CHAPTER 25 Stability of the Distal Radioulnar Joint
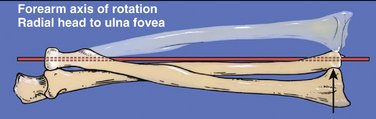
The longitudinal axis of forearm pronation/supination passes through the center of the radial head proximally and through the foveal sulcus at the lateral base of the ulnar styloid distally. Af Ekenstam and Hagert1 defined the pole of the distal ulna as that portion adjacent to the triangular fibrocartilage (TFC) that is covered by hyaline cartilage and responsible for absorption of load transferred to the forearm from the medial carpus, through the articular disc of the TFC onto the ulna. The fovea is the recess lying between hyaline cartilage of the ulnar pole and the ulnar styloid. This fossa is richly vascularized; it serves as a point of insertion of the major distal radioulnar joint (DRUJ), stabilizing the ligamentous components of the TFC.
Advances in Understanding of Anatomy and Biomechanics of the Distal Radioulnar Joint
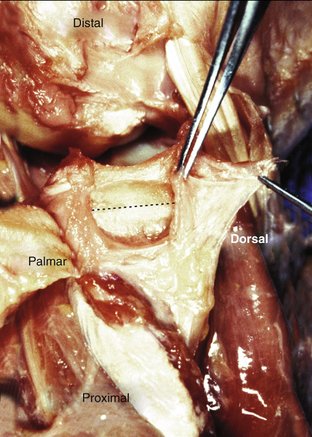
Research published particularly over the past 30 years now gives us a clear understanding of how the anatomical position of the fovea and the deep components of the TFC are critical to the rotational and translational stability of the DRUJ. Anatomical works by Bednar and associates, in 1991,2 and Thiru-Pathi and colleagues, in 1986,3 independently demonstrate the rich vascularity within the ulnar fovea. These authors also described the source of vascular nutrition of all peripheral tissues of the TFC, both dorsal and palmar. Their two landmark papers also describe the avascular, central articular disc of the TFC, nourished by synovial fluid from both the DRUJ and the ulnocarpal joint.
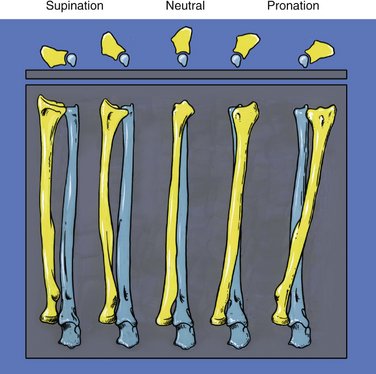
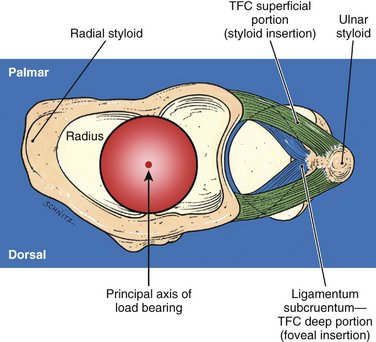
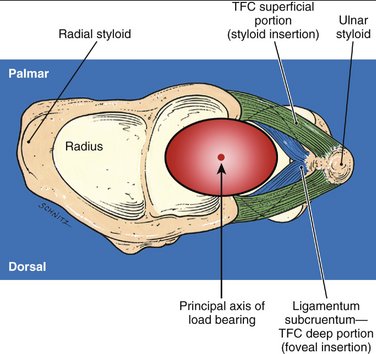
At the ginglymus ulnotrochlear joint of the elbow, the ulna participates only in forearm flexion and extension; it does not rotate. Forearm pronation/supination involves rotation of the radiocarpal unit (with the attached hand) around a rotationally fixed and stable ulna. The complex architecture of the ulnotrochlear articular surfaces and the collateral ligament stabilizers of the elbow allow the ulna to move as a hinge only, without a rotational component. The longitudinal axis around which rotation takes place can be visualized in Figure 25-1. The anatomy of the sigmoid notch of the radius, the seat of the ulna (which articulates with the notch), and the guiding, checkrein potential of the components of the TFC allow 90 degrees of forearm supination (at which point the two forearm bones are essentially parallel, and the interosseous space the widest) to 90 degrees of pronation, at which point the radius has rotated across the anterior surface of the fixed ulna (Fig. 25-2). The principal axis* of load bearing at the DRUJ tracks obliquely across the sigmoid notch as the radiocarpal unit pronates/supinates around the fixed ulna (Fig. 25-3). The tracking line is from distal/dorsal in pronation to proximal/palmar in supination.
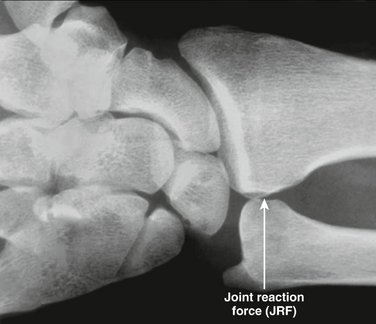
In the human bipedal condition, with flexed elbows at the side (prepared for work), the radiocarpal unit rests “on top” of the ulnar seat, with gravity pulling the hand and its load toward the ground (Fig. 25-4). This so-called zero-rotation position of the forearm has been nicely described by Palmer.4 In this position—the most common for human forearm function—a significant joint reaction force (JRF) can develop between the sigmoid notch of the radius and the rotationally fixed ulnar seat (see Fig. 25-4). Usually, radiographs of the carpus are viewed with the fingers toward the ceiling. Students of hand surgery learn that it is easier to develop three-dimensional thinking about the anatomy of the wrist and the distal end of the ulna if (1) their patients are clinically examined with their elbows on the examining table and their fingers toward the ceiling; (2) if radiographs are viewed with the fingers toward the ceiling; and (3) if arthroscopy of the wrist is performed with the fingers toward the ceiling.
I have reoriented Figure 25-4, however, to allow the reader an appreciation of the “zero-rotation” position of the working forearm, with the radial and ulnar styloids at their widest anatomical separation and the forearm in neutral rotation (0 degrees of pronation/supination). In this position, the principal axis of load bearing at the DRUJ passes through the center of the sigmoid notch and the center of the seat of the ulna. In zero rotation, the various radioulnar ligament components of the TFC are under the least amount of tension.1,5
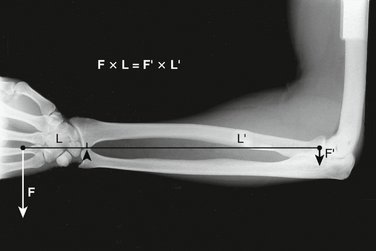
The structural presence and health of articular surface cartilage on the ulnar seat (as well as the sigmoid notch) are critical in providing a painless mechanical fulcrum for all radioulnar load-bearing activity. In a state of equilibrium (no forearm motion), all moments around a fixed fulcrum (i.e., the seat of the ulna) must be equal (Fig. 25-5). The loaded hand (F) times the length of the loaded hand from the fulcrum provided by the seat of the ulna (L) must be equal to the moment (F′ × L′) on the proximal side of the fulcrum:
where F′ is the stability provided at the radiocapitellar joint by the annular ligament encircling the radial head and L′ is the entire length of the forearm. Because F × L = F′ × L′, the relatively long forearm makes the requirement for proximal radius stability by the annular ligament (F′) relatively small, regardless of the load in the hand.
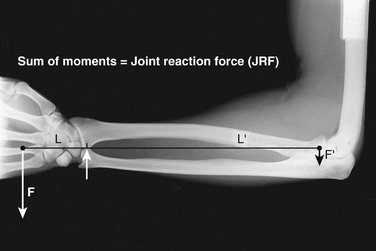
The sum of all moments distal and proximal to this fulcrum equals the total load on the fulcrum (the ulnar seat) itself, defined as the joint reaction force (JRF) at the DRUJ (Fig. 25-6). Based on how much load is in the hand (F), and the size of the moment distal to the DRUJ, the reader begins to appreciate the potential magnitude of the JRF at the DRUJ and the importance of surface hyaline cartilage health at both the sigmoid notch and the ulnar seat for painless DRUJ function.
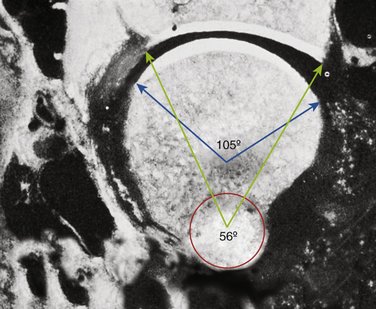
Using elegant cadaver dissections, in 1985 af Ekenstam and Hagert1,6 demonstrated that the concave radius of curvature of the sigmoid notch is greater than that of the ulnar seat (Fig. 25-7). This incongruity of articular surfaces creates a geometrically nonconstrained articulation at the DRUJ, subject to translational dorsal and palmar instability of the sigmoid notch on the ulnar seat. Not only does the radiocarpal unit rotate around the fixed ulnar seat in pronation/supination, but the flatter surface of the sigmoid notch also has enough inherent instability through incongruous cartilage surfaces to allow translation of the notch palmarly or dorsally on the fixed ulna as the forearm rotates into pronation or supination, respectively. The DRUJ is not a ball-and-socket joint. Figure 25-3 reveals the exposed cadaver sigmoid notch (the ulna has been dissected free and hinged palmarly out of the notch to the reader’s left), showing the oblique tracking line of the principal axis of forearm load bearing through a full pronation/supination arc at the DRUJ (see earlier). Because rotation of the radius across the ulna from supination to pronation results in relative ulnar-positive variance4 at the end arc of forearm pronation, the tracking line of the principal axis of load bearing across the sigmoid notch must—by definition—be oblique. It tracks from slightly more proximal at the palmar edge of the notch in full supination to slightly more distal at the dorsal edge of the notch in full pronation.
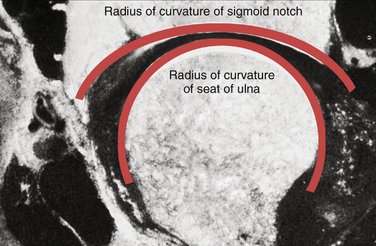
FIGURE 25-7 Transverse section through the DRUJ. The radius of curvature of the sigmoid notch is greater than the radius of curvature of the seat of the ulna, leading to an inherent instability of the DRUJ through an arc of pronation/supination. Rotation of the forearm around a longitudinal axis of rotation (see Fig. 25-1) is manifest at the DRUJ by rotation and translation of the sigmoid notch against the ulnar seat.
(From Af Ekenstam F, Hagert CG: Anatomical studies on the geometry and stability of the distal radioulnar joint. Scand J Plast Reconstr Surg. 1985; 19:17-25.)
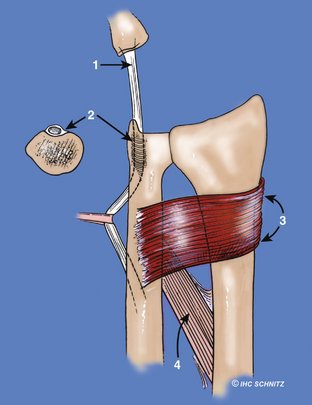
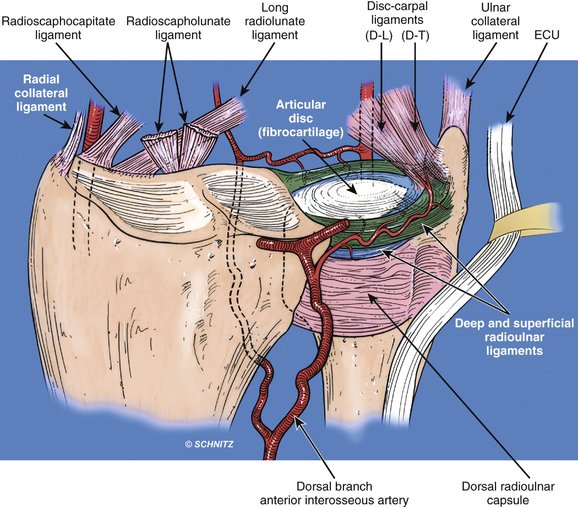
Stability of the DRUJ
With inherently unstable, nonconstrained articular surfaces, anatomical stability of the DRUJ is achieved through extrinsic extracapsular as well as intrinsic intracapsular structures. Extrinsic stability is provided principally by (1) dynamic tensioning of the extensor carpi ulnaris (ECU) as its tendon crosses the distal head of the ulna7,8; (2) the semi-rigid sixth dorsal compartment itself, constraining the ECU tendon7,8; (3) dynamic support provided by the superficial and deep heads of the pronator quadratus9; and (4) the interosseous ligament of the mid forearm10 (Fig. 25-8). The extrinsic DRUJ stabilizers are of secondary importance compared with the more biomechanically effective intrinsic radioulnar components of the TFC.1,2,6 Dorsal and palmar radioulnar TFC fibers arise from the medial border of the distal radius and insert on the ulna at two separate and distinct sites: (1) the fovea at the base of the ulnar styloid and (2) the ulnar styloid itself. Figure 25-9 emphasizes the well-vascularized nature of the dorsal and palmar radioulnar ligaments. Figure 25-10 illustrates the critical and clinically significant difference between the angle of attack of the dorsal and palmar superficial radioulnar fibers inserting on the ulnar styloid and the deep fibers inserting onto the fovea. Well-vascularized, longitudinally oriented connective tissue fibers of the TFC anchor the radius to the ulna along both its dorsal and palmar margins. The blood supply to both these areas of the periphery of the TFC is through branches of the posterior interosseous artery (see Fig. 25-9).2,3 These vessels course along the dorsal and palmar radioulnar ligaments penetrating and nourishing the dorsal 20% and palmar 20% of the TFC.2,3 Between these two sets of DRUJ checkreins, the articular disc is nourished by synovial fluid washing from the ulnocarpal joint distally and the DRUJ proximally. The articular disc is primarily responsible for load transmission from the medial carpus to the forearm, particularly with the hand-forearm unit in ulnar deviation. In neutral deviation of the hand-forearm unit, the principal axis of load transmission passes from the hand, through the head of the capitate, then the scapholunate ligament, and finally onto the articular surface of the distal radius at the interfossal ridge, which separates the elliptical (scaphoid-bearing) and spherical (lunate-bearing) fossae of the distal radius (see Figs. 25-10 and 25-11). Af Ekenstam and colleagues6 have demonstrated in the laboratory that, in neutral position of the wrist, 84% of hand load is transferred to the radius and only 16% is transferred through the central articular disc of the TFC. With ulnar deviation of the hand-forearm unit (Figs. 25-12 and 25-13), the principal axis of load bearing shifts medially, placing more load on the articular disc and the pole of the distal ulna, rather than on the interfossal ridge of the distal radius when the hand-forearm unit is in neutral deviation.
How the TFC Components Guide the Radiocarpal Unit around a Fixed Ulna: The Significance of Rotation and Translation
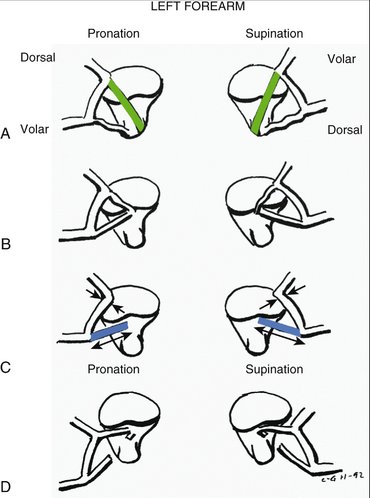
The dorsal and palmar radioulnar ligaments consist of superficial components inserting directly onto the ulnar styloid and deep components inserting significantly more laterally, into the fovea adjacent to the articular surface of the pole of the distal ulna (Fig. 25-14). These two components of the TFC are distinct in both their anatomy and function. Scrutiny of Figure 25-14 reveals that fibers of the superficial component form an acute angle as they converge on the ulnar styloid from the medial radius. This narrow angle of attack gives the superficial TFC a poor mechanical advantage for guiding the radiocarpal unit through an arc of pronation/supination. The deep components of the TFC (arising along the medial border of the distal radius, but inserting into the fovea), however, form an obtuse angle of attack, which is much more mechanically advantageous in stabilizing rotation of the radius around the fixed ulna (see Fig. 25-14). The deep components of the TFC have been referred to by wrist investigators as the ligamentum subcruentum. In his landmark 1975 article on the “Articular Disc of the Hand,” Kauer11 gives credit to Henle12 and Fick13 for describing a vascularized fissure between the superficial and deep components of the TFC, which they called the “ligamentum subcruentum” but technically was not a ligament at all. More recently, however, the term “ligamentum subcruentum” has come to represent the deep fibers of the TFC (inserting into the fovea) and is now used commonly by many wrist investigators as interchangeable with the term “deep TFC radioulnar ligaments.”
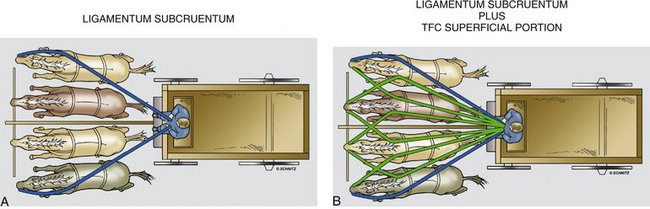
Figures 25-11 and 25-13 schematically represent the superficial radioulnar ligaments (green) and the deep ligamentum subcruentum (blue) in transverse section through the ulnocarpal joint. The distinct differences in fiber orientation and mechanical advantage of the deep radioulnar ligaments in controlling forearm rotation are apparent. It might be easier, however, to understand the relative difference in the effectiveness of the superficial and deep radioulnar ligaments of the TFC in controlling physiological forearm rotation and translation using an analogy of a team of horses, a buckboard, and a driver (Fig. 25-15). The team of horses represents the radius; the seat of the buckboard is the fovea of the ulna. The buckboard driver holds the reins securely at the buckboard seat (the ulnar fovea). The angle of attack of the blue reins to the two outside horses of the team represents the angle of attack of the deep dorsal and palmar fibers of the ligamentum subcruentum from the radius (the team of horses) to the foveal sulcus of the ulna (the seated buckboard driver). Their orientation makes the angle of attack on the outside horses of the team much more effective in turning the team of horses (the radius) around the buckboard (the ulna). The narrower, acute angle of attack of the superficial TFC fibers is represented as green reins connecting the driver to the central horses of the team. This angle of attack is much less effective in controlling rotation of the team relative to the driver (see Fig. 25-15B). Like the diagrammatic obtuse blue fibers of the ligamentum subcruentum in Figures 25-11 and 25-13, the blue reins are much more effective in controlling the team of horses by virtue of their obtuse angle of attack on the two outside horses.
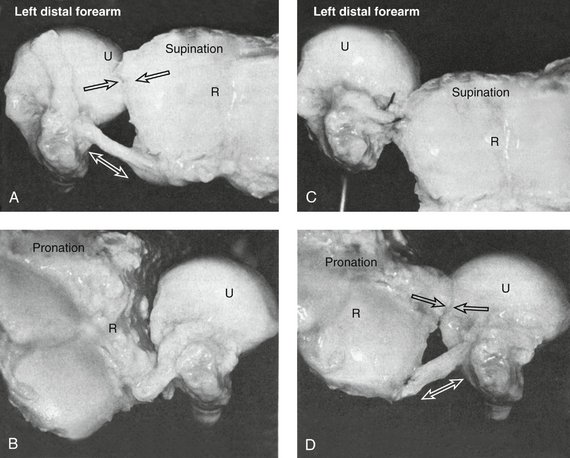
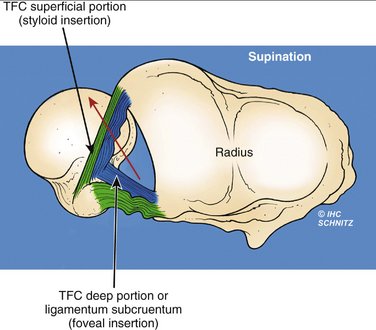
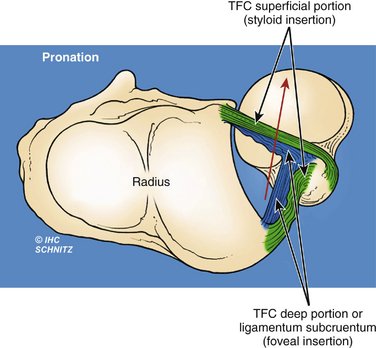
Af Ekenstam and Hagert first suggested in 19851 that the deep fibers of the TFC were the principal intrinsic stabilizers of the DRUJ. Although these investigators used cadaver dissections and experimental techniques that might be considered somewhat basic by today’s standards, their conclusions were sound: in forearm supination the dorsal, deep fibers of the ligamentum subcruentum tighten significantly while the deep palmar fibers remain lax. This suggests a pulling, tethering mechanism for controlling stability during DRUJ rotation (Fig. 25-16). Conversely, these authors found that the palmar, deep fibers of the ligamentum subcruentum were the principal restraints against superphysiological palmar migration of the radiocarpal unit at the sigmoid notch in pronation (see Fig. 25-16).
In 1991, Schuind and associates,5 from the Mayo Clinic Biomechanics Laboratory, refuting af Ekenstam and Hagert’s 1985 work, suggested a totally different TFC function for controlling forearm stability. Using a sophisticated stereophotogrammatic technique with phosphorescent markers and computer analysis, the authors concluded that the dorsal fibers of the TFC tighten in pronation and the palmar fibers tighten in supination, conclusions opposite those published by af Ekenstam and Hagert 6 years earlier.
Controversy raged in the academic hand surgical world until 1994, when Hagert—carefully studying the conflicting conclusions from 1985 and 1991—recognized that both research groups were correct but that each was examining a different piece of the puzzle. In a small, but brilliant work published in 1994,14 Hagert clarified the biomechanical effect of each component of the TFC for the first time. In this article he reasoned that his earlier 1985 publication studied only the deep components of the TFC—those inserting into the fovea of the ulna. This was a consequence of aggressive excision of the central articular disc for the 1985 study, which affected the integrity of the dorsal and palmar superficial TFC radioulnar ligaments. He also implied that the phosphorescent markers applied to the surface of the TFC by Schuind and associates5 measured developing tension or tightening of the superficial radioulnar ligaments only, as these fibers enveloped the articular disc. The surface phosphorescent markers, however, did not consider the biomechanics of the radiofoveal deep fibers, with their much more mechanically effective angle of attack. Hagert clearly stated that in forearm pronation, the dorsal superficial fibers of the TFC must tighten for stability as do the deep palmar fibers of the ligamentum subcruentum. Conversely, in supination, the palmar superficial TFC radioulnar fibers (to the ulnar styloid) tighten as do the deep dorsal fibers of the ligamentum subcruentum, making both theories correct (Fig. 25-17).
Two critical anatomical factors are responsible for a more significant stabilizing effect of the ligamentum subcruentum on forearm rotation than the superficial radioulnar ligaments of the TFC: first, full forearm pronation allows the principal axis of load bearing at the DRUJ to track distally and dorsally along the sigmoid notch to a point where less than 10% of the dorsal notch is still in contact with the articular seat of the ulna.1 In this position, most of the hyaline cartilage–covered distal end of the ulna has herniated against the dorsal DRUJ capsule,15 out from under the confining cover of the dorsal superficial radioulnar fibers of the TFC that attach to the bony ulnar styloid. In maximum pronation, DRUJ stability is based almost entirely on the restraining, pulling action of the palmar, deep fibers of the ligamentum subcruentum, preventing superphysiological translation from occurring. Second, the obtuse angle of attack of these deep fibers (recall the analogy of the team of horses and the buckboard) is perfectly oriented to prevent DRUJ subluxation. More than any other intrinsic or extrinsic DRUJ-stabilizing components discussed earlier, these two anatomical considerations are responsible for DRUJ stability.
Conversely, in full supination (as the sigmoid notch migrates dorsally on the ulnar seat to less than 10% articular surface contact1) the superficial palmar TFC fibers become ineffective as the ulnar head rolls out beyond their effective confines, stretching the palmar DRUJ capsule.15 At the same time, the dorsal ligamentum subcruentum tightens and its obtuse orientation becomes mechanically advantageous in restraining the radiocarpal unit from superphysiological dorsal migration on the seat of the ulna. The profound stabilizing importance of the ligamentum subcruentum relative to the superficial fibers of the TFC becomes quite clear.
Provocative Maneuvers for Determining the Health and Integrity of the Ligamentum Subcruentum: The Perpetual Role of Physical Diagnosis in Hand Surgery
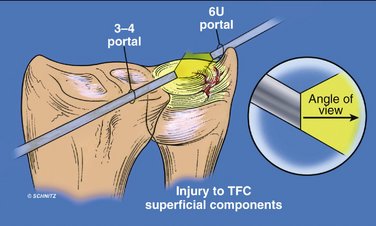
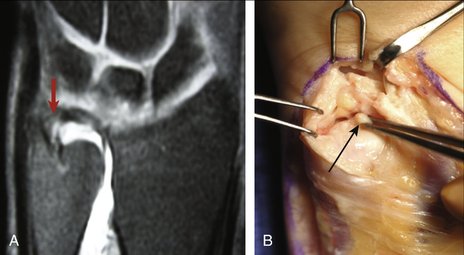
Direct arthroscopy of the TFC through the ulnocarpal joint can, unfortunately, only provide information about the integrity and health of the superficial dorsal and palmar fibers of the TFC and the articular disc (Fig. 25-18). Ulnocarpal arthroscopy will not allow the surgeon visualization of the deeper ligamentum subcruentum unless the superficial TFC has been completely ruptured and retracted from its moorings on the bony ulnar styloid, or if a large, central degenerative hole has been worn through the articular disc.16 The clinician can, however, examine the distal forearm for health and integrity of the dorsal and palmar components of the ligamentum subcruentum using precise provocative maneuvers and physical diagnostic techniques.
Physical findings of pain and/or instability with these two provocative maneuvers must always be compared with findings of the opposite, uninjured extremity.
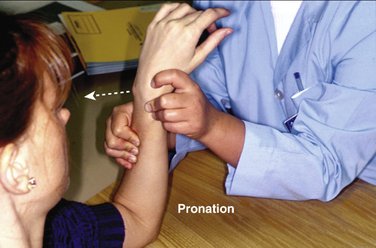
These physical diagnostic techniques are highly reliable. They are precise in detecting painful instability of the DRUJ, whether secondary to inflammatory arthropathy or trauma. The importance of provocative maneuvers that can isolate the deep TFC ligamentum subcruentum from the superficial radioulnar ligaments cannot be overstated, especially because no information about the condition of the ligamentum subcruentum can be gleaned from ulnocarpal arthroscopy (see Fig. 25-18). In full supination, essentially all load introduced by the examiner’s hand stresses the dorsal ligamentum subcruentum (Fig. 25-21), as the seat of the ulna is translated along the sigmoid notch beyond the confines of the superficial palmar TFC fibers. In full pronation, introduction of a superphysiological load by the examiner’s thumb against the distal ulna stress-tests the palmar ligamentum subcruentum, eliciting pain and/or instability in its pathological state (Fig. 25-22). Physical diagnosis of injury to the deep fibers of the TFC should be considered the “gold standard” in clinical evaluation of the TFC. Once the clinician understands the significance of TFC fiber orientation and can appreciate the importance of the critical angle of attack of the deep TFC fibers from the medial radius to the ulnar fovea, injuries to the TFC leading to either subtle or gross instability can be readily identified by careful physical examination.
A new generation of wrist coils has improved the diagnostic potential of magnetic resonance imaging (MRI) over the past 15 years. There are many published studies corroborating MRI findings at the distal end of the ulna by open surgical exploration; diagnostic accuracy has become much more reasonable in recent years. But MRI with or without gadolinium contrast should not be regarded as a substitute for a thorough physical examination of the DRUJ and the TFC, particularly through use of direct palpation of the periphery of the TFC and stress-testing techniques. The MR image in Figure 25-23A clearly shows integrity of the superficial radioulnar ligaments arising from the medial radius and inserting into the ulnar styloid; contrast agent is observed streaming around the pole of the distal ulna, across the fovea to the base of the styloid, suggesting complete avulsion of the ligamentum subcruentum (deep TFC fibers) from the foveal sulcus. This massive injury to the deep components of the TFC resulted in painful dorsal and palmar translational instability at the DRUJ in this patient. Provocative stress-testing (described earlier) was clinically positive in both pronation and supination. Figure 25-23B demonstrates intraoperative findings of complete avulsion of the ligamentum subcruentum from the ulnar fovea. While possibly corroborating the clinician’s physical findings, MRI should be considered only helpful in assessing the condition of a patient’s TFC but not definitively diagnostic. The incidence of false-positive and false-negative MRI findings still remains very high today. MRI findings should always require clinical correlation by the examining physician.
Displaced Basilar Ulnar Styloid Fractures
With newfound understanding of the integral role played by the ligamentum subcruentum in DRUJ mechanics, more critical attention should be given to displaced basilar ulnar styloid fractures, so often occurring in association with fractures of the distal radius. Laboratory cadaver studies by Viegas and colleagues, in 1990,17 demonstrate certain conditions necessary for traumatic ulnar styloid failure and displacement. Their results suggest that with certain losses of radius length, palmar tilt, and/or angle of inclination associated with distal radius fractures, enough tension could be placed on the ulnar styloid through the intact superficial radioulnar ligaments of the TFC that the bony styloid could be avulsed from its base as the fractured distal radius fragments displace. With the ulnar styloid (and TFC) intact, the authors could osteotomize the radius but achieve only the following in their laboratory: (1) radius shortening of 2 and 4 mm; (2) an angle of radius inclination of 10 degrees; and (3) a radius tilt of 0 degrees. However, if they first osteotomized the ulnar styloid through its base, the radius could be then shortened beyond 4 mm, the inclination could be reduced to at least 0 degrees, and a dorsal tilt of 15 degrees or 30 degrees could be achieved. The clinical implication of their work is clear: a distal radius fracture with metaphyseal collapse and shortening and/or dorsal tilt beyond the authors’ experimental methods can result in either a concomitant displaced fracture of the ulnar styloid (an avulsion fracture via intact superficial TFC components inserting onto the bony ulnar styloid) or an avulsion or tear of the TFC superficial ligaments from the styloid itself, with the bone remaining intact.18 In the clinical setting, one can readily appreciate that with displaced distal radius fractures, if the ulnar styloid has been avulsed at its base by the superficial TFC fibers that insert directly into the bony ulnar styloid, then—by definition—the deep fibers of the ligamentum subcruentum must also be avulsed and displaced from the fovea of the ulna, precisely the same distance as the ulnar styloid displacement from its bony base (Fig. 25-24). The potential effect of a ligamentum subcruentum injury of this nature on DRUJ stability, with or without concomitant avulsion of the ulnar styloid through its base, should be obvious. The hand surgeon must exercise judgment in determining whether the degree of ulnar styloid displacement is sufficient to justify surgical open reduction and stabilization. By surgically anchoring the displaced basilar ulnar styloid fracture back to its bony base by open reduction and internal fixation (at the same time as any required anatomical open reduction and internal fixation of the displaced distal radius fracture), the surgeon essentially ensures that the concomitantly avulsed ligamentum subcruentum is most closely approximated to the fovea. Once healed, the DRUJ-stabilizing function of the deep radioulnar component of the TFC has been restored. After anatomical alignment of the bony ulnar styloid, the deep TFC fibers can be maintained in this position by immobilization with a long arm cast for 6 weeks (preventing forearm rotation), with or without adjunctive percutaneous 0.062-inch Kirschner wires (K-wires) through the ulna into the radius in “zero rotation.” A more secure and predictable reattachment of the ligamentum subcruentum can be performed using bone-anchoring techniques directly to the foveal sulcus of the ulna (see later).
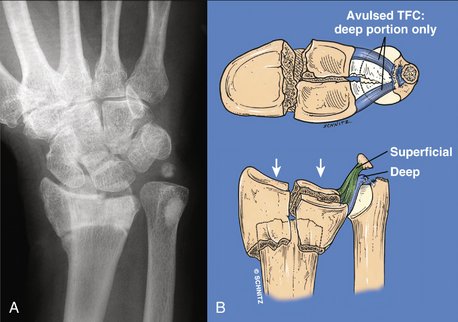
FIGURE 25-24 A and B, Basilar ulnar styloid fractures can be displaced in association with displaced distal radius fractures through tension on the intact superficial dorsal and palmar radioulnar ligaments (green). As the radius fracture fragments displace, the intact superficial radioulnar ligaments (green) can either rupture (see Palmer’s19 classification of traumatic TFC lesions) or remain intact, avulsing the entire styloid from its base (as in this example). If the superficial radioulnar ligaments (green) remain intact, as the styloid displaces from its base the deep fibers of the ligamentum subcruentum (blue) will be avulsed from their insertion at the ulnar fovea and displace the same distance as the initial displacement of the ulnar styloid. Figure A, Radiograph of the displaced radius and ulnar styloid fractures. B, Schematic representation of the tearing and separation of the critical ligamentum subcruentum (blue) as its foveal insertion fails.
Consequences of Failing to Appreciate TFC Anatomy When Treating Displaced Distal Radius Fractures
An example of the consequences of failing to respect this type of disruption of anatomy—and potential disturbance of normal DRUJ biomechanics—is seen in Figure 25-25A-C. A 19-year-old female college student fell off her bicycle onto the outstretched dominant hand, incurring this grossly displaced, extra-articular distal radius fracture. The extent of shortening and dorsal angulation is clear (see Fig. 25-25A, B). Also readily seen is the significant displacement of the ulnar styloid, avulsed through its base by the intact superficial radioulnar components of the TFC. The patient was treated elsewhere by closed reduction of her distal radius fracture and cast immobilization until radius bony union (see Fig. 25-25C). She presented for a second opinion in my office 9 months after her initial treatment (see Fig. 25-25D), complaining of disabling pain at the distal end of the ulna, particularly with loaded pronation and supination. Physical examination revealed (1) subtle hypermobility at the sigmoid notch on stress-testing the ligamentum subcruentum using the provocative maneuvers described earlier (relative to the opposite side); (2) full pronation and supination; and (3) 65 degrees of wrist extension and 75 degrees of wrist flexion. There was no tenderness on direct palpation of the ulnar styloid fracture nonunion. The “piano key” sign was negative. This traditional sign of micro-instability of the DRUJ is elicited by placing the seated patient with his or her palm flap on the examining table. The hypothenar eminence is forced firmly against the table by the patient, which causes a prominent and unstable distal ulna to relocate at the DRUJ. The action of the unstable ulna being forced up and down mimicks the action of a piano key.
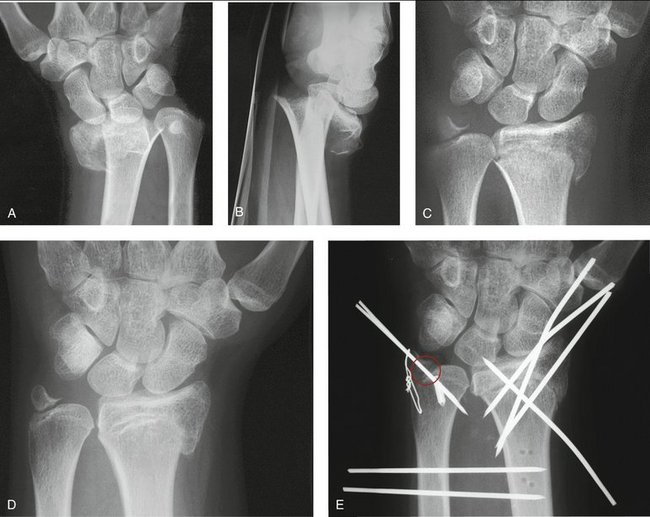
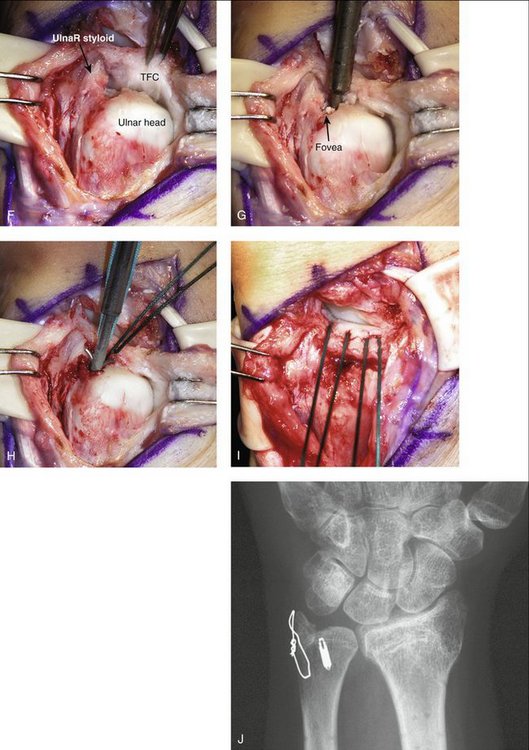
FIGURE 25-25 Anteroposterior (A) and lateral (B) radiographs of a 19-year-old woman who fell off a bicycle onto her outstretched dominant hand. The magnitude of radius shortening, dorsal angulation, and complete loss of inclination is readily seen. C, The patient was treated elsewhere by closed reduction and cast immobilization for 6 weeks. Anteroposterior radiograph out of plaster reveals lateral displacement of the distal radius fragment, with similar lateral displacement of the ulnar styloid through its base, avulsed by the intact superficial radioulnar ligaments of the TFC. D, Nine months after the initial injury, the radius is healed, the displaced ulnar styloid fracture nonunion is ankylosed and nontender, but the DRUJ is painful and unstable through a full arc of pronation/supination. Provocative maneuvers that stress the deep dorsal and deep palmar fibers of the ligamentum subcruentum were positive for pain and instability. E, Dome osteotomy of the radius malunion allowed a 6-mm medial shift of the distal radius fragment in this patient. The ulnar styloid could then be anatomically reduced at its base and held with tension-band wires. With the bony anatomy restored, the critical, deep radioulnar ligaments of the ligamentum subcruentum were now juxtaposed to the fovea (red circle) and could be securely reattached with a bone anchor. To eliminate any forearm rotation for 6 weeks, two 0.062-inch K-wires were introduced percutaneously through the distal shaft of the ulna into the radius. F to I, A sequence of intraoperative steps used to prepare the ulnar fovea for a bone anchor. Once placed deeply into the fovea, the standard 2-0 suture material manufactured with the anchor can be reinforced by the surgeon by adding additional suture material to the anchor, giving a potential four-strand attachment of the avulsed, deep radioulnar fibers of the ligamentum subcruentum to bone. J, Long-term follow-up anteroposterior radiograph. The patient recovered full, painless pronation/supination under load.
Radiographs of this young woman show a 6-mm, radially displaced malunion of the distal radius, with a 6-mm displacement of her ulnar styloid, avulsed through its bony base by the superficial dorsal and palmar radioulnar components of the TFC (see Fig. 25-25). The styloid is displaced from its base exactly the same distance as the lateral displacement of the distal radius fragment at the malunion site. The original displacement of the metaphyseal radius fracture at the time of injury impact pulled the ulnar styloid from its base by force-transmission through the intact superficial dorsal and palmar components of the TFC. As the bony styloid was avulsed from its base, the deep foveal attachments of the ligamentum subcruentum failed as well, destabilizing the DRUJ by loss of this critical anchor point. Failure by the first treating surgeon to anatomically reduce the distal radius not only resulted in a radius malunion and ulnar styloid nonunion (see Fig. 25-25) but also left the avulsed fibers of the deep ligamentum subcruentum adjacent to hyaline cartilage covering the distal ulnar pole. There was no potential whatsoever for the ligamentum subcruentum to heal to the fovea because of the magnitude of the initial fracture displacement.
The patient’s 6-mm radius malunion not only shifted the ulnar styloid from its anatomical base but also left the ligamentum subcruentum displaced to a position from which it could not be reanchored to the fovea without corrective osteotomy of the radius. A dome osteotomy of the radius was performed (see Fig. 25-25E), allowing a 6-mm medial shift of the distal radius, along with the superficial radioulnar ligaments and articular disc, all still attached to the ulnar styloid. The restored anatomy of the radius allowed the ulnar styloid fibrous union to be taken down, reduced, and anchored anatomically to its base using a tension-band wiring technique. With the ulnar styloid anatomically reduced, the deep fibers of the TFC could be restored to their anatomical insertion into the fovea. A bone anchor placed directly into the fovea (with an additional 2-0 Fiberwire added to the 2-0 Ethibond suture already attached) ensured an anatomical insertion of the deep fibers of the TFC. Fixation techniques for the radius dome osteotomy (four 0.062-inch K-wires in this case) are of secondary importance to understanding the profound importance of repairing the deep components of the TFC to the fovea in this patient. The critical concept was to shift the entire distal forearm unit medially, enabling anatomical restoration of the ligamentum subcruentum to the fovea and restoration of normal DRUJ mechanics. Figure 25-25E demonstrates the intraoperative technique of preparing the fovea for reattachment of the ligamentum subcruentum, installing the bone anchor (with additional 2-0 Fiberwire attached), and passing sutures through the TFC before pulling the deep fibers securely into the fovea. As seen in the postoperative radiograph (see Fig. 25-25E), two additional percutaneous 0.062-inch K-wires were passed through the distal ulna into the radius before tying the bone anchor sutures as tightly as possible. The K-wires maintain rigid stability of the DRUJ during the early postoperative healing process. All eight percutaneous K-wires seen in Figure 25-25E were removed 6 weeks after surgery. After rehabilitation the patient regained full, painless pronation/supination, with normal load-bearing capacity at the DRUJ. Her final radiograph is seen in Figure 25-25J.
Conclusions
I am hopeful that the reader now understands why the works of af Ekenstam and Hagert in 1985, and Schuind and associates, in 1991, deemed so controversial then, should now be considered corroborative. Special credit should also go to Dr. Carl-Goran Hagert, who recognized the reasons for our misunderstandings in 1994 and provided a clear explanation of how the different components of the TFC work in conjunction with each other, in providing functional stability at the DRUJ. The superficial radioulnar components of the TFC maintain stability of the hypovascular articular disc for load transmission from the medial side of the carpus to the pole of the ulna. The clinical manifestation of chronic, superphysiological load on the superficial components of the TFC is progressive deterioration of the articular disc, the ulnar pole, and, eventually, the lunatotriquetral joint, referred to by Milch in 194116 as “ulnocarpal abutment syndrome” and classified by Palmer as progressive degenerative lesions of the TFC.16 Deep peripheral tears of the TFC have an effect on DRUJ rotational stability that is quite different from the effects of central degenerative TFC tears classified by Palmer in 1989.
The deep components of the TFC (palmar and dorsal ligamentum subcruentum), with their obtuse and mechanically advantageous angle of attack from the palmar and dorsal medial edges of the distal radius to the ulnar fovea, principally guide the radius around a fixed ulna through a full functional arc of pronation/supination. That the DRUJ can be destabilized by rupture of the deep fibers of the TFC alone, with the superficial radioulnar ligaments still intact, is now well recognized. In the past 3 years we have treated 10 patients at the Indiana Hand Center with intraoperative documentation of ligamentum subcruentum avulsion from the ulnar fovea but a normal ulnocarpal arthroscopic examination, with intact superficial radioulnar ligaments and articular disc. Recent improvements in contrast MRI have made our presumptive diagnoses more clear, but the value of preoperative physical diagnostic maneuvers cannot be overstated. Bone anchoring of the avulsed ligamentum subcruentum to the ulnar fovea is now a regularly performed surgical procedure in our practice, in those cases in which provocative stress-testing of the ligamentum subcruentum has been positive. Certainly, the chronicity and magnitude of the patient’s symptoms, as well as a failure of conservative management, are factors that enhance the indications for surgical intervention.
1. Af Ekenstam F, Hagert CG. Anatomical studies on the geometry and stability of the distal radioulnar joint. Scand J Plast Reconstr Surg. 1985;19:17-25.
2. Bednar MS, Arnoczky SP, Weiland AJ. The microvasculature of the triangular fibrocartilage complex: its clinical significance. J Hand Surg [Am]. 1991;16:1101-1105.
3. Thiru-Pathi RG, Ferlic DC, Clayton ML, McClure DC. Arterial anatomy of the triangular fibrocartilage of the wrist and its clinical significance. J Hand Surg [Am]. 1986;11:258-263.
4. Palmer AK, Werner FW. Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res. 1984;187:26-35.
5. Schuind F, An KN, Berglund L, et al. The distal radioulnar ligaments: a biomechanical study. J Hand Surg [Am]. 1991;16:1106-1114.
6. Af Ekenstam FW, Palmer AK, Glisson RR. The load on the radius and ulna in different positions of the wrist and forearm: a cadaver study. Acta Orthop Scand. 1984;55:363-365.
7. Goldner JL, Hayes MG. Stabilization of the remaining ulna using one-half of the extensor carpi ulnaris tendon after resection of the distal ulna. Orthop Trans. 1979;3:330-331.
8. Spinner M, Kaplan EB. Extensor carpi ulnaris: its relationship to stability of the distal radioulnar joint. Clin Orthop Relat Res. 1970;68:124-128.
9. Ruby LK, Ferenz CC, Dell PC. The pronator quadratus interposition transfer: an adjunct to resection arthroplasty of the distal radioulnar joint. J Hand Surg [Am]. 1996;21:60-65.
10. Hotchkiss RN, An KN, Sowa DT, et al. An anatomic and mechanical study of the interosseous membrane of the forearm: pathomechanics of the proximal migration of the radius. J Hand Surg [Am]. 1989;14:256-261.
11. Kauer JMG. The articular disc of the hand. Acta Anat. 1975;93:590-605.
12. Henle J. Handbuch der Bänderlehre des Menschen. Braunschweig: Friedrich Vieweg; 1856.
13. Fick RA. Handbuch der Anatomie und Mechanik der Gelenke unter Berucksichtigung der bewegenden Muskeln. Vol 1. Anatomie der Gelenke. Jena: Fischer; 1904.
14. Hagert CG. Distal radius fracture and the distal radioulnar joint—anatomical considerations. Handchir Mikrochir Plast Chir. 1994;26:22-26.
15. Kleinman WB, Graham TJ. The distal radioulnar joint capsule: clinical anatomy and role in posttraumatic limitation of forearm rotation. J Hand Surg [Am]. 1998;23:588-599.
16. Milch H. Cuff resection of the ulna for malunited Colles’ fracture. J Bone Joint Surg. 1941;23:311-313.
17. Viegas SF, Pogue DJ, Patterson RM, Peterson PD. Effects of radioulnar instability on the radiocarpal joint: a biomechanical study. J Hand Surg [Am]. 1990;15:728-732.
18. Pogue DJ, Viegas SF, Patterson RM, et al. Effects of distal radius fracture malunion on wrist joint mechanics. J Hand Surg [Am]. 1990;15:721-727.
19. Palmer AK. Triangular fibrocartilage complex lesions: a classification. J Hand Surg [Am]. 1989;14:594-606.