26 Stellate Block
Placement
Anatomy
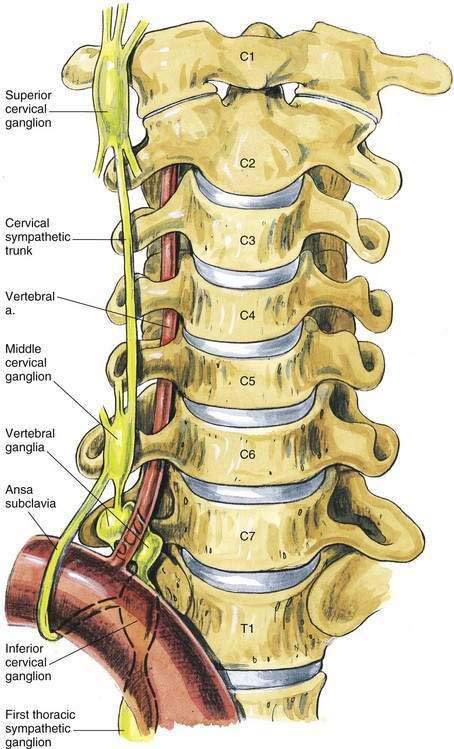
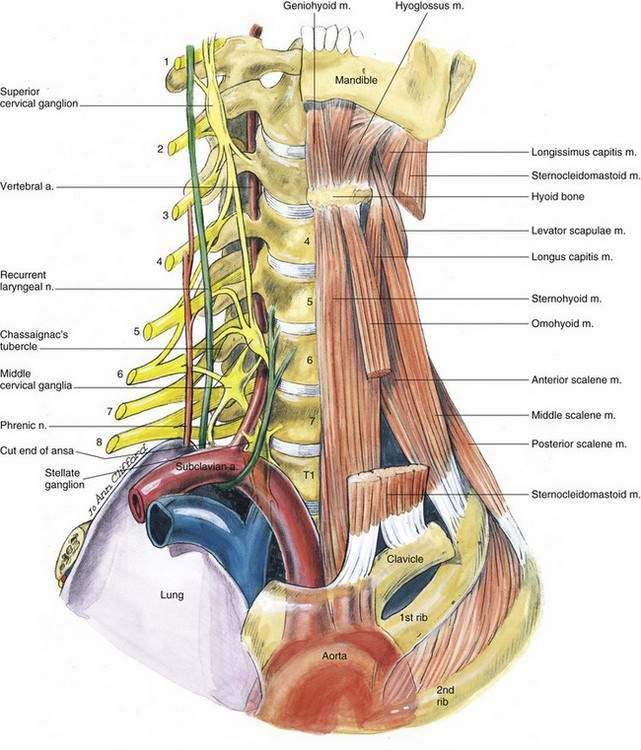
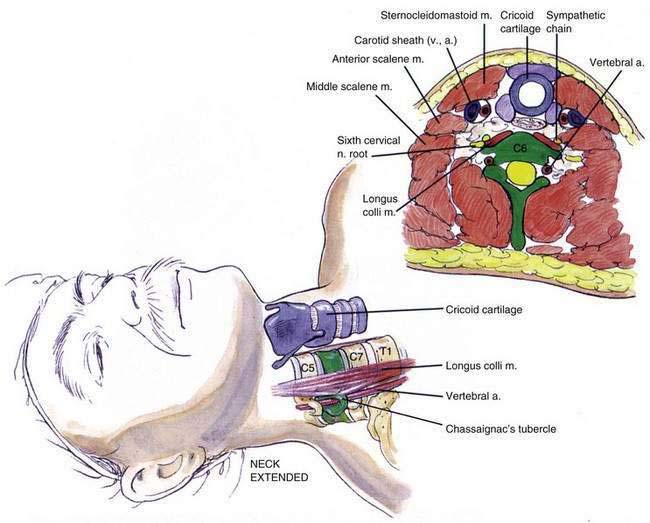
The cervical sympathetic trunk is a cephalad continuation of the thoracic sympathetic trunk. It is composed of three ganglia: the superior cervical ganglion, generally opposite the first cervical vertebra; the middle cervical ganglion, usually opposite the sixth cervical vertebra; and the stellate (cervicothoracic) ganglion, generally opposite the seventh cervical and first thoracic vertebrae near the head of the first rib. The stellate ganglion is a fusion of the inferior cervical ganglion and the first thoracic ganglion—hence the name cervicothoracic ganglion (Fig. 26-1). The cervical part of the sympathetic chain and ganglion lies on the anterior surface of, and is separated from, the transverse processes of the cervical vertebrae by the thin prevertebral musculature (primarily the longus colli muscle), as illustrated in Figure 26-2. Because the anterior approach to the stellate ganglion is often made at the level of the sixth cervical vertebral (Chassaignac’s) tubercle, it can be seen that the term stellate block is really a misnomer. To produce stellate (cervicothoracic) ganglion block, the anesthesiologist must rely on spread of the local anesthetic solution along the prevertebral muscles, or place the needle at the level of the seventh cervical vertebra with the use of ultrasonography or fluoroscopy.
Position
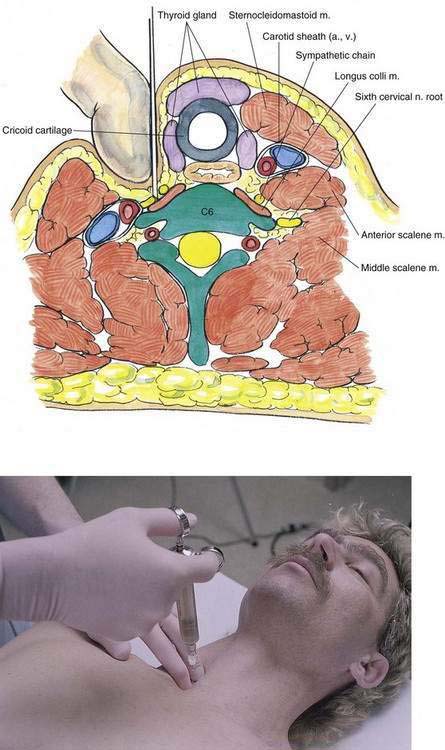
The patient should be in the supine position, with the neck in slight extension (Fig. 26-3). This is often facilitated by removing the patient’s pillow before positioning. The anesthesiologist should stand beside the patient’s neck and identify the sixth cervical vertebral tubercle with palpation. This can be accomplished by locating the cricoid cartilage and moving the fingers laterally until they contact this easily palpable vertebral tubercle.
Needle Puncture
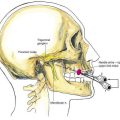
Once the sixth cervical vertebral tubercle is identified as shown in Figure 26-3, the anesthesiologist should place the index and third fingers between the carotid artery laterally and the trachea medially at the level of C6. A short, 22- or 25-gauge needle is inserted until it contacts the transverse process of C6. The needle is then withdrawn approximately 1 to 2 mm, and 5 to 10 mL of local anesthetic is injected (Fig. 26-4).
Potential Problems
As illustrated in Figure 26-2, the vertebral artery runs close to the transverse process of C6, and intravascular injection must be avoided. The recurrent laryngeal and phrenic nerves may also be blocked if the needle position is not ideal. Patients should be cautioned that they may experience a lump in the throat or a sense of dyspnea. Reassurance is usually all that is necessary.