CHAPTER 162 Stereotactic Radiosurgery for Trigeminal Neuralgia
The French surgeon Nicholas Andre described “tic doulourex,” or trigeminal neuralgia, in 1756. Trigeminal neuralgia is characterized by a temporary paroxysmal lancinating or electric shock–like pain in the trigeminal nerve distribution and is typically confined to one side of the face but may be bilateral in rare cases. Pain-free intervals are common and vary in length from weeks to years. The prevalence of trigeminal neuralgia is 4 to 5 per 100,000.1 First-line treatment for trigeminal neuralgia is with medications. Medications typically employed include Tegretol (carbamazepine), Neurontin (gabapentin), Lyrica (pregabalin), and baclofen. Other kinds of facial pain broadly called atypical trigeminal neuralgia may occur with deafferentation, trauma, multiple sclerosis, somatoform pain disorders, and herpes zoster; more appropriate classification schemes exist.2 Nonetheless, treatment options for these types of facial pain are fairly similar to those used for trigeminal neuralgia, but the treatment options are usually less effective.
Because most patients with trigeminal neuralgia present in their 50s or 60s, they typically have a greater than 10-year life expectancy. Over the years, it is not uncommon for a patient’s trigeminal neuralgia to become refractory to their medications. Those with medically refractory trigeminal neuralgia go on to neurosurgical treatment. One of the major causes of trigeminal neuralgia is compression of the nerve by a vascular structure. The first microvascular decompression was described by Taarnhoj in 1952 and refined by Janetta3–5; this procedure treats the causal agent of trigeminal neuralgia. Ablative neurosurgical procedures performed through percutaneous techniques (e.g., glycerol injection, thermocoagulation, radiofrequency rhizotomy) produce a partial lesion of the trigeminal nerve and may afford pain relief. The concept of stereotactic radiosurgery for trigeminal neuralgia was introduced as a minimally invasive option, but this approach necessitates a trigeminal nerve lesion to some degree.
Historical Perspective of Gamma Knife in Trigeminal Neuralgia
The initial interest in Gamma Knife radiosurgery for trigeminal neuralgia arose from Lars Leksell’s interest in using radiosurgery for the treatment of pain syndromes.6 Twenty years before building the Gamma Knife, Leksell used an orthovoltage stereotactic technique to treat patients with trigeminal neuralgia and achieved some degree of relief of symptoms.7
Leksell also described gamma thalamotomies, which were used not only for tremor but also for intractable pain.8 The gasserian ganglion was irradiated for trigeminal neuralgia, and gamma capsulotomies were performed to interrupt frontolimbic connections in the treatment of intractable anxiety and obsessive-compulsive disorders.9,10 Leksell’s first patient was treated through an x-ray tube attached to a stereotactically centered device, and, in some patients, Leksell achieved pain relief for up to 17 years after treatment. The major challenge in targeting trigeminal neuralgia at that time was the limited visualization of the gasserian ganglion on plain x-rays. This hurdle, combined with the introduction of new drugs and the emergence of nonablative methods, caused a decline in the use of Gamma Knife for trigeminal neuralgia through the 1970s and early 1980s. However, with the introduction of high-quality magnetic resonance imaging (MRI), which permitted high-resolution imaging of the trigeminal nerve and root entry zone, interest began to increase again.
Rationale for Radiosurgery in Trigeminal Neuralgia and Factors Related to Successful Treatment
As early as 1941, Olivecrona understood (and described) that mechanical pressure along the root or at the level of the gasserian ganglion could be the cause of trigeminal neuralgia.11 In their pioneering work, Granit, Leksell, and Skoglund (1944) demonstrated that local pressure on nerve fibers could result in painful afferent discharges from the injured neural segment,12 evidence that has been supported by more contemporary work from Jannetta and colleagues, who have suggested that vascular compression of the trigeminal nerve may be a causal agent in trigeminal neuralgia.5,13,14 Despite these hypotheses, however, the fact that balloon compression of the trigeminal nerve can lead to symptomatic improvement in some patients with trigeminal neuralgia underscores the void in our understanding of the pathophysiology of this disease entity.15,16
Radiosurgery appears to be more effective when used as the initial modality than as a salvage treatment for patients with trigeminal neuralgia. Maesawa and coworkers17 demonstrated that patients who underwent radiosurgery following failed microsurgical decompression had high rates of recurrence, with only 60% of these patients maintaining complete pain relief at 1 year, a number that dropped to 53% at 2 years and 33% at 5 years. Régis and colleagues18 have reported that the probability of pain relief at 1 year in patients without previous surgery was 88%, compared with 82%, 80%, and 75% in patients with one, two, and three prior surgical interventions respectively.
In patients who have not undergone previous surgery for trigeminal neuralgia, patients who have contact between a blood vessel and the trigeminal nerve revealed by high-resolution MRI have a particularly favorable response to radiosurgery.19 In addition to these factors, Pollock and associates20 demonstrated that younger patient age and the length of the trigeminal nerve irradiated were related to improved radiosurgical outcomes (with patients who had longer segments radiated having improved outcomes). In contrast, Régis and associates21 noted that the probability of being pain free was lower in patients younger than 60 years of age (56% compared with 91%).
The presence of atypical facial pain (such as tingling or burning) has also been reported to have a poorer prognosis when radiosurgical treatment is used, with only 44% improvement of symptoms in this group, compared with 84% improvement in patients with typical pain according to Maesawa and colleagues.17 Atypical facial pain patients frequently represent a collection of patients with different types of underlying disease (e.g., postherpetic neuralgia, pain following sinus surgery, pain from facial trauma). The efficacy of Gamma Knife radiosurgery for relief of pain in atypical facial pain patients is not well defined by the literature; this is in part due to the heterogeneity of this patient population. Nevertheless, it is safe to conclude that the outcome of radiosurgical treatment for atypical facial pain patients is less favorable than for those with traditional trigeminal neuralgia.
Treatment with Gamma Knife radiosurgery in the setting of multiple sclerosis has been performed with lower rates of success according to some authors.18,22 Régis and associates18 found a trend toward treatment failure in cases of multiple sclerosis (42.9% compared with 12.8%; P = .07) when the minimal nerve dose was lower. In contrast, Rogers and coworkers23 achieved a high level of success in a study of 15 patients with multiple sclerosis undergoing Gamma Knife radiosurgery for trigeminal neuralgia. At a mean follow-up of 17 months, 80% of patients had experienced relief using an initial dose of 70 to 90 Gy. Five patients underwent repeat Gamma Knife radiosurgery to the same treatment area with a mean maximal dose of 48 Gy. All five patients attained some pain relief, and 60% were able to discontinue their trigeminal neuralgia pain medication.23 More investigation is required to assess the long-term success and toxicity (in particular the development of troublesome facial numbness) of Gamma Knife radiosurgery in multiple sclerosis patients.
Radiosurgical Targeting
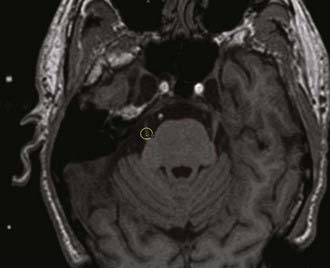
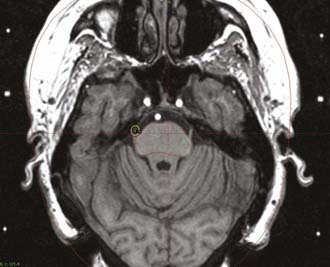
Accurate MRI is critical to the success of radiosurgical treatment. The trigeminal nerve is typically imaged using at least a 1.5-Tesla (T) MRI unit (Fig. 162-1); 3-T imaging during radiosurgery may offer improved resolution. Localization is performed using T1-weighted and fast spin echo T2-weighted axial images along with coronal images of the nerve (Fig. 162-2). The axial volume acquisition matrices are then divided into sections of 1 mm without gaps. In many centers, T1-weighted images are also repeated after administration of gadolinium. Three-dimensional reconstructions are also routinely performed (Fig. 162-3). When MRI is not feasible (i.e., in patients with pacemakers), computed tomography (CT) may be used for targeting, although this is not ideal. CT cisternography can be used to improve delineation of the radiosurgical target.
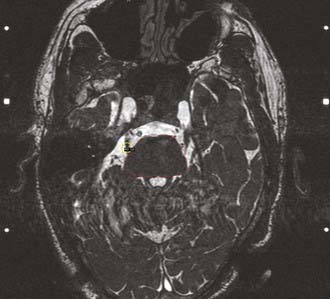
FIGURE 162-2 This is a constructive interference in steady state (CISS) sequence axial image of the same patient depicted in Figure 162-1. The brainstem is again contoured in red. CISS sequencing can be particularly useful in patients with prior open neurosurgical interventions around the area of the trigeminal nerve.
With radiosurgery, the usual target for treating trigeminal neuralgia is the trigeminal nerve root entry zone at the level of the pons. Varying lengths of the cisternal segment of the trigeminal nerve can affect radiosurgical targeting. Longer segments of the nerve allow for placement of a single isocenter with minimal to no blocking yet with still a tolerable dose delivered to the brainstem. A patient with a shorter trigeminal nerve cisternal segment may necessitate blocking or beam shaping to reduce dose to the brainstem (Fig. 162-4). Using a gamma angle of 110 degrees frequently facilitates alignment of the isocenter with the axis of the trigeminal nerve.
Much has been written about whether the trigeminal nerve should be targeted more proximally or distally.24–26 Régis and associates21 irradiated the cisternal (distal) portion of the trigeminal root and reported a high rate of effective pain control, with an 87% rate of excellent outcome and a 10% rate of painful relapse. This more anterior target choice showed fewer complications even with a maximal dose of 90 Gy. Nicol and associates27 and Pollock and coworkers20 targeted the trigeminal root entry zone with a dose of 90 Gy and found a higher rate of pain control, along with a higher rate of complications compared with when lower doses were given. Massager and colleagues26 obtained higher pain control rates using the plexus triangularis as the target. However, the length of the nerve targeted in this study was significantly increased when compared to other reports, and, as a result, the rate of trigeminal nerve injury (38%) was higher than that reported by Nicol27 and Pollock.20
Dose selection for trigeminal neuralgia has been studied extensively. Most centers use maximal doses of 70 to 85 Gy.28–33 Several authors have demonstrated a significant improvement in the rate of pain cessation and a reduction of recurrence rate when high maximal doses are used. Brisman and Mooij34 demonstrated that treatments in which the brainstem received 20% or more of the maximal dose to a volume of 20 mm3 provided better pain control than those targeting smaller regions with lower doses. When higher doses are required, the isocenter is usually placed away from the brainstem to avoid injury. Because doses greater than 90 Gy have been associated with an increased risk for postradiosurgical complications, most radiosurgical teams tend to limit the maximal dose to 90 Gy or less.33
Clinical Follow-Up
After radiosurgical treatment, clinical follow-up is critical. Generally, patients should be followed at 3- to 6-month intervals and new MRI studies obtained 6 to 9 months after surgery. In patients who have new neurological symptoms, an MRI can be performed earlier. In addition to imaging studies, follow-up examination should include a full neurological assessment and examination of cranial nerve function. The function of the trigeminal nerve in particular may have significant correlation to patient prognosis. Pollock and coworkers20 reported a strong correlation between the development of new facial sensory loss and achievement and maintenance of pain relief after radiosurgery, with patients harboring new trigeminal deficits being 4.5 times more likely to have excellent pain relief, compared with patients who have normal postradiosurgical trigeminal nerve function. Experimental models of radiosurgical treatment have confirmed that the etiology for this may lie in a nonselective destruction of myelinated and unmyelinated sensory fibers, including afferent nociceptive fibers.35
Some have suggested that postradiosurgical enhancement of the trigeminal nerve on MRI may correlate with the radiation dose used and thus may be related to the accuracy of targeting.36 In clinical practice, however, trigeminal nerve enhancement has not correlated with improved clinical outcomes.37
Pain Control After Radiosurgery for Trigeminal Neuralgia: A Review of the Literature
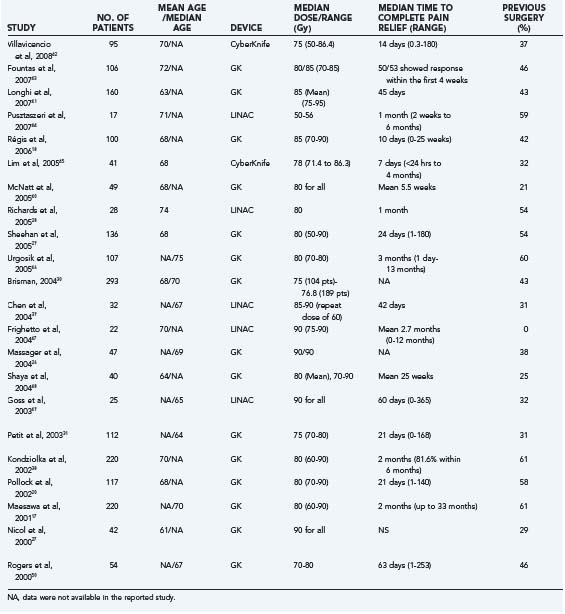
Although the neurosurgical treatment of choice for trigeminal neuralgia remains microvascular decompression, Gamma Knife surgery offers a reasonable alternative in patients who are unwilling to undergo surgery or who are not surgical candidates. A summary of major series on stereotactic radiosurgery for trigeminal neuralgia is presented in Table 162-1.17,18,20,26–31,38–50 Because of variations in data presentation, not all data are available for every series; however, every effort has been made to present a homogenous data set to allow direct comparison from a wide variety of studies. Régis and colleagues18 achieved a high rate of initial pain control with 94% of patients having either excellent or good response within 10 days. Pollock and associates20 showed that 75% of patients experienced complete pain relief at some point after radiosurgery.
Because the effects of radiation are dependent on both acute and delayed changes in the target tissue, there is a latency interval for the expected response, as in all radiosurgical procedures.51 In all of the series presented in Table 162-1, pain relief was typically achieved within the first several weeks after the procedure. Fountas and colleagues43 reported that most patients with no previous surgeries responded within 4 weeks after treatment. Pollock and associates20 found a comparable mean latency period of about 3 weeks. In other large series, however, the latency has been noted to be as long as 8 weeks after radiosurgery.17
According to the University of Pittsburgh group,17 most patients responded to Gamma Knife radiosurgery within 6 months of treatment, with a median time of 2 months to achieve 50% pain relief. Complete pain relief was achieved by 48%, with 82% of patients achieving some pain relief 6 months after treatment. Another 10% of patients achieved pain relief later, ranging from 6 to 33 months after radiosurgery. However, even these patients obtained partial pain relief within 6 months. These findings appear to indicate that many patients with partial pain relief initially will continue to have improvements in pain control. The 15% of patients who did not achieve pain control in 1 year did not achieve clinical improvement after radiosurgery, indicating that 1 year may be the optimal time to judge the true effectiveness of radiosurgery in trigeminal neuralgia patients.
From 1996 to 2003, 151 cases of trigeminal neuralgia were treated with the Gamma Knife at the University of Virginia and had evaluable follow-up.29 Radiosurgery was performed once in 136 patients, twice in 14 patients, and 3 times in 1 patient. One hundred twenty-two patients had typical trigeminal neuralgia, 3 with atypical trigeminal neuralgia, 4 with multiple sclerosis–associated trigeminal neuralgia, and 7 with trigeminal neuralgia and a history of a cavernous sinus tumor. In each case, the chosen radiosurgical target was located 2 to 4 mm anterior to the entry of the trigeminal nerve into the pons. The maximal radiation doses ranged from 50 to 90 Gy. The mean time to relief of pain was 24 days (range, 1 to 180 days). Forty-seven percent, 45%, and 34% of patients were pain free without medication at the 1-, 2-, and 3-year follow-ups, respectively. Ninety percent, 77%, and 70% of patients experienced some improvement in pain at the 1-, 2-, and 3-year follow-ups, respectively. Twelve patients (9%) suffered the onset of new facial numbness after treatment.
The pain from trigeminal neuralgia can be debilitating to those affected, and pain control itself may not be the only quality-of-life (QOL) measure that is related to patient outcomes. Petit and colleagues31 investigated QOL associated with Gamma Knife radiosurgery for trigeminal neuralgia. Even with partial pain relief, patients reported a median 80% improvement in QOL, with 65% believing that their surgery was successful. Patients with pain relief that was maintained at the time of analysis reported a median 100% improvement in their QOL, with a 100% success rate. Even the patients with temporary treatment responses (pain recurrence after a median of 8.5 months) described a median 80% improvement in QOL with an associated 60% of treatment success. These findings suggest that temporary pain relief, coupled with a low incidence of treatment morbidity, is a worthwhile treatment outcome for most patients.
Recurrence and Retreatment
Reported rates of recurrence following radiosurgery for trigeminal neuralgia have ranged from 5% to 42%, and recurrence is likely related to incomplete radiation effects on the targeted tissues.1,2,17,20,21,26,27,33,34,37,52–58 Maesawa and colleagues17 demonstrated that 71% of patients achieved or maintained complete or greater than 50% relief at 2 years, whereas 56% maintained the relief 5 years. Because of the relatively favorable risk-benefit profile of radiosurgery treatment in trigeminal neuralgia, some patients with recurrent symptoms may benefit from retreatment. Pollock and associates22 and Maesawa and colleagues17 recommend retreatment with radiosurgery in patients if they achieved a significant reduction in pain after initial Gamma Knife treatment. Eight of 10 patients in the initial study by Pollock and coworkers59 were pain free after initial radiosurgery and all these patients achieved complete pain relief with repeat Gamma Knife. These findings suggest that the response to initial Gamma Knife radiosurgery may be used by physicians to predict the response to repeat radiosurgery. Others have suggested that patients who have longer remission after radiosurgery tend to be more successful when retreated.60
Which regions to target during retreatment is a controversial subject. Generally speaking, retreatment involves the delivery of radiation at or near the previously treated site, although the target at retreatment usually is more anterior than that of an initial treatment. Shetter and colleagues61 and Pollock and coworkers22 have reported using a single 4-mm collimator shot targeted in the trigeminal nerve at its juncture with the brainstem, whereas Hasegawa and associates62 positioned a single 4-mm collimator anterior to the portion of the trigeminal nerve originally targeted so that there was a 50% overlap in the two radiosurgical volumes (compared with 100% overlap in most other studies). The rationale for this strategy is to reduce the radiation dose to the brainstem while increasing the dose to the length of trigeminal nerve root. Ultimately, a prospective dose planning study will be required to determine which technique is the best.
In our experience, the side effects of repeat Gamma Knife treatment are low, and new facial numbness is the most common complication reported. New or worsened facial numbness can be found in 11% to 70% of patients after second treatment.1,17,18 The overall effectiveness of repeat radiosurgical treatment is similar to the efficacy of the initial procedure, with rates of complete or partial pain relief ranging from 78% to 85%,22,27,62 although fewer retreatment patients achieve enough relief to completely discontinue their pain medications. Many contributing factors have been suggested for this, including patient factors, more conservative dosimetry when planning repeat radiosurgery, and a more severe form of the disease.62
Complications from Radiosurgery
Although stereotactic radiosurgery is not associated with some of the immediate risks of open surgical procedures, it nonetheless has risks. Potential complications associated with radiosurgery include radiation-induced parenchymal changes (some of which are reversible and others irreversible), radiation-induced neoplasia, and vascular injury.63,64 A noteworthy complication in the treatment of trigeminal pain is facial numbness or dysesthesias (anesthesia dolorosa). The incidence of new trigeminal dysfunction varies from 6% to 66%.24,29,31–33 Pollock and coworkers33 reported an association between higher radiation doses and the risk for trigeminal nerve dysfunction. In that study, 54% of patients treated with 90 Gy experienced facial numbness, whereas only 15% of patients treated with 70 Gy experienced a similar problem. In our series, 12 of 136 patients (9%) developed new facial numbness after Gamma Knife surgery. In our study, only 1 patient received a dose of 90 Gy, and no facial numbness was noted in this case. Cases of anesthesia dolorosa and absence of the corneal reflex after radiosurgery are rare. Repeat Gamma Knife surgery was associated with an increased risk for facial numbness, whereas 7% of patients who had only one Gamma Knife surgery developed new facial numbness (P = .002, t-test).29 In a series of 18 patients who underwent repeat radiosurgery, Herman and colleagues60 noted an 11% incidence of new or worsened facial numbness, which was not substantially elevated over the risk for facial numbness in those having only one Gamma Knife surgery. However, Hasegawa and associates62 and Shetter and colleagues61 noted an increased risk for facial numbness associated with repeat Gamma Knife surgery.
Comparison of Radiosurgery and Open Surgery for Trigeminal Neuralgia
Microvascular decompression (MVD) is the only treatment modality for trigeminal neuralgia that addresses the underlying pathophysiology of the disease, making it the well-established “gold standard.” Barker and colleagues5 reported that 70% of patients who underwent MVD had complete pain relief 10 years after surgery. Although this type of follow-up is lacking in the radiosurgical literature, in patients without previous surgery, Pollock and coworkers65 observed a rate of complete pain relief of 67% at 1 and 3 years, whereas Maesawa and colleagues17 observed a rate of complete pain relief of 70% at 9 months and 5 years. Given these results, radiosurgery as a primary treatment appears to provide a comparable rate of pain control to that of open surgery.
The major disadvantages of radiosurgical treatment are the high rate of recurrence and the delay in onset of pain relief. As described earlier only 27% of patients in the Pollock series65 were pain free without medication at the time of most recent follow-up. This, combined with the fact that no long-term data greater than 5 years are available in any radiosurgical series, confirms that MVD should (at least for now) remain the first-line treatment for patients who can tolerate the operation because of the durability of pain relief. In patients who cannot tolerate a surgical procedure, those in whom a vascular etiology cannot be identified as the cause of symptoms, and those unwilling to undergo an open surgery, radiosurgery is an appropriate alternative. The risks of repeat MVD are also known to be significantly higher than after the first surgery,5 and thus patients who have recurrence following failed MVD may also be considered candidates for radiosurgery, albeit with a lower chance of successful remission.
Brisman R. Gamma Knife surgery with a dose of 75 to 76.8 Gray for trigeminal neuralgia. J Neurosurg. 2004;100:848-854.
Brisman R, Khandji AG, Mooij RB. Trigeminal nerve-blood vessel relationship as revealed by high-resolution magnetic resonance imaging and its effect on pain relief after Gamma Knife radiosurgery for trigeminal neuralgia. Neurosurgery. 2002;50:1261-1266.
Brisman R, Mooij R. Gamma knife radiosurgery for trigeminal neuralgia: dose-volume histograms of the brainstem and trigeminal nerve. J Neurosurg. 2000;93(suppl 3):155-158.
Eller JL, Raslan AM, Burchiel KJ. Trigeminal neuralgia: definition and classification. Neurosurg Focus. 2005;18:E3.
Hasegawa T, Kondziolka D, Spiro R, et al. Repeat radiosurgery for refractory trigeminal neuralgia. Neurosurgery. 2002;50:494-500.
Kondziolka D, Lacomis D, Niranjan A, et al. Histological effects of trigeminal nerve radiosurgery in a primate model: implications for trigeminal neuralgia radiosurgery. Neurosurgery. 2000;46:971-976.
Kondziolka D, Lunsford LD, Flickinger JC, et al. Stereotactic radiosurgery for trigeminal neuralgia: a multiinstitutional study using the gamma unit. J Neurosurg. 1996;84:940-945.
Maesawa S, Salame C, Flickinger JC, et al. Clinical outcomes after stereotactic radiosurgery for idiopathic trigeminal neuralgia. J Neurosurg. 2001;94:4-20.
Massager N, Lorenzoni J, Devriendt D, et al. Gamma knife surgery for idiopathic trigeminal neuralgia performed using a far-anterior cisternal target and a high dose of radiation. J Neurosurg. 2004;100:597-605.
Merrison AF, Fuller G. Treatment options for trigeminal neuralgia. BMJ. 2003;327:1360-1361.
Nicol B, Regine WF, Courtney C, et al. Gamma knife radiosurgery using 90 Gy for trigeminal neuralgia. J Neurosurg. 2000;93(suppl 3):152-154.
Petit JH, Herman JM, Nagda S, et al. Radiosurgical treatment of trigeminal neuralgia: evaluating quality of life and treatment outcomes. Int J Radiat Oncol Biol Phys. 2003;56:1147-1153.
Pollock BE, Foote RL, Stafford SL, et al. Results of repeated Gamma Knife radiosurgery for medically unresponsive trigeminal neuralgia. J Neurosurg. 2000;93(suppl 3):162-164.
Pollock BE, Phuong LK, Foote RL, et al. High-dose trigeminal neuralgia radiosurgery associated with increased risk of trigeminal nerve dysfunction. Neurosurgery. 2001;49:58-62.
Pollock BE, Phuong LK, Gorman DA, et al. Stereotactic radiosurgery for idiopathic trigeminal neuralgia. J Neurosurg. 2002;97:347-353.
Régis J, Bartolomei F, Metellus P, et al. Radiosurgery for trigeminal neuralgia and epilepsy. Neurosurg Clin N Am. 1999;10:359-377.
Régis J, Metellus P, Hayashi M, et al. Prospective controlled trial of gamma knife surgery for essential trigeminal neuralgia. J Neurosurg. 2006;104:913-924.
Richards GM, Bradley KA, Tomé WA, et al. Linear accelerator radiosurgery for trigeminal neuralgia. Neurosurgery. 2005;57:1193-1200.
Rogers CL, Shetter AG, Fiedler JA, et al. Gamma knife radiosurgery for trigeminal neuralgia: the initial experience of The Barrow Neurological Institute. Int J Radiat Oncol Biol Phys. 2000;47:1013-1019.
Rogers CL, Shetter AG, Ponce FA, et al. Gamma knife radiosurgery for trigeminal neuralgia associated with multiple sclerosis. J Neurosurg. 2002;97(suppl 5):529-532.
Shaya M, Jawahar A, Caldito G, et al. Gamma knife radiosurgery for trigeminal neuralgia: a study of predictors of success, efficacy, safety, and outcome at LSUHSC. Surg Neurol. 2004;61:529-534.
Sheehan J, Pan HC, Stroila M, Steiner L. Gamma knife surgery for trigeminal neuralgia: outcomes and prognostic factors. J Neurosurg. 2005;102:434-441.
Tawk RG, Duffy-Fronckowiak M, Scott BE, et al. Stereotactic Gamma Knife surgery for trigeminal neuralgia: detailed analysis of treatment response. J Neurosurg. 2005;102:442-449.
Zhang P, Brisman R, Choi J, Li X. Where to locate the isocenter? The treatment strategy for repeat trigeminal neuralgia radiosurgery. Int J Radiat Oncol Biol Phys. 2005;62:38-43.
1 Merrison AF, Fuller G. Treatment options for trigeminal neuralgia. BMJ. 2003;327:1360-1361.
2 Eller JL, Raslan AM, Burchiel KJ. Trigeminal neuralgia: definition and classification. Neurosurg Focus. 2005;18:E3.
3 Taarnhoj P. Decompression of the trigeminal root and the posterior part of the ganglion as treatment in trigeminal neuralgia; preliminary communication. J Neurosurg. 1952;9:288-290.
4 Taarnhoj P. (A new operation for trigeminus neuralgia; decompression of the trigeminal root and the posterior part of the ganglion; preliminary report.). Nord Med. 1952;47:360-364.
5 Barker FG2nd, Jannetta PJ, Bissonette DJ, et al. The long-term outcome of microvascular decompression for trigeminal neuralgia. N Engl J Med. 1996;334:1077-1083.
6 Steiner L, Forster D, Backlund E-O, Steiner L, editors. Radiosurgery: Baseline and Trends. New York: Raven. 1992:263-292.
7 Leksell L. Brain fragments in radiosurgery. In: Steiner L., editor. Radiosurgery: Baseline and Trends. New York: Raven Press; 1992:623-692.
8 Steiner L, Forster D, Leksell L, et al. Gammathalamotomy in intractable pain. Acta Neurochir (Wien). 1980;52(3-4):173-184.
9 Rylander G. Stereotactic radiosurgery in anxiety and obsessive-compulsive neurosis. In: Hitchcock E, Ballantine HT, Meyerson BA, editors. Modern Concepts in Psychiatric Surgery. Amsterdam: Elsevier/North-Holland Biomedical Press, 1979.
10 Mindus P. Capsulotomy in anxiety disorders, a multidiscipline study, in Neurosurgery. Stockholm: Karolinska Institute; 1991.
11 Olivecrona H. Die Trigeminusneuralgie und ihre Behandlung, 14. Berlin: Nervenarzt. 1941. 49-57
12 Granit R, Leksell L, Skoglund CR. Fibre interaction in injured or compressed region of nerve. Brain. 1944;67:125-140.
13 Lovely TJ, Jannetta PJ. Microvascular decompression for trigeminal neuralgia. Surgical technique and long-term results. Neurosurg Clin N Am. 1997;8:11-29.
14 Jannetta PJ. Arterial compression of the trigeminal nerve at the pons in patients with trigeminal neuralgia. J Neurosurg. 1967;26(suppl):159-162.
15 Brown JA, Chittum CJ, Sabol D, et al. Percutaneous balloon compression of the trigeminal nerve for treatment of trigeminal neuralgia. Neurosurg Focus. 1996;1:e4.
16 Brown JA, Gouda JJ. Percutaneous balloon compression of the trigeminal nerve. Neurosurg Clin N Am. 1997;8:53-62.
17 Maesawa S, Salame C, Flickinger JC, et al. Clinical outcomes after stereotactic radiosurgery for idiopathic trigeminal neuralgia. J Neurosurg. 2001;94:14-20.
18 Régis J, Metellus P, Hayashi M, et al. Prospective controlled trial of Gamma Knife surgery for essential trigeminal neuralgia. J Neurosurg. 2006;104:913-924.
19 Brisman R, Khandji AG, Mooij RB. Trigeminal nerve-blood vessel relationship as revealed by high-resolution magnetic resonance imaging and its effect on pain relief after Gamma Knife radiosurgery for trigeminal neuralgia. Neurosurgery. 2002;50:1261-1266. discussion 1266-1267
20 Pollock BE, Phuong LK, Gorman DA, et al. Stereotactic radiosurgery for idiopathic trigeminal neuralgia. J Neurosurg. 2002;97:347-353.
21 Régis J, Bartolomei F, Metellus P, et al. Radiosurgery for trigeminal neuralgia and epilepsy. Neurosurg Clin N Am. 1999;10:359-377.
22 Pollock BE, Foote RL, Stafford SL, et al. Results of repeated gamma knife radiosurgery for medically unresponsive trigeminal neuralgia. J Neurosurg. 2000;93(suppl 3):162-164.
23 Rogers CL, Shetter AG, Ponce FA, et al. Gamma knife radiosurgery for trigeminal neuralgia associated with multiple sclerosis. J Neurosurg. 2002;97(suppl 5):529-532.
24 Kondziolka D, Lunsford LD, Flickinger JC, et al. Stereotactic radiosurgery for trigeminal neuralgia: a multiinstitutional study using the gamma unit. J Neurosurg. 1996;84:940-945.
25 Zhang P, Brisman R, Choi J, Li X. Where to locate the isocenter? The treatment strategy for repeat trigeminal neuralgia radiosurgery. Int J Radiat Oncol Biol Phys. 2005;62:38-43.
26 Massager N, Lorenzoni J, Devriendt D, et al. Gamma knife surgery for idiopathic trigeminal neuralgia performed using a far-anterior cisternal target and a high dose of radiation. J Neurosurg. 2004;100:597-605.
27 Nicol B, Regine WF, Courtney C, et al. Gamma knife radiosurgery using 90 Gy for trigeminal neuralgia. J Neurosurg. 2000;93(suppl 3):152-154.
28 Richards GM, Bradley KA, Tomé WA, et al. Linear accelerator radiosurgery for trigeminal neuralgia. Neurosurgery. 2005;57:1193-1200.
29 Sheehan J, Pan HC, Stroila M, et al. Gamma knife surgery for trigeminal neuralgia: outcomes and prognostic factors. J Neurosurg. 2005;102:434-441.
30 Brisman R. Gamma knife surgery with a dose of 75 to 76.8 Gray for trigeminal neuralgia. J Neurosurg. 2004;100:848-854.
31 Petit JH, Herman JM, Nagda S, et al. Radiosurgical treatment of trigeminal neuralgia: evaluating quality of life and treatment outcomes. Int J Radiat Oncol Biol Phys. 2003;56:1147-1153.
32 Tawk RG, Duffy-Fronckowiak M, Scott BE, et al. Stereotactic Gamma Knife surgery for trigeminal neuralgia: detailed analysis of treatment response. J Neurosurg. 2005;102:442-449.
33 Pollock BE, Phuong LK, Foote RL, et al. High-dose trigeminal neuralgia radiosurgery associated with increased risk of trigeminal nerve dysfunction. Neurosurgery. 2001;49:58-62.
34 Brisman R, Mooij R. Gamma knife radiosurgery for trigeminal neuralgia: dose-volume histograms of the brainstem and trigeminal nerve. J Neurosurg. 2000;93(suppl 3):155-158.
35 Kondziolka D, Lacomis D, Niranjan A, et al. Histological effects of trigeminal nerve radiosurgery in a primate model: implications for trigeminal neuralgia radiosurgery. Neurosurgery. 2000;46:971-976.
36 Alberico RA, Fenstermaker RA, Lobel J. Focal enhancement of cranial nerve V after radiosurgery with the Leksell Gamma Knife: experience in 15 patients with medically refractory trigeminal neuralgia. AJNR Am J Neuroradiol. 2001;22:1944-1948.
37 Massager N, Abeloos L, Devriendt D, et al. Clinical evaluation of targeting accuracy of Gamma Knife radiosurgery in trigeminal neuralgia. Int J Radiat Oncol Biol Phys. 2007;69:1514-1520.
38 Kondziolka D, Lunsford LD, Flickinger JC. Stereotactic radiosurgery for the treatment of trigeminal neuralgia. Clin J Pain. 2002;18:42-47.
39 Chen JC, Girvigian M, Greathouse H, et al. Treatment of trigeminal neuralgia with linear accelerator radiosurgery: initial results. J Neurosurg. 2004;101(suppl 3):346-350.
40 McNatt SA, Yu C, Giannotta SL, et al. Gamma knife radiosurgery for trigeminal neuralgia. Neurosurgery. 2005;56:1295-1301.
41 Longhi M, Rizzo P, Nicolato A, et al. Gamma knife radiosurgery for trigeminal neuralgia: results and potentially predictive parameters. Part I: Idiopathic trigeminal neuralgia. Neurosurgery. 2007;61:1254-1260.
42 Villavicencio AT, Lim M, Burneikiene S, et al. Cyberknife radiosurgery for trigeminal neuralgia treatment: a preliminary multicenter experience. Neurosurgery. 2008;62:647-655.
43 Fountas KN, Smith JR, Lee GP, et al. Gamma Knife stereotactic radiosurgical treatment of idiopathic trigeminal neuralgia: long-term outcome and complications. Neurosurg Focus. 2007;23:E8.
44 Pusztaszeri M, Villemure J, Regli L, et al. Radiosurgery for trigeminal neuralgia using a linear accelerator with BrainLab system: report on initial experience in Lausanne, Switzerland. Swiss Med Wkly. 2007;137:682-686.
45 Lim M, Villavicencio AT, Burneikiene S, et al. CyberKnife radiosurgery for idiopathic trigeminal neuralgia. Neurosurg Focus. 2005;18:E9.
46 Urgosik D, Liscak R, Novotny JJr, et al. Treatment of essential trigeminal neuralgia with Gamma Knife surgery. J Neurosurg. 2005;102(suppl):29-33.
47 Frighetto L, DeSalles A, Smith ZA, et al. Noninvasive linear accelerator radiosurgery as the primary treatment for trigeminal neuralgia. Neurology. 2004;62:660-662.
48 Shaya M, Jawahar A, Caldito G, et al. Gamma knife radiosurgery for trigeminal neuralgia: a study of predictors of success, efficacy, safety, and outcome at LSUHSC. Surg Neurol. 2004;61:529-534.
49 Goss BW, Frighetto L, DeSalles AA, et al. Linear accelerator radiosurgery using 90 gray for essential trigeminal neuralgia: results and dose volume histogram analysis. Neurosurgery. 2003;53:823-828.
50 Rogers CL, Shetter AG, Fiedler JA, et al. Gamma knife radiosurgery for trigeminal neuralgia: the initial experience of The Barrow Neurological Institute. Int J Radiat Oncol Biol Phys. 2000;47:1013-1019.
51 Jagannathan J, Sherman JH, Mehta GU, Chin LS. Radiobiology of brain metastasis: applications in stereotactic radiosurgery. Neurosurg Focus. 2007;22:E4.
52 Flannery TW, Suntharalingam M, Kwok Y, et al. Gamma knife stereotactic radiosurgery for synchronous versus metachronous solitary brain metastases from non-small cell lung cancer. Lung Cancer. 2003;42:327-333.
53 Levivier M, Lorenzoni J, Massager N, et al. Use of the Leksell Gamma Knife C with automatic positioning system for the treatment of meningioma and vestibular schwannoma. Neurosurg Focus. 2003;14:e8.
54 Levivier M, Massager N, Wikler D, et al. Use of stereotactic PET images in dosimetry planning of radiosurgery for brain tumors: clinical experience and proposed classification. J Nucl Med. 2004;45:1146-1154.
55 Levivier M, Wikler DJr, Massager N, et al. The integration of metabolic imaging in stereotactic procedures including radiosurgery: a review. J Neurosurg. 2002;97(suppl 5):542-550.
56 Lorenzoni J, Devriendt D, Massager N, et al. Radiosurgery for treatment of brain metastases: estimation of patient eligibility using three stratification systems. Int J Radiat Oncol Biol Phys. 2004;60:218-224.
57 Lorenzoni JG, Massager N, David P, et al. Neurovascular compression anatomy and pain outcome in patients with classic trigeminal neuralgia treated by radiosurgery. Neurosurgery. 2008;62:368-375.
58 Massager N, Lorenzoni J, Devriendt D, Levivier M. Radiosurgery for trigeminal neuralgia. Prog Neurol Surg. 2007;20:235-243.
59 Pollock BE, Foote RL, Link MJ, et al. Repeat radiosurgery for idiopathic trigeminal neuralgia. Int J Radiat Oncol Biol Phys. 2005;61:192-195.
60 Herman JM, Petit JH, Amin P, et al. Repeat Gamma Knife radiosurgery for refractory or recurrent trigeminal neuralgia: treatment outcomes and quality-of-life assessment. Int J Radiat Oncol Biol Phys. 2004;59:112-116.
61 Shetter AG, Rogers CL, Ponce F, et al. Gamma knife radiosurgery for recurrent trigeminal neuralgia. J Neurosurg. 2002;97(suppl 5):536-538.
62 Hasegawa T, Kondziolka D, Spiro R, et al. Repeat radiosurgery for refractory trigeminal neuralgia. Neurosurgery. 2002;50:494-500.
63 Lim YJ, Leem W, Park JT, et al. Cerebral infarction with ICA occlusion after Gamma Knife radiosurgery for pituitary adenoma: A case report. Stereotact Funct Neurosurg. 1999;72(suppl 1):32-39.
64 Ganz JC. Gamma knife radiosurgery and its possible relationship to malignancy: a review. J Neurosurg. 2002;97(suppl 5):644-652.
65 Pollock BE, Foote RL, Stafford SL. Stereotactic radiosurgery: the preferred management for patients with nonvestibular schwannomas? Int J Radiat Oncol Biol Phys. 2002;52:1002-1007.