Stellate ganglion block
Anatomy
The sympathetic chain lies along the anterolateral aspect of the vertebral bodies in a fascial space bounded posteriorly by the prevertebral muscles and in the cervical region anteriorly by the carotid sheath. The nerve fibers in the cervicothoracic chain originate from preganglionic sympathetic fibers from T1 to T6 and visceral afferent fibers from the head, neck, and upper extremity (see Chapter 40). These fibers are distributed to the brain, meninges, eye, ear, glands, skin, and vessels of the head, neck, upper extremity, and some thoracic viscera. The efferent and afferent fibers form several ganglia; the first thoracic and inferior cervical ganglia lie in close proximity and are often fused to form the stellate ganglion, which is oval and about 1 inch long by 0.5 inch wide. It lies within the fascial space described earlier. It is bounded posteriorly by the neck of the first rib and the transverse process of C7 and anteriorly by the dome of the pleura, the carotid sheath, and the vertebral artery. The medial boundary is the vertebral column. It is important to note that some thoracic preganglionic sympathetic fibers may bypass the stellate ganglion.
Technique
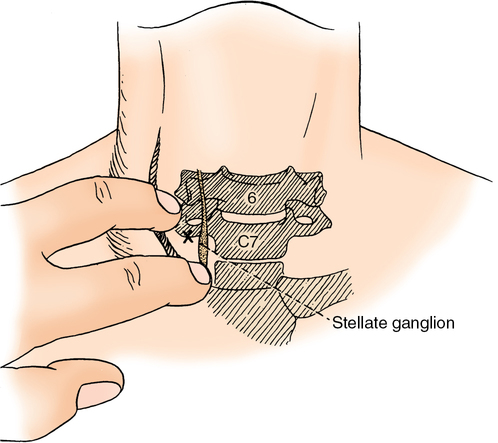
Although posterior and anterior approaches have been described, a paratracheal route is used most frequently. The patient is instructed to lie supine with the head supported by a pillow. The head is kept in the midline in slight extension. The patient’s mouth should be slightly open to relax the neck muscles. The stellate ganglion can be blocked at the level of C6 or C7, but, because of the risk of pleural puncture, the approach to the fascial space is often made slightly superior to the ganglion at the level of C6 (Chassaignac tubercle) (Figure 218-1). Two fingerbreadths (1.5-2 cm) above the clavicular head, the trachea, sternocleidomastoid muscle, and carotid sheath are palpated (approximately at the level of the cricoid cartilage). The anesthesia provider presses two fingers gently down onto the lateral edge of the transverse process of C6 (the most readily palpable cervical anterior tubercle) while simultaneously drawing the contents of the carotid sheath laterally (Figure 218-2). A 1.5-in to 3-in, 23-gauge or 25-gauge B (blunt) bevel needle is inserted just lateral to the trachea after skin infiltration with a local anesthetic agent. The transverse process of C6 should be encountered between the two palpating fingers at a depth of 1.5 to 2 cm. The needle is withdrawn 2 mm to place it in the correct fascial plane, and 8 to 10 mL of local anesthetic agent is injected incrementally after careful aspiration. A 0.5-mL test dose is recommended to rule out a vertebral artery injection. A generalized seizure can occur with as little as 0.5 mL of local anesthetic agent injected into the vertebral artery. If blockage of the sympathetic supply to the upper extremity is desired, the patient is placed in a 30-degree head-up position to encourage caudal diffusion of the local anesthetic agent to the upper thoracic ganglia. In addition, a larger volume of local anesthetic agent may be necessary. Position of the needle and spread of solution may be confirmed by fluoroscopy.
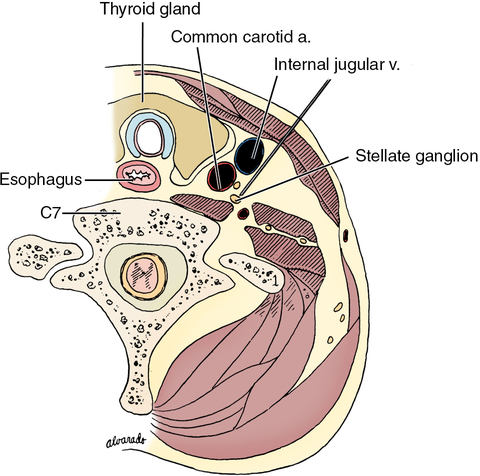
A large number of different types of nerve blocks, including stellate ganglion blocks, are being performed under ultrasound guidance to improve success of the block and to decrease complications. Real-time ultrasound of the neck can delineate the carotid artery, internal jugular vein, esophagus, thyroid, longus colli muscle, root of C6, and the transverse process of C6. The needle tip is directed to penetrate the prevertebral fascia covering the longus colli, and the injection is performed under direct ultrasound visualization. Signs of a successful stellate ganglion block and complications and side effects of a stellate ganglion block are outlined in Boxes 218-1 and 218-2, respectively.






