Chapter 2 Stress, Inflammation, and Shock
The systemic inflammatory changes that accompany cardiac surgery and cardiopulmonary bypass can sometimes result in a clinical state that resembles septic shock. It is now recognized that severe systemic inflammation is a nonspecific host response to a range of physiologic stressors, of which infection and cardiopulmonary bypass are but two examples. Additionally, there is evidence that inflammation plays an important role in other forms of shock (e.g., hemorrhagic and cardiogenic shock).
NEUROENDOCRINE AND METABOLIC EFFECTS
Tissue injury results in the activation of nociceptors, which transduce a signal of actual or threatened tissue damage, via the sensory neurones, to the medulla of the brain. This signal is then integrated within the brain stem and results in activation of the sympathetic nervous system, the renin-angiotensin-aldosterone system, and the hypothalamic-pituitary axis. Hypothalamic corticotropin releasing hormone stimulates the release of adrenocorticotropic hormone from the anterior pituitary, which in turn stimulates the release of cortisol and other glucocorticoids from the adrenal cortex. In addition, growth hormone is released from the anterior pituitary, vasopressin from the posterior pituitary, and glucagon from the pancreas. The secretion of thyroid hormones and insulin are suppressed.1
This neuroendocrine response results in a multitude of changes throughout the body.
THE INFLAMMATORY RESPONSE TO SURGERY AND CARDIOPULMONARY BYPASS
Inflammation is primarily a protective response to tissue injury that helps destroy or quarantine harmful agents or damaged tissue. Inflammation may be localized (e.g., the region of redness, swelling, and warmth surrounding an insect bite) or systemic. Systemic inflammation occurs in a variety of clinical situations, including major surgery, cardiopulmonary bypass, burns, pancreatitis, myocardial infarction, and sepsis. The systemic inflammatory response is a continuum. At one end of the spectrum is a barely detectable, self-limited state manifested by a mild fever, leukocytosis, and an increase in inflammatory markers (e.g., C-reactive protein). This is the situation that typically occurs following major surgery or a myocardial infarction. At the other end of the spectrum is a profoundly harmful, self-reinforcing syndrome manifested by circulatory shock and multiple organ failure.2,3
The Mechanisms of the Inflammatory Response
The mechanisms of inflammation and the interactions among the various components are extremely complex and only a brief description is provided here. The process is summarized in Fig. 2-1.
Contact Activation: Platelets, Coagulation, Complement
Endotoxin
Endotoxin is a lipopolysaccharide released from gram-negative bacteria during their growth and replication. Endotoxin can result in the production of large quantities of TNF-α and IL-6 by macrophages and endothelial cells. Endotoxemia is a critical component in the pathogenesis of gram-negative septic shock. Endotoxin is also present in the blood after cardiopulmonary bypass; its presence may be related to impaired gut barrier function due to splanchnic ischemia.5
Microvascular Dysfunction
Cardiac output is increased in systemic inflammatory states, but oxygen delivery and utilization within the tissues may be severely impaired. Although the overall effect of inflammation is increased nitric oxide production and systemic vasodilation, vasoconstriction also occurs. For instance, impaired synthesis of nitric oxide is thought to contribute to the increased pulmonary vascular resistance that occurs following cardiopulmonary bypass.6 Vasoconstriction may also occur due to endothelial production of thromboxane (a vasoconstricting prostaglandin) and endothelins. In addition, microvascular obstruction may occur due to thrombosis, leukocyte margination and aggregation, platelet activation, and reduced red cell deformability. Finally, there is evidence of impaired mitochondrial function in sepsis.7
The Clinical Manifestations of Severe Inflammation
The systemic inflammatory response syndrome (SIRS) is a clinical diagnosis defined by specific criteria (Table 2-1).8 Note that important hemodynamic instability is not a requirement for the diagnosis of SIRS. However, severe systemic inflammation often does result in profound circulatory disturbance. This disturbance is characterized by widespread vasodilation, myocardial depression (ejection fraction may be depressed but cardiac output may be dramatically increased), impaired peripheral perfusion due to microvascular failure, and relative hypovolemia due to intravascular fluid loss into the interstitium. Severe tissue hypoxemia may exist despite a very high cardiac output. Mixed venous oxygen saturation may be normal or increased and is not a good marker of tissue perfusion in this situation.
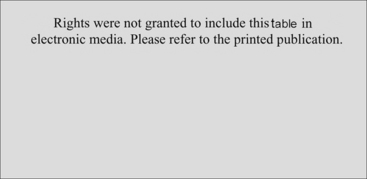
Table 2-1 Criteria for Diagnosis of the Systemic Inflammatory Response Syndrome
Rights were not granted to include this table in electronic media. Please refer to the printed book.
Bone RC, Balk RA, Cerra FB, et al: Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee, American College of Chest Physicians/Society of Critical Care Medicine. Chest 101:1644-1655, 1992.
If this clinical state occurs in the context of infection it is classified as either severe sepsis or septic shock (Chapter 35). In cardiac surgical patients, the condition is variably known as low systemic vascular resistance syndrome, vasoplegic shock, or culture-negative septic shock. Low systemic resistance occurs in 20% to 45% of patients after cardiac surgery9,10; severe shock occurs in 5% to 10% of patients.10,11
In addition to cardiovascular dysfunction, severe inflammation is associated with dysfunction of other organs, such as the lungs (acute lung injury, acute respiratory distress syndrome), kidneys, liver, gut, brain, and blood (coagulopathy, thrombocytopenia, and fibrinolysis). Involvement of multiple organs defines the condition of multiple organ dysfunction syndrome (MODS).8 MODS is a commonly described sequela of cardiac surgery; in one study MODS occurred in 11% of cardiac surgery patients and was associated with a mortality rate of 41%.12 Although MODS can occur as a consequence of inflammation-mediated vasoplegic shock, it can also occur as a result of other forms of shock (see subsequent material). In the cardiothoracic intensive care unit, cardiogenic shock is an important cause of MODS.
Prevention of SIRS and MODS
A wide range of strategies have been identified to attenuate the inflammatory response to cardiac surgery and cardiopulmonary bypass and potentially to reduce the incidence of MODS.2 They include limiting allogenic blood transfusion, using biocompatible (heparin-coated) bypass circuits, using warm-blood cardioplegia, avoiding the reinfusion of blood obtained via cardiotomy suction, performing cardiac surgery “off-pump,” using aprotinin, and employing specific anesthesia techniques such as the use of inhaled anesthetic agents (sevoflurane or isoflurane) and regional anesthesia (epidural). However, with most of these strategies only a reduction in inflammatory-mediator production has been identified, not improved survival rates.
The treatment of post-cardiac-surgery vasoplegic shock in the intensive care unit is primarily supportive (Chapter 20). However, there is some very limited evidence supporting specific therapies, such as corticosteroids,13 methylene blue,11 and vasopressin.14 Corticosteroids may also improve outcome after septic shock,15,16 although this effect is controversial. Human recombinant activated protein C appears to improve outcome after severe sepsis.17
A number of interventions have been shown to reduce the development of MODS and, in some cases, improve survival rates. These interventions include early goal-directed fluid therapy,18 restrictive blood transfusion,19 lung-protective ventilation,20 tight glycemic control,21 and enteral nutrition.22 The indications for and appropriateness of these therapies are discussed elsewhere in the book.
Shock
It is usual to think of the various types of shock as being distinct entities and, indeed, each type of shock has its own characteristic clinical features. For instance, warm, dilated peripheries are a feature of vasodilatory shock, and pulmonary edema is a trait of cardiogenic shock. However, the similarities among the various forms of shock are far more striking than the differences. All forms of shock result in the activation of identical neuroendocrine pathways and provoke a systemic inflammatory response. Myocardial dysfunction is the defining characteristic of cardiogenic shock, but it is also an important feature of septic shock.23,24 In fact, in some forms of septic shock, notably meningococcemia, myocardial dysfunction may be the primary hemodynamic manifestation.25 Hypovolemia is a feature not only of hypovolemic shock but also of vasodilatory shock. Indeed, prior to fluid resuscitation, septic shock may be clinically indistinguishable from hypovolemic shock. Also, there is evidence that hypovolemia and inappropriate vasodilation occur in cardiogenic shock.26,27
As already stated, systemic inflammation is strongly associated with certain forms of vasodilatory shock. However, shock itself, irrespective of the cause, precipitates a potent inflammatory response. Thus, following the initial period of resuscitation, cardiogenic shock28 and hemorrhagic shock29 resemble a sepsislike syndrome, with increased levels of inflammatory markers and pathologic vasodilation. One of the primary mechanisms of the postresuscitation systemic inflammatory response is ischemia-reperfusion,30 which is defined as tissue injury that is directly related to revascularization. Ischemia-reperfusion is also an important mechanism underlying myocardial stunning, as discussed in Chapter 1. All forms of shock can ultimately lead to MODS.
1 Desborough JP. The stress response to trauma and surgery. Br J Anaesth. 2000;85:109-117.
2 Laffey JG, Boylan JF, Cheng DC. The systemic inflammatory response to cardiac surgery: implications for the anesthesiologist. Anesthesiology. 2002;97:215-252.
3 Levy JH, Tanaka KA. Inflammatory response to cardiopulmonary bypass. Ann Thorac Surg. 2003;75:S715-S720.
4 Despotis GJ, Avidan MS, Hogue CWJr. Mechanisms and attenuation of hemostatic activation during extracorporeal circulation. Ann Thorac Surg. 2001;72:S1821-S1831.
5 Andersen LW, Landow L, Baek L, et al. Association between gastric intramucosal pH and splanchnic endotoxin, antibody to endotoxin, and tumor necrosis factor-alpha concentrations in patients undergoing cardiopulmonary bypass. Crit Care Med. 1993;21:210-217.
6 Beghetti M, Silkoff PE, Caramori M, et al. Decreased exhaled nitric oxide may be a marker of cardiopulmonary bypass-induced injury. Ann Thorac Surg. 1998;66:532-534.
7 Crouser ED, Julian MW, Blaho DV, et al. Endotoxin-induced mitochondrial damage correlates with impaired respiratory activity. Crit Care Med. 2002;30:276-284.
8 Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee, American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101:1644-1655.
9 Kristof AS, Magder S. Low systemic vascular resistance state in patients undergoing cardiopulmonary bypass. Crit Care Med. 1999;27:1121-1127.
10 Carrel T, Englberger L, Mohacsi P, et al. Low systemic vascular resistance after cardiopulmonary bypass: incidence, etiology, and clinical importance. J Card Surg. 2000;15:347-353.
11 Levin RL, Degrange MA, Bruno GF, et al. Methylene blue reduces mortality and morbidity in vasoplegic patients after cardiac surgery. Ann Thorac Surg. 2004;77:496-499.
12 Kollef MH, Wragge T, Pasque C. Determinants of mortality and multiorgan dysfunction in cardiac surgery patients requiring prolonged mechanical ventilation. Chest. 1995;107:1395-1401.
13 Kilger E, Weis F, Briegel J, et al. Stress doses of hydrocortisone reduce severe systemic inflammatory response syndrome and improve early outcome in a risk group of patients after cardiac surgery. Crit Care Med. 2003;31:1068-1074.
14 Morales DL, Gregg D, Helman DN, et al. Arginine vasopressin in the treatment of 50 patients with postcardiotomy vasodilatory shock. Ann Thorac Surg. 2000;69:102-106.
15 Annane D, Sebille V, Charpentier C, et al. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA. 2002;288:862-871.
16 Annane D, Bellissant E, Bollaert PE, et al. Corticosteroids for severe sepsis and septic shock: a systematic review and meta-analysis. BMJ. 2004;329:480.
17 Bernard GR, Vincent JL, Laterre PF, et al. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med. 2001;344:699-709.
18 Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368-1377.
19 Hebert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med. 1999;340:409-417.
20 Anonymous. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med. 2000;342:1301-1308.
21 van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med. 2001;345:1359-1367.
22 Perez J, Dellinger RP. Other supportive therapies in sepsis. Intensive Care Med. 2001;27(suppl 1):S116-S127.
23 Kumar A, Krieger A, Symeoneides S, et al. Myocardial dysfunction in septic shock: Part I I. Role of cytokines and nitric oxide. J. Cardiothorac Vasc Anesth. 2001;15:485-511.
24 Kumar A, Haery C, Parrillo JE. Myocardial dysfunction in septic shock: Part I. Clinical manifestation of cardiovascular dysfunction. J Cardiothorac Vasc Anesth. 2001;15:364-376.
25 Monsalve F, Rucabado L, Salvador A, et al. Myocardial depression in septic shock caused by meningococcal infection. Crit Care Med. 1984;12:1021-1023.
26 Laurent I, Monchi M, Chiche JD, et al. Reversible myocardial dysfunction in survivors of out-of-hospital cardiac arrest. J Am Coll Cardiol. 2002;40:2110-2116.
27 Hochman JS. Cardiogenic shock complicating acute myocardial infarction: expanding the paradigm. Circulation. 2003;107:2998-3002.
28 Adrie C, Laurent I, Monchi M, et al. Postresuscitation disease after cardiac arrest: a sepsis-like syndrome ? Curr Opin Crit Care. 2004;10:208-212.
29 Hierholzer C, Billiar TR. Molecular mechanisms in the early phase of hemorrhagic shock. Langenbecks Arch Surg. 2001;386:302-308.
30 Ar’Rajab A, Dawidson I, Fabia R. Reperfusion injury. New Horiz. 1996;4:224-234.