CHAPTER 62 Standard Temporal Lobectomy
Historical Background
The standard temporal lobectomy developed concurrently with the identification of the temporal lobe epilepsy syndrome and the emergence of electroencephalography (EEG) in the 1940s and 1950s. Much of the credit belongs to Penfield and Jasper at the Montreal Neurological Institute (MNI).1 When Herbert Jasper joined the MNI in 1937, he brought the technique of EEG with him. By this time, Penfield and his partner William Cone had been performing surgery for epilepsy since Penfield arrived in 1928. As EEG became more established in the evaluation and diagnosis of focal epilepsy through the work of Jasper and Gibbs, the classification and study of temporal lobe epilepsies was under way. Through the close friendship of Jasper and Penfield, the MNI became a leader in the late 1930s in the surgical treatment of epilepsy. In 1941, Jasper and Kershman proposed a classification of epilepsy based on EEG waves.2 In this report, they described the localization of psychomotor phenomena from within the deep regions of the temporal lobe. Despite increasing awareness of the role of the mesial temporal lobe in these seizures, the lack of understanding about the function of this tissue and the inability of the surgeon to “see” the lesion at the time of resection led to reluctance on Penfield’s part to remove these structures.1 In 1950, Penfield reported his success in anterolateral temporal resections.3 In this series of 68 patients, 10 had partial removal of the uncus, and only 2 had hippocampal resections. EEG abnormalities were recorded from the temporal lobe in this group of patients, but an underlying substrate had not been identified. At the same time, Percival Bailey and Ernest Gibbs reported a series of 25 patients from the University of Illinois program who underwent temporal resection guided by EEG.4 Similar to Penfield’s series, these patients did not have hippocampal resections.
The second phase in the development of the modern surgical strategy to treat temporal lobe seizures took place in the 1950s as the role of the mesial temporal lobe structures in the pathogenesis of the epilepsy became better understood. This occurred as a number of scientists began to study the connections of the mesial temporal lobe to the rest of the brain and through the use of stimulation studies to reproduce seizure semiology in animals and humans.5–8 In 1952, Penfield and Baldwin published a classic monograph describing their technique for anterolateral temporal lobectomy including the hippocampus and amygdala.9 They reported that the most frequent pathologic abnormality in two of three of their cases was an atrophic lesion termed incisural sclerosis. Falconer in a report in 1953 recognized a connection with febrile seizures and introduced a modification allowing for en bloc resection of the hippocampus, which allowed the pathologists to study the tissue.10 With the advent of neuroimaging, modifications to the technique reported by Penfield have been made to address specific pathology seen preoperatively. Despite these modifications, the operation developed and introduced by innovative neurosurgeons in the early 20th century remains one of the most successful operations for the treatment of epilepsy today.
Identification of Surgical Candidates: The Concept of Pharmacoresistance and Medical Intractability
The indications for epilepsy surgery generally include the presence of focal epilepsy resistant to treatment with an adequate trial of anticonvulsant therapy. The precise definition of an adequate anticonvulsant trial is open to interpretation, but a study by Kwan and Brodie produced useful information regarding the efficacy of anticonvulsant therapy in newly diagnosed epilepsy.11 This study suggests that after three medications fail to control seizures, further success is unlikely, and other options should be considered. Consider also the paper by Wiebe and associates, comparing temporal lobectomy to optimal medical therapy in a group of patients with temporal lobe epilepsy.12 In this prospective randomized trial, surgical therapy in combination with medical therapy was far superior to ongoing medical therapy alone. These papers lend credence to the idea that patients with ongoing epilepsy despite a trial with a few anticonvulsants should be expeditiously evaluated for possible epilepsy surgery.
Preoperative Evaluation
Video Electroencephalography Monitoring
The diagnosis and type of epilepsy should be confirmed through prolonged video-scalp EEG monitoring in a dedicated epilepsy monitoring unit (EMU).13 Scalp EEG recording is a noninvasive monitoring technique that can sample extensive areas of the brain to give the best overview of the general distribution of interictal and ictal epileptic activities. It gives an excellent overview of the approximate location and extent of the epileptogenic area. Most epileptic patients with TLE (between 85% and 100%) show epileptiform discharges on their interictal scalp EEG recordings.14,15 Both the localization and pathologic type of the epileptogenic lesion within the temporal lobe affect the scalp localization (and lateralization) of interictal and ictal EEG patterns. In addition, video recordings and analyses permit the characterization of the seizure semiology that may be helpful in the localization and lateralization of the ictal onset zone.
Semiology and Electroencephalography Patterns in Mesial Temporal Lobe Epilepsy Due to Hippocampal Sclerosis or Mesial Temporal Mass Lesions (Neoplasms or Cavernomas)
Hippocampal sclerosis is one of the most common pathologic substrates in patients with TLE. Patients with mesial TLE show a characteristic electroclinical syndrome that typically consists of a rising abdominal sensation aura that may be followed by mouth and hand automatisms and possible ictal contralateral hand dystonic posturing. The presence of postictal speech difficulties may help in lateralizing the seizure onset zone to the dominant hemisphere for language. Patients with TLE due to hippocampal sclerosis show slowing in the ipsilateral temporal electrodes and interictal epileptic sharp waves that are usually mapped to the anterior temporal lobe.16 In addition, in less than 50% of these patients, sharp waves mapped to the contralateral anterior temporal lobe electrodes are found. Patients with mesial TLE due to amygdalohippocampal tumors or cavernomas are more likely to exhibit less localized sharp waves and less likely to have contralateral epileptiform abnormalities.
Semiology and Electroencephalography Patterns in Neocortical Temporal Lobe Epilepsy Due to Cortical Dysplasia or Temporal Mass Lesions (Neoplasms or Cavernomas)
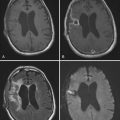
Imaging
Magnetic resonance imaging (MRI) of the brain, fluorodeoxyglucose (FDG) positron emission tomography (PET), ictal radionuclide blood flow studies (e.g., single-photon emission computed tomography [SPECT]), and functional MRI are the main neuroimaging tests that are used in the preoperative evaluation of patients with pharmacoresistant epilepsy that is suspected to arise from the temporal lobe. The typical MRI sequence involves thin-slice coronal T1-weighted imaging, fluid-attenuated inversion recovery (FLAIR) coronal sequences, and T2-weighted coronal sequences. Typical findings of mesial temporal sclerosis include atrophy of the affected hippocampus and increased signal intensity on the FLAIR and T2 sequences. One must always carefully study the remainder of the temporal lobe because dual pathology occurs in about 10% to 30% of mesial temporal sclerosis cases.17–19 Findings suggestive of dual pathology include blurring of the temporal pole gray-white interface or enlargement or distortion of the cortical ribbon. These are important findings that may influence the choice of surgical procedure.
The metabolism of the brain is studied with the use of interictal PET scanning. In this procedure, a radionuclide (18FDG) is injected, and computed tomography (CT) scanning is performed. This test gives the clinician a picture of how the brain takes up glucose. Originally designed for TLE, the test is said to be 70% specific when hypometabolism is seen in one of the temporal lobes.20
The localization of language is now possible by noninvasive functional MRI, which is slowly replacing the more invasive intracarotid sodium amobarbital testing. One possible advantage of the latter is the ability to test memory function at the same time, although recent reports suggest that cognitive functional MRI may offer an important, noninvasive, preoperative assessment of hippocampal memory function.21–23
Neuropsychological and Psychosocial Preoperative Evaluations
Neuropsychological testing and psychosocial and psychiatric evaluations are also completed during the initial work-up. Neuropsychological information is important because the temporal lobes play a role in emotion, language, and memory. In fact, patients with TLE are often aware of significant progressive memory and naming problems that lead them to pursue surgical intervention. Despite many years of experience in temporal lobe surgery, our understanding of function and prediction of neuropsychological deficits is still somewhat poor. During the preoperative evaluation of the TLE patient, it is important to gain a baseline measure of overall intellectual functioning as well as verbal and visual spatial memory scores. This is accomplished with standardized neuropsychological testing, which is then repeated 6 months after surgery. Preoperative and postoperative deficits in short-term memory and naming are common in patients with dominant (language-localized) TLE, and the risk for worsening must be discussed with the patient. This risk is dependent on baseline preoperative functioning and the individual substrate of the epilepsy (e.g., presence of mesial temporal sclerosis).24–26
Surgical Decision Making
For the TLE patient, decisions revolve around localizing the epilepsy to the lateral or mesial temporal lobe, the presence and nature of the epileptic lesion, and the presence of language or important short-term memory deficits. For the patient undergoing a standard temporal lobectomy, the epilepsy should be localized to the anteromesial temporal lobe, and ideally a well-defined lesion should be present (mesial temporal sclerosis, malformation of cortical development, neoplasm, cavernoma). The planned posterior extent of resection should not encroach on possible neocortical temporal lobe language areas. If the dominant temporal lobe is involved, a baseline memory or naming deficit in the presence of mesial temporal sclerosis would support the conclusion that the correct brain site was targeted, and the risk for causing further neurological deficits would be acceptably low.27,28
The anatomy of the temporal lobe deserves a brief discussion at this point. The temporal lobe has well-defined anterior, lateral, basal, and mesial surfaces. The posterior boundary is arbitrary, having no obvious anatomic demarcation separating it from the parietal area. The temporal lobe is made up of five gyri and their corresponding sulci. The lateral surface lies below the sylvian fissure and extends to the floor of the middle cranial fossa. The gyri from top to bottom include the superior temporal gyrus (T1), the middle temporal gyrus (T2), and the inferior temporal gyrus (T3), which often extends onto the basal surface. The basal surface includes the inferior temporal gyrus (T3), the fusiform gyrus, and the parahippocampal gyrus. The mesial surface includes the amygdala and the parahippocampal gyrus, including the uncus. The collateral sulcus separates the fusiform and parahippocampal gyri and serves as an important reference to locate the temporal horn of the ventricle. Within the temporal horn, important anatomic structures include the inferior choroidal point (anterior choroidal artery enters the choroid plexus here), the hippocampus occupying the mesiobasal portion of the ventricle, the fornix, the choroid plexus, the choroidal fissure, and the amygdala in the anterior-superior-medial portion of the ventricle. The reader is referred to an excellent series of articles describing in detail the temporal lobe anatomy.29
Functional anatomy in the temporal lobe includes comprehensive language cortex in the dominant temporal lobe, visual field fibers (Meyer’s loop) subserving the contralateral upper quadrantic visual field information, and potential important memory and naming centers. The anatomy of language cortex in the temporal lobe can be quite variable.30,31 Cortical stimulation testing can be performed to further identify and protect lateral language cortex when posterior temporal lobe resections are anticipated on the dominant side. This can be done either intraoperatively with the patient awake or extraoperatively with implanted electrodes. After the language cortex has been identified, the temporal resection can be tailored to the patient’s individual anatomy. The standard temporal lobectomy is designed to avoid temporal lobe cortical language sites by limiting the resection of the superior temporal gyrus to 3 to 4.5 cm from the anterior temporal pole. There is some controversy as to whether even this practice is safe, and some centers advocate leaving the entire superior temporal gyrus in place. This is based on language-stimulation data suggesting the presence of language sites in the anterior 3 cm of the superior temporal gyrus in a small percentage of patients.30 Of course, these sites were not resected, and thus it is difficult to know whether they were essential language sites. Other “nonessential” language sites in the temporal lobe have been demonstrated through cortical stimulation followed by resection.32 These sites were located in the basal temporal lobe by direct cortical stimulation but left no permanent language deficit after they were resected. Insufficient data, however, are available from the limited numbers of patients reported to conclude with certainty that no patient will develop a permanent language deficit after resection of a basal temporal language site.
Visual field fibers are also located in the temporal lobe as they extend forward from the lateral geniculate body before turning posterior on their way to calcarine cortex. These fibers are located unpredictably in the roof of the temporal horn, and standard temporal lobe resections cause injury to this fiber tract in as many as 50% of cases.33 This leads to the “pie in the sky” visual field deficit with loss of peripheral vision in the opposite upper quadrant. In most cases, the visual field defect noted with careful perimetry testing is not clinically significant.
Surgical Technique
When the decision has been made to perform a standard temporal lobectomy, the technique varies little from patient to patient. The word standard implies a reproducible operation from patient to patient and even surgeon to surgeon. It is best used to treat the “standard” syndrome of mesial TLE consisting of reproducible EEG, MRI, and seizure semiology elements. The targets of this operation are the mesial temporal lobe structures that are “sclerotic”: the parahippocampus, hippocampus, and amygdala. The exact posterior extent of resection of the hippocampus to improve outcomes is unknown, but at least one prospective trial correlated improved outcome with more aggressive resection of the hippocampus.34
Once positioned, the hair in the frontotemporal region is clipped, and a “reverse question mark” incision is made from just above the zygoma, extending back in the temporal region to the posterior part of the pinna and then curving anteriorly just above the insertion of the temporalis muscle. A larger skin flap is not necessary and may lead to increased risk for cosmetic deformity. The skin incision is carried out staying in the plane above the temporalis fascia. I (W.B.) prefer to split the fascia of the temporalis muscle and then elevate the muscle using a T incision based on the zygoma, with most of the muscle bulk reflected anteriorly.35 This approach is done with a scalpel to minimize shrinking of the muscle fibers and facilitates an easier reattachment of the muscle at the end of the procedure. One should also be careful to leave enough muscle cuff attached to the temporal bone to allow secure suturing of the muscle at closure. Despite all these efforts, a significant cosmetic deformity may occur from wasting of the temporalis muscle, and this should be discussed with the patient before surgery. At this stage, exposure of the temporal bone from the root of the zygoma to the anatomic “keyhole” should be visualized. The anterior aspect of the temporalis muscle is undermined with electrocautery in case the bone in the region of the sphenoid wing needs to be rongeured away to allow additional exposure of the temporal pole. In most cases, this additional removal of bone is unnecessary and further increases the chances of a cosmetic deformity after surgery.
Outcomes
After the surgery is completed, time must pass before determining outcome. Long-term seizure-free outcomes after temporal lobectomy, especially when performed for mesial temporal sclerosis, are often stated to be the best of all surgical procedures for medically resistant epilepsy. A number of long-term studies following patients for 5 to 10 years after surgery describe an initial seizure-free rate reaching 80%, which then noticeably declines over time to a 5-year seizure-free rate of about 50%.36–40 Factors predicting an unfavorable outcome may include the presence of epileptic activity on the 6-month postoperative EEG, frequent preoperative seizures, generalized motor seizures, bilateral MRI abnormalities, and increased epilepsy duration.36,41–43 Interestingly, in the report by Jeha in 2006, the presence of a normal MRI preoperatively did not lead to a worse outcome after surgery.36 This is in disagreement with other studies suggesting a worse outcome in the face of a normal preoperative MRI and would suggest that patients with well-localized nonlesional TLE should be considered for temporal lobectomy.40,44 Another important factor in the postoperative management of these patients is the “running-down” phenomenon described to occur in as many as one third of patients experiencing postoperative seizures after temporal lobectomy.43,45–47 In a recent study, the presence of rare postoperative seizures 6 months after surgery was observed in a group of patients who subsequently were documented to have long-term seizure freedom in 74% of cases.43 The authors hypothesized that the epileptogenic zone (EZ) in these patients was considerably reduced but not completely removed. The running-down theory implies that this greatly reduced EZ gradually loses the power to generate seizures or that the anticonvulsant medications are able to control them.
Outcome analysis is extremely important in this group of patients because questions regarding return to employment, driving, and cessation of medication hinge on the success of surgery. Concrete information regarding potential risks and benefits of anticonvulsant withdrawal are necessary to allow these patients to reintegrate into society safely without medications. The National Library of Medicine has indexed more than 4400 articles that focus on epilepsy surgery, and 75% of these were published after 1990.48 As Wiebe points out, the quality of these studies is reflected by the fact that only seven randomized controlled trials have been performed, and four of these involved the efficacy of vagus nerve stimulation.49–52 Two others compared different surgical procedures to treat temporal lobe epilepsy without medical controls, and the final study compared temporal lobectomy with medical treatment.12,34 Importantly, the results of the randomized trial by Wiebe in which 58% of surgically treated patients remained free of seizures appear comparable to the results of the systematic review of class IV nonrandomized studies involving 1952 patients.53 In this large review, overall 66% of patients remained seizure free after surgery.
Surgical Complications
The rate of significant complications after temporal lobectomy is fortunately quite low. In general, the neurosurgical risks that need to be discussed with the patient include the general risks of craniotomy and the more specific risks of manipulating the temporal lobe. General complications include infection (wound, craniotomy, meningitis, urine), hemorrhage (wound, epidural, subdural, intracerebral), red blood cell transfusion related to acute blood loss anemia, deep venous thrombosis, anesthetic complications, and death. The incidence of mortality after temporal lobectomy is approaching zero as experience and technology improves.12,53,54
Visual field loss after temporal lobectomy is related to injury of the geniculocalcarine fibers as they make their way from the lateral geniculate body to the occipital cortex. The most common pattern of injury results in a contralateral superior quadrantanopsia (“pie in the sky”) from damage to Meyer’s loop as it courses forward in the roof of the temporal horn of the lateral ventricle. Its variable course and lack of anatomic distinction at surgery make it a difficult structure to protect. The incidence of superior quadrantanopsia reported on retrospective studies is variable, but likely a realistic estimate is 35% to 50% after standard temporal lobectomy.33,55,56 Contralateral homonymous hemianopsia is much less common and usually results when larger temporal lobe resections are performed and damage to the geniculocalcarine tract occurs at the posterior aspect of the inferior temporal horn (trigone region). The optic tract can also be injured in the prethalamic region by dissections that stray too far superiorly at the level of the amygdala and anterior hippocampus. Finally, a contralateral hemianopsia may accompany a hemiparesis when damage to the anterior choroidal artery occurs in its cisternal segment. This artery is an important structure to protect during removal of the mesial structures. Respecting the anatomic landmarks during removal of the amygdala and hippocampus is the best way to avoid this potentially devastating complication. Hemiparesis may also result from manipulation or retraction injury of the ipsilateral cerebral peduncle. This type of postoperative deficit generally improves with time and is best avoided by limiting retraction during surgery on the roof of the temporal horn.
Postoperative aphasias can occur after dominant temporal lobe resections. These are generally characterized by perseveration, naming difficulties, paraphasias, and word substitutions. Fortunately, these are usually transient and peak 24 to 48 hours after surgery before resolution. Although the exact cause is unknown, this language disturbance can be quite severe when it occurs. Potential mechanisms include retraction and ischemic infarction of comprehensive language cortex and resection of anterior and basal temporal lobe language sites that ultimately are not essential language sites.32 Management of this complication should include postoperative MRI with stroke protocol, corticosteroid therapy, and speech therapy services. The patient and family should be reassured that language function will improve when the MRI does not demonstrate a posterior temporal lobe infarction. Strategies to avoid injury to the posterior temporal neocortex during surgery include minimizing retraction during removal of the posterior hippocampus and protecting the arterial and venous structures serving this area.
Cognitive Outcome and Quality of Life
Complaints centered on cognitive function are common in the temporal lobe epilepsy patient. Many patients have significant neuropsychological deficits before surgery thought to be related to damage to the mesial temporal lobe structures involved in memory as well as the effects of anticonvulsant therapy on normal cortical tissue. Preoperative and postoperative cognitive assessment is important to help counsel the patient on existing deficits and to predict and document the effects of temporal lobectomy on memory function. Preoperative risk factors for worsening memory function after surgery include dominant TLE, lack of hippocampal sclerosis, normal baseline neuropsychological function, and later age of onset of the epilepsy.27,28,57 Additionally, postoperative memory function and quality of life appear to be positively related to seizure freedom after surgery.24
Memory assessment includes the use of standardized neuropsychological testing, intracarotid sodium amobarbital testing (Wada’s test), and more recently functional MRI.21–23 Additionally, detailed patient questioning regarding their own observations about memory and cognitive functioning are important because little correlation may exist between neuropsychological testing results and how the patient functions in day-to-day life. Although dominant temporal lobe surgery predisposes the patient to a decline in verbal memory and short-term memory functioning, the risks associated with nondominant temporal lobe surgery are less predictable. Visual spatial memory can be quantified during testing, and although removal of the nondominant hippocampus usually results in no apparent clinical deficits, impaired performance may be observed on postoperative retesting.
Considerable interest has focused on quality of life and psychiatric comorbidities associated with TLE. Depression and anxiety appear to be the most common psychiatric disturbances encountered before surgery, and depression is the most common encountered after surgery.58,59 Patients undergoing temporal lobectomy generally experience improved quality of life compared with medically treated patients.12,60–62 Measuring an individual’s improvement in day-to-day functions and well-being is important, and health-related quality-of-life (HRQOL) measurements are being used with increasing frequency in patients with medically intractable epilepsy. In a recent study by von Lehe and colleagues, HRQOL scores correlated positively with seizure control, and the authors suggested that to obtain better quality of life after epilepsy surgery, seizures must be controlled.63 In a randomized controlled trial for temporal lobectomy, the average quality of life measures at 6 months and 1 year were significantly higher in those treated with surgery.12 In this study, there were no differences in the rates of psychiatric comorbidities between the two groups.
Helmstaedter C. Neuropsychological aspects of epilepsy surgery. Epilepsy Behav. 2004;5:S45-S55.
Jeha L, Najm I, Bingaman W, et al. Predictors of outcome after temporal lobectomy for the treatment of intractable epilepsy. Neurology. 2006;66:1938-1940.
Kwan P, Brodie MJ. Early identification of refractory epilepsy. N Engl J Med. 2000;342:314-319.
Nogueira de Almeida A, Teixeira MJ, Feindel WH. From lateral to mesial: the quest for a surgical cure for temporal lobe epilepsy. Epilepsia. 2008;49:98-107.
Seidenberg M, Hermann B, Wyler A, et al. Neuropsychological outcome following anterior temporal lobectomy in patients with and without the syndrome of mesial temporal lobe epilepsy. Neuropsychology. 1998;12:303-316.
Spencer SS. The relative contributions of MRI, SPECT, and PET imaging in epilepsy. Epilepsia. 1994;35:S72-S89.
Tanriverdi T, Olivier A, Poulin N, et al. Long-term seizure outcome after mesial temporal lobe epilepsy surgery: corticalamygdalohippocampectomy versus selective amygdalohippocampectomy. J Neurosurg. 2008;108:517-524.
Wen HT, Rhoton AL, De Oliveira E, et al. Microsurgical anatomy of the temporal lobe. Part 1: mesial temporal lobe anatomy and its vascular relationships as applied to amygdalohippocampectomy. Neurosurgery. 1999;45:549-591.
Wiebe S, Blume WT, Girvin JP, et al. A randomized, controlled trial of surgery for temporal lobe epilepsy. N Engl J Med. 2001;345:311-318.
Wyler AR, Hermann BP, Somes G. Extent of medial temporal lobe resection on outcome from anterior temporal lobectomy: a randomized prospective study. Neurosurgery. 1995;37:982-991.
1 Nogueira de Almeida A, Teixeira MJ, Feindel WH. From lateral to mesial: the quest for a surgical cure for temporal lobe epilepsy. Epilepsia. 2008;49:98-107.
2 Jasper HH, Kershman J. Electroencephalographic classification of the epilepsies. Arch Neurol Psychiatry. 1941;45:903-943.
3 Penfield W, Flanigin H. Surgical therapy of temporal lobe seizures. Arch Neurol Psychiatry. 1950;64:491-500.
4 Bailey P, Gibbs F. The surgical treatment of psychomotor epilepsy. JAMA. 1951;145:365-370.
5 Kaada BR. Somato-motor, autonomic and electrocorticographic responses to electrical stimulation of “rhinencephalic” and other structures in primates, cat, and dog. Acta Physiol Scand. 1951;24:1-285.
6 Gastaut H, Vigouroux M, Naquet R. Lesions epileptogenes amygdalo-hippocampiques provoquees chez le chat par injection de crème d’alumine. Rev Neurol. 1952;87:607-609.
7 Feindel W, Gloor P. Comparison of electroencephalographic effects of stimulation of amygdala and brainstem reticular formation in cats. Electroencephalogr Clin Neurophysiol. 1954;6:389-402.
8 Feindel W, Penfield W, Jasper H. Localization of epileptic discharge in temporal lobe automatism. Trans Am Neurol Assoc. 1952;77:14-17.
9 Penfield W, Baldwin M. Temporal lobe seizures and the technique of subtotal temporal lobectomy. Ann Surg. 1952;136:625-634.
10 Falconer MA. Discussion on the surgery of temporal lobe epilepsy: surgical and pathological results. Proc R Soc Med. 1953;46:971-974.
11 Kwan P, Brodie MJ. Early identification of refractory epilepsy. N Engl J Med. 2000;342:314-319.
12 Wiebe S, Blume WT, Girvin JP, et al. A randomized, controlled trial of surgery for temporal lobe epilepsy. N Engl J Med. 2001;345:311-318.
13 Rosenow F, Luders H. Presurgical evaluation of epilepsy. Brain. 2001;124:1683-1700.
14 Ebner A, Hoppe M. Noninvasive electroencephalography and mesial temporal sclerosis. J Clin Neurophysiol. 1995;12:23-31.
15 Chee MW, Morris HH3rd, Antar MA, et al. Presurgical evaluation of temporal lobe epilepsy using interictal temporal spikes and positron emission tomography. Arch Neurol. 1993;50:45-48.
16 Hamer H, Najm I, Mohamed A, Wyllie E. Interictal epileptiform discharges in temporal lobe epilepsy due to hippocampal sclerosis versus mesial temporal tumors. Epilepsia. 1999;40:1261-1268.
17 Prayson RA, Reith JD, Najm IM. Mesial temporal sclerosis. A clinico-pathologic study of 27 patients, including 5 with coexistent cortical dysplasia. Arch Pathol Lab Med. 1996;120:532-536.
18 Diehl B, Najm I, La Presto E, et al. Temporal lobe volumes in patients with hippocampal sclerosis with or without cortical dysplasia. Neurology. 2004;62:1729-1735.
19 Kalnins RM, McIntosh A, Saling MM, et al. Subtle microscopic abnormalities in hippocampal sclerosis do not predict clinical features of temporal lobe epilepsy. Epilepsia. 2004;45:940-947.
20 Spencer SS. The relative contributions of MRI, SPECT, and PET imaging in epilepsy. Epilepsia. 1994;35:S72-S89.
21 Richardson MP, Strange BA, Thompson PJ, et al. Pre-operative verbal memory fMRI predicts post-operative memory decline after left temporal lobe resection. Brain. 2004;127:2419-2426.
22 Rabin ML, Narayan VM, Kimberg DY, et al. Functional MRI predicts post-surgical memory following temporal lobectomy. Brain. 2004;127:2286-2298.
23 Branco DM, Suarez RO, Whalen S, et al. Functional MRI of memory in the hippocampus: laterality indices may be more meaningful if calculated from whole voxel distributions. Neuroimage. 2006;32:592-602.
24 Helmstaedter C. Neuropsychological aspects of epilepsy surgery. Epilepsy Behav. 2004;5:S45-S55.
25 Seidenberg M, Hermann BP, Schoenfeld J, et al. Reorganization of verbal memory function in early onset left temporal lobe epilepsy. Brain Cogn. 1997;35:132-148.
26 Seidenberg M, Hermann B, Wyler A, et al. Neuropsychological outcome following anterior temporal lobectomy in patients with and without the syndrome of mesial temporal lobe epilepsy. Neuropsychology. 1998;12:303-316.
27 LoGalbo A, Sawrie S, Roth DL, et al. Verbal memory outcome in patients with normal preoperative verbal memory and left mesial temporal sclerosis. Epilepsy Behav. 2005;6:337-341.
28 Hamberger MJ, Drake EB. Cognitive functioning following epilepsy surgery. Curr Neurol Neurosci Rep. 2006;6:319-326.
29 Wen HT, Rhoton AL, De Oliveira E, et al. Microsurgical anatomy of the temporal lobe. Part 1: mesial temporal lobe anatomy and its vascular relationships as applied to amygdalohippocampectomy. Neurosurgery. 1999;45:549-591.
30 Haglund M, Berger M, Shamseldin M, et al. Cortical localization of temporal lobe language sites in patients with gliomas. Neurosurgery. 1994;34:567-576.
31 Ojemann GA. Brain organization for language from the perspective of electrical stimulation mapping. Behav Brain Res. 1983;6:189-230.
32 Schaffler L, Luders HO, Morris HH, et al. Anatomic distribution of cortical language sites in the basal temporal language area in patients with left temporal lobe epilepsy. Epilepsia. 1994;35:525-528.
33 Nilsson D, Malmgren K, Rydenhag B, et al. Visual field defects after temporal lobectomy—comparing methods and analyzing resection size. Acta Neurol Scand. 2004;110:301-307.
34 Wyler AR, Hermann BP, Somes G. Extent of medial temporal lobe resection on outcome from anterior temporal lobectomy: a randomized prospective study. Neurosurgery. 1995;37:982-991.
35 Pekar L, Blaha M, Schwab J, et al. Craniotomy and the temporal branch of the facial nerve. Rozhl Chir. 2004;83:205-208.
36 Jeha L, Najm I, Bingaman W, et al. Predictors of outcome after temporal lobectomy for the treatment of intractable epilepsy. Neurology. 2006;66:1938-1940.
37 Tanriverdi T, Olivier A, Poulin N, et al. Long-term seizure outcome after mesial temporal lobe epilepsy surgery: corticalamygdalohippocampectomy versus selective amygdalohippocampectomy. J Neurosurg. 2008;108:517-524.
38 Janszky J, Pannek HW, Janszky I, et al. Failed surgery for temporal lobe epilepsy: predictors of long-term seizure-free course. Epilepsy Res. 2005;64:35-44.
39 Dupont S, Tanguy ML, Clemenceau S, et al. Long-term prognosis and psychosocial outcomes after surgery for MTLE. Epilepsia. 2006;47:2115-2124.
40 McIntosh AM, Kalnins RM, Mitchell LA, et al. Temporal lobectomy: long-term seizure outcome, late recurrence and risks for seizure recurrence. Brain. 2004;127:2018-2030.
41 Hennessy MJ, Elwes RD, Rabe-Hesketh S, et al. Prognostic factors in the surgical treatment of medically intractable epilepsy associated with mesial temporal sclerosis. Acta Neurol Scand. 2001;103:344-350.
42 Kuzniecky R, Ho SS, Martin R, et al. Temporal lobe developmental malformations and hippocampal sclerosis: epilepsy surgical outcome. Neurology. 1999;52:479-484.
43 Janszky J, Janszky I, Schulz R, et al. Temporal lobe epilepsy with hippocampal sclerosis: predictors of long-term surgical outcome. Brain. 2005;128:395-404.
44 Berkovic SF, McIntosh AM, Kalnins RM. Pre-operative MRI predicts outcome of temporal lobectomy. Neurology. 1995;45:1358-1363.
45 Rasmussen T. The neurosurgical treatment of focal epilepsy. In: Niedermeyer E, editor. Modern Problems of Pharmacopsychiatry: Epilepsy, Vol. 4. New York: Krager; 1970:306-325.
46 Ficker DM, So EL, Mosewich RK, et al. Improvement and deterioration of seizure control during the postsurgical course of epilepsy surgery patients. Epilepsia. 1999;40:62-67.
47 Weiser HG, Ortega M, Friedman A, et al. Long-term seizure outcomes following amygdalohippocampectomy. J Neurosurg. 2003;98:751-763.
48 Wiebe S. Effectiveness and safety of epilepsy surgery: what is the evidence? CNS Spectr. 2004;9:120-122. 126-132
49 Salinsky MC. The vagus nerve stimulation study group. A randomized controlled trial of chronic vagus nerve stimulation for the treatment of medically intractable seizures. Neurology. 1995;45:224-230.
50 Handforth A, DeGiorgio CM, Schachter SC, et al. Vagus nerve stimulation therapy for partial-onset seizures: a randomized active-control trial. Neurology. 1998;51:48-55.
51 Amar AP, Heck CN, Levy ML, et al. An institutional experience with cervical vagus nerve trunk stimulation for medically refractory epilepsy: rationale, technique, and outcome. Neurosurgery. 1998;43:1265-1276.
52 Scherrmann J, Hoppe C, Kral T, et al. Vagus nerve stimulation: clinical experience in a large patient series. J Clin Neurophysiol. 2001;18:408-414.
53 Engel J, Wiebe S, French J, et al. Practice parameter: temporal lobe and localized neocortical resections for epilepsy: report of the Quality Standards subcommittee of the American Academy of Neurology in association with the American Epilepsy Society and the American Association of Neurological Surgeons. Neurology. 2003;60:538-547.
54 Sindou M, Guenot M, Isnard J, et al. Temporo-mesial epilepsy surgery: outcome and complications in 100 consecutive adult patients. Acta Neurochir. 2006;148:39-45.
55 Tecoma ES, Laxer KD, Barbaro NM, et al. Frequency and characteristics of visual field deficits after surgery for mesial temporal sclerosis. Neurology. 1993;43:1235-1238.
56 Marino R, Rasmussen T. Visual field changes after temporal lobectomy in man. Neurology. 1968;18:825-835.
57 Davies KG, Risse GL, Gates JR. Naming ability after tailored left temporal resection with extraoperative language mapping: increased risk of decline with later epilepsy onset age. Epilepsy Behav. 2005;7:273-278.
58 Cankurtaran ES, Ulug B, Saygi S, et al. Psychiatric morbidity, quality of life, and disability in mesial temporal lobe epilepsy patients before and after anterior temporal lobectomy. Epilepsy Behav. 2005;7:116-122.
59 Blumer D, Wakhlu S, Davies K, et al. Psychiatric outcome of temporal lobectomy for epilepsy: incidence and treatment of psychiatric complications. Epilepsia. 1998;39:478-486.
60 Derry PA, Wiebe S. Psychological adjustment to success and failure following epilepsy surgery. Can J Neurol Sci. 2000;27:116-120.
61 Selai CE, Elstner K, Trimble MR. Quality of life pre and post epilepsy surgery. Epilepsia Res. 2000;38:67-74.
62 Gilliam F, Kuzniecky R, Meador K, et al. Patient-oriented outcome assessment after temporal lobectomy for refractory epilepsy. Neurology. 1999;53:687-694.
63 Von Lehe M, Lutz M, Kral T, et al. Correlation of health-related quality of life after surgery for mesial temporal lobe epilepsy with two seizure outcome scales. Epilepsy Behav. 2006;9:73-82.