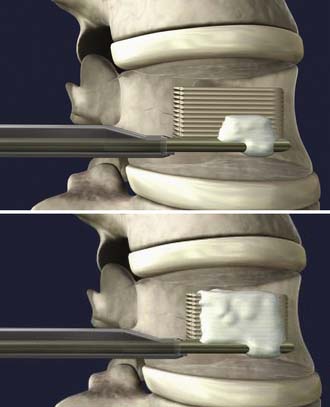
The StaXx FX Structural Kyphoplasty System (Spine Wave, Inc., Shelton, Conn.) was introduced to allow the physician to reduce the vertebral fracture and to correct the kyphotic deformity with a system of progressively stacked wavers made from PEEK (Figure 41-1). The permanent implant system allows controlled vertical expansion in situ and eliminates the intraoperative height loss that may occur after deflation of a balloon. Pradhan et al11 remarked that using balloons to reduce the fracture is not ideal, because the balloon and subsequently inserted cement follow a path of least resistance, resulting in localized stresses on the endplate. These localized stresses compromise the endplate’s ability to maintain an improvement in the spine’s overall sagittal alignment. The geometry of the StaXx system includes a wide, flat surface to support the endplate, which encourages hydrostatic compression of the nucleus and normalization of load across the disc. This endplate support may enable the system to reduce the number of adjacent level fractures following treatment of an initial compression fracture. Tactile feedback and manual wafer implantation provide greater physician control and directed axial expansion to reduce the fractured endplate.
Background of Scientific Testing and Clinical Outcomes
Cadaveric testing by Dr. Stephen M. Belkoff has shown similarities in both strength and stiffness between balloon kyphoplasty and structural kyphoplasty (presented at the Annual Meeting of Congress of Neurological Surgeons, September 15-20, 2007).12 The study methods compared bilateral Kyphon Bone Tamp (KyphX) and unilateral StaXx FX Structural Kyphoplasty (Spine Wave Shelton, CT USA). Vertebral bodies were preconditioned with a preload of 89 N and then subjected to compressive loading at a displacement rate of 5 mm/min until the body had lost half its height. The fractures were then put under a preload of 144 N to simulate a recumbent position during surgery and treated with either KyphX or StaXx. The average cement volume when using StaXx was 2.50 ml, compared with 7.25 ml with KyphX. Restoration of vertebral body height was greatest in the anterior portion of the body and only observed when using the StaXx device. The amount of height restoration was 5 to 10 mm. The authors observed that the inflatable bone tamps were able to restore height until they were deflated and removed. At this time, the compressive preload caused the vertebral body to lose all height restoration. Treated vertebral bodies were crushed again, and there were no significant differences in strength or stiffness between the two devices.11
Clinical Presentation and Evaluation
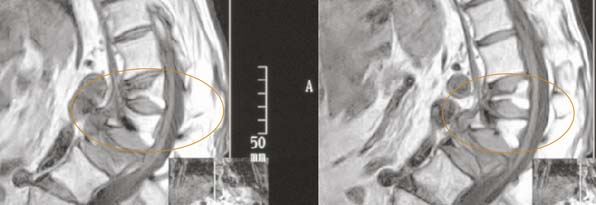
A standing scoliosis radiographic series should be performed, but at minimum a standing lateral view and a standing anteroposterior (AP) view are required. Magnetic resonance imaging (MRI) is imperative visualization to help pinpoint and confirm the location of the pain and visualize the fracture and it’s configuration. It is important to be aware that radiographs are of limited utility in determining if the fracture is acute or chronic. Ideally, a previous radiograph will be available so that a new vertebral fracture can be distinguished from an existing deformity of the vertebral body. MRI is particularly well suited for determining if the compression fracture is acute, because edema will accompany an acute fracture. A T2-weighted image will show this edema as a brighter area. The specificity of the film can be optimized with an imaging sequence altered to suppress the appearance of fat in the vertebral body, which also tends to show bright on FSE (fast spin echo) T2 images (Figure 41-2). The clinician should be aware that outside MRIs may not be collected with fat suppression and the diagnostic value of the film may be decreased. Alternatively in those cases, T1-weighted images will show an edema as a darker area (Figure 41-3). Computed tomography (CT) scans performed during the initial evaluation provide a better view of the fractured vertebra and the location of any resulting fragments. If the patient is not a suitable candidate for an MRI, then the CT scan in conjunction with nuclear medicine bone scan can also be used to establish fracture age. With any vertebroplasty or kyphoplasty procedure, endplate restoration and vertebral height augmentation are more readily achieved on active fractures. Typically, chronic fractures do not have a great deal of mobility and this may interfere with the ability to restore the endplate or augment the height of the vertebral body. In fact, reduction may not be possible on a chronic fracture.

FIGURE 41-2 A T2-weighted MRI sequence with bright edema, indicating an active fracture.
(Images courtesy of Orlando Ortiz, MD.)
All results should be compared with the patient-reported location, to determine if the pain is a result of the fractured body. A T-score determination is useful in determining if a patient has osteoporosis or not, especially with a first-time fracture, and requires bisphosphonate medications to help prevent further bone loss.
Operative Technique
Position
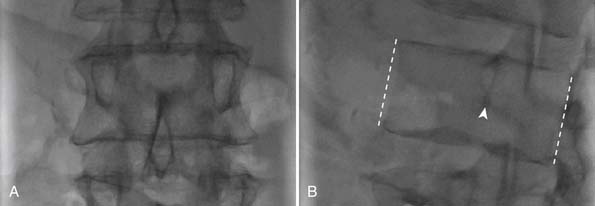
The patient should be placed in the standard prone position. Placement of the StaXx Structural Kyphoplasty device is performed under fluoroscopy using a peripedicular approach. First, the vertebral body is viewed en face in both AP and lateral images. It’s important that the AP image be square to the vertebral body and not the patient; thus the C-arm must be rotated to account for the lateral curvature of the spine. Once the C-arm is properly oriented for the AP view, the arm should be rotated until the lateral aspect of the pedicle has moved over about 50% of the vertebral body (Figure 41-4). A perpendicular line should be dropped from the lateral aspect of the pedicle toward the inferior endplate (Figure 41-5). The target is on this perpendicular line, 3 to 5 mm superior to the inferior endplate. The targeting needle should be coincident with the C-arm, similar to looking down a rifle barrel. This trajectory ensures that the needle will be placed above Kambin’s triangle, which is a safe area avoiding the exiting nerve roots below.
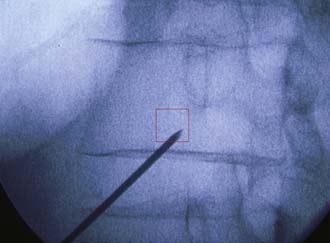
FIGURE 41-5 The red box indicates the peripedicular area targeted during needle placement.
(Image courtesy of Wayne Olan, MD.)
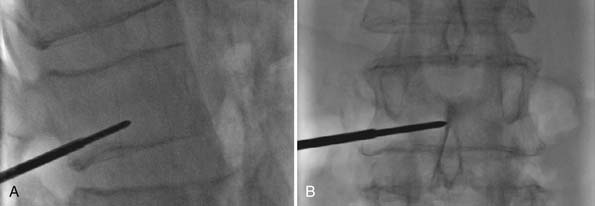
Confirmation of needle placement is observed in the AP and lateral views (Figure 41-6). The needle stylet is removed, and a Steinmann pin is advanced to the midline in both the AP and lateral views. This confirms the proper trajectory and subsequent positioning of the stack in the center of the vertebral body.
Procedure
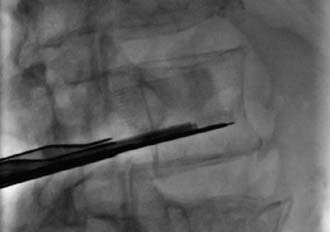
The C-arm is then rotated perpendicular (90 degrees) to the instrumentation and fluoroscopy is used to confirm that the introducer and access port assembly are inserted in the vertebral body, allowing the Steinmann pin to be removed. The access port assembly is advanced until sufficiently secured in the cortical wall (Figure 41-7). The introducer is then removed, leaving the access port. Under perpendicular and lateral fluoroscopic guidance, a depth gauge is used to determine the length across the vertebral body (Figure 41-8).
After the wafer length is selected, the wafer cartridge is inserted into the implant delivery gun. The gun and cartridge assembly is primed and inserted into the access port under perpendicular fluoroscopic guidance (Figure 41-9). Using lateral fluoroscopic guidance, 1-mm interlocking stackable PEEK wafers are inserted sequentially, allowing for direct control of the fracture reduction (Figure 41-10).
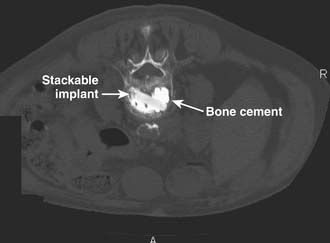
Fracture reduction, tactile feedback, superior endplate deformation, or inferior cartridge track deflection are stopping points for wafer insertion. Once the gun has been removed from the access port, still in the lateral view, a port seal is used to guide the cement needle along the anterior side of the wafer stack. Bone cement, mixed to a toothpaste consistency, is injected anterior to the wafer stack for stabilization. The cement advances up the wafer stack, filling the anterior aspect of the vertebral body. If the cement does not flow across midline, in the AP view, additional cement may be placed posterior to the wafer stack (Figure 41-11).
Postoperative Care
The structural kyphoplasty procedure is generally performed in the outpatient setting, as is the case with vertebroplasty or balloon kyphoplasty. The patient is typically discharged home after standard postprocedure recovery care. Standing radiographs may be obtained before patient discharge.
Complications and Avoidance
Although structural kyphoplasty uses less cement than the traditional balloon kyphoplasty, there is still the potential for cement to leak outside of the vertebral body. Patients should be monitored for signs and symptoms of soft tissue damage, nerve root pain, cord compression, and neurological impairment. These complications may not always be evident immediately following the procedures. The physician should assess for these events at follow-up either in the office or via the phone.
Case Studies
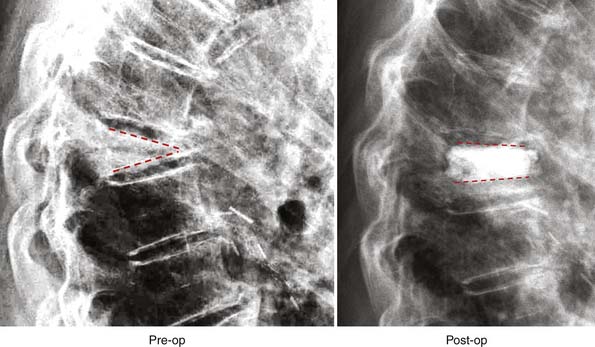
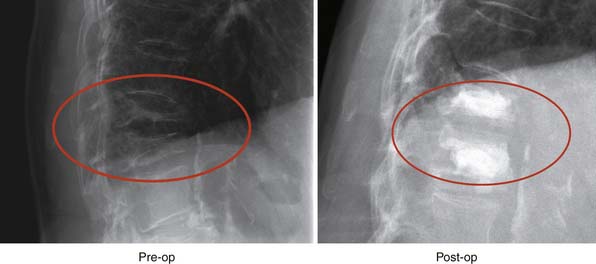
Two case studies are provided. The first is shown in Figure 41-12. This demonstrates a compression fracture with almost complete loss of anterior height. The inferior and superior endplates form an angle of 45 degrees. Following the application of StaXx and cement, much of the anterior height is restored, and the endplates form an angle of 30 degrees. The reduction required 11 wafers and 3 ml cement. The second case study is shown in Figure 41-13. This demonstrates reduction of a two-adjacent-vertebrale compression fracture. Following reduction, the kyphotic angle had improved from 38 degrees to just 21 degrees. The cement shows good diffusion through the both vertebral bodies.
1. Hadjipavlou A.G., Tzermiadianos M.N., Katonis P.G., et al. Percutaneous vertebroplasty and balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures and osteolytic tumors. JBJS. 2005;87-B(12):1595-1604.
2. M. Tzermiadianos, A. Hadjipavlou, S. Renner, et al., Altered disc properties after an osteoporotic vertebral fracture. Is it a risk factor for adjacent fractures? Journal of Bone and Joint Surgery – British, Vol. 91-B, Issue (Suppl. 1), 108-109
3. Luo J., Skrzypiec D.M., Pollintine, et al. P. Mechanical efficacy of vertebroplasty: influence of cement type, BMD, fracture severity, and disc degeneration. Bone. 2007;40(4):1110-1119.
4. Frankel B and Vandergrift A. The natural history of subsequent adjacent level vertebral compression fractures. Paper #13. Presented at the North American Spine Society 22nd Annual Meeting, October 23-27, Austin, Texas.
5. Frankel B.M., Monroe T., Wang C. Percutaneous vertebral augmentation: an elevation in adjacent-level fracture risk in kyphoplasty as compared with vertebroplasty. Spine J. 2007;7:575-582.
6. Fribourg D., Tang C., Sra P., et al. Incidence of subsequent vertebral fractures after kyphoplasty. Spine. 2004;29(20):2270-2276.
7. Harrop J.S., Prpa B., Reinhardt M.K., et al. Primary and secondary osteoporosis incidence of subsequent vertebral compression fractures after kyphoplasty. Spine. 2004;29(19):2120-2125.
8. Belkoff S.M., Mathis J.M., Fenton D.C., et al. An ex vivo biomechanical evaluation of an inflatable bone tamp used in the treatment of compression fracture. Spine. 2001;26(2):151-156.
9. Voggenreiter G. Balloon kyphoplasty is effective in deformity correction of osteoporotic vertebral compression fractures. Spine. 2005;30(24):2806-2812.
10. Kim M.J., Lindsey D.P., Hannibal M., et al. Vertebroplasty versus kyphoplasty: biomechanical behavior under repetitive loading conditions. Spine. 2006;31(18):2079-2084.
11. Pradhan B.B., Bae H.W., Kropt M.A., et al. Kyphoplasty reduction of osteoporotic vertebral compression fractures: correction of local kyphosis versus overall sagittal alignment. Spine. 2006;31(4):435-441.
12. Belkoff S.M., Manzi R., Paxson R.D. Mechanical comparison of vertebral body compression fracture reduction: StaXx FX versus Kyphoplasty. Annual Meeting of Congress of Neurological Surgeons. September 15-20, 2007.