Sports Medicine
In the United States, greater than 30 million (approximately one third) of school-aged children participate in organized sports.1 Sports-related injuries occur more frequently in the lower extremities compared with the upper extremities. This section will review acute and chronic sports injury patterns with an emphasis on entities that are unique in children. This section will cover multimodality imaging and emphasize important magnetic resonance imaging (MRI) features related to pediatric sports injuries. Acute fractures and dislocations are covered in Chapter 143.
Avulsion Injuries and Muscle Injuries
Etiology: Avulsion injuries or fractures may occur at muscle attachments to an apophysis or at ligamentous attachments to a chondro-osseous junction.
The musculoskeletal unit of the child is composed of the apophysis, tendon, myotendinous junction, and muscle belly. In the skeletally mature patient, the weakest component of the musculoskeletal unit is the myotendinous junction. In the skeletally immature patient, particularly during periods of rapid growth, the cartilaginous physeal equivalent region of the apophysis is the weakest component of the musculoskeletal unit.2 As a consequence, apophyseal avulsion injuries (Fig. 145-1), rather than myotendinous tears, may occur when the musculoskeletal unit is stressed.
Apophyseal injuries are more frequent in the lower extremity than in the upper extremity. In the lower extremity, the pelvis and knee are the most common sites for apophyseal avulsion injuries.3 Ligamentous avulsion injuries similarly are more common in the lower extremity than in the upper extremity.
After the apophysis, the next weakest component of the musculoskeletal unit is the myotendinous junction. Muscle tears most commonly occur at the myotendinous junctions. Myotendinous tears are an acute event during a physical activity in which a child can pinpoint the time (within seconds) in which the injury occurred. This should be differentiated from delayed onset muscle soreness (DOMS). DOMS is not related to a single event but may be caused by an activity with repetitive eccentric and concentric muscle contractions with no acute pain at the time of the activity. Instead, symptoms and pain usually are felt the following day after the activity.4
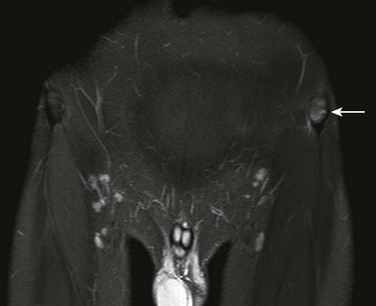
Imaging: In the acute setting, the displaced avulsion fracture fragment is present without proliferative callus formation present (see Fig. 145-1). During healing, proliferative callus will be seen, suggesting its subacute or chronic nature.
When radiographs are negative and no displaced fragment exists, an MRI scan may be obtained. MRI may demonstrate subtle edema of the apophysis and metaphyseal equivalent bone, physeal equivalent edema and widening, and adjacent soft tissue edema (e-Fig. 145-2). The term fracture should be used only when a linear displaced or nondisplaced fracture is present. When edema alone is present within the apophysis and adjacent soft tissues, the term avulsion injury should be used.
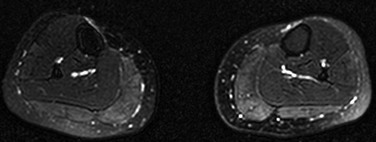
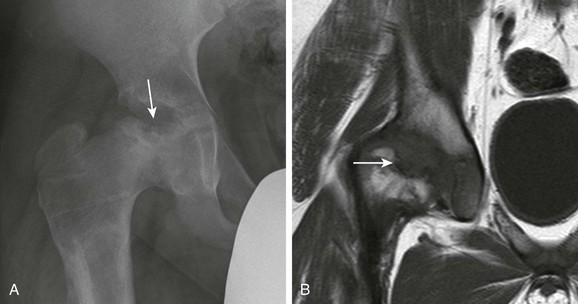
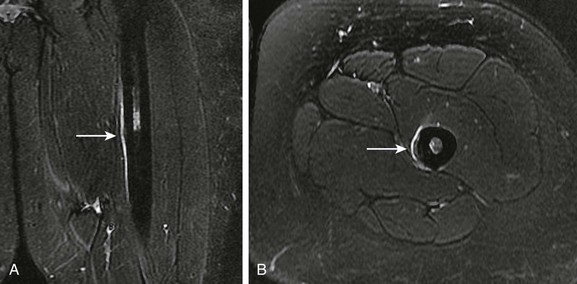
MRI may also demonstrate avulsion injuries and fractures at the level of the chondro-osseous junction (Fig. 145-3).
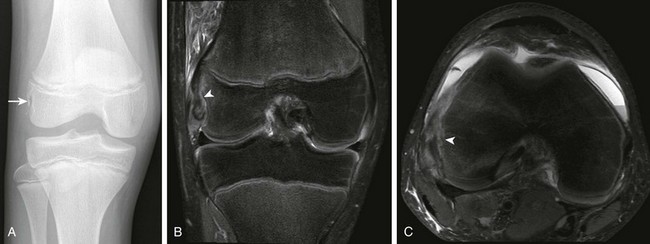
Figure 145-3 A 13-year-old boy with a popliteus origin chondro-osseous avulsion fracture (arrow).
A, An anteroposterior knee radiograph. B, Proton density fat-saturated coronal image. C, Proton density fat suppression axial image demonstrates chondro-osseous fracture line (arrowhead).
MRI is preferred for delineating the remainder of the musculoskeletal unit. When muscle edema is present related to trauma, three possible etiologies exist: (1) DOMS (Fig. 145-4), (2) direct muscle contusion (e-Fig. 145-5), and (3) myotendinous muscle tear (Fig. 145-6) (Table 145-1). With DOMS, MRI shows diffuse edema on fluid sensitive sequences without discrete fiber disruption. Direct muscle contusions shows similar changes to DOMS but are more focal in nature when injury is mild, with discrete fiber disruption and hematoma formation when the injury is severe. In the setting of muscle hematomas, these may mimic an intramuscular abscess. Gadolinium-enhanced, T1-weighted, fat-saturated imaging may demonstrate rim enhancement for both hematomas and intramuscular abscess. T1-weighted imaging without gadolinium may demonstrate T1-weighted hyperintense foci related to blood products and may suggest muscle hematoma and less likely intramuscular abscess with proteinaceous content. Myotendinous muscle tears may range from partial, with only some fibers disrupted at the level of the aponeurosis, to complete disruption with muscle fiber and aponeurosis retraction.
Table 145-1
Magnetic Resonance Imaging Appearance and Grading of Myotendinous Tears
| Grade 1 | Edema at the myotendinous junction |
| Grade 2 | Partial tearing at the myotendinous junction |
| Grade 3 | Complete tear at the myotendinous junction with tendon retraction |
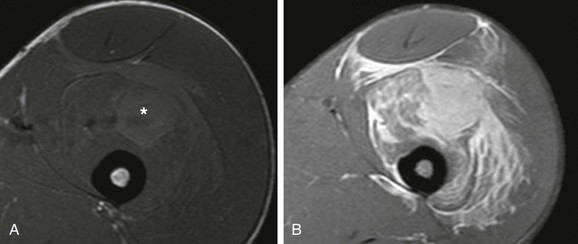
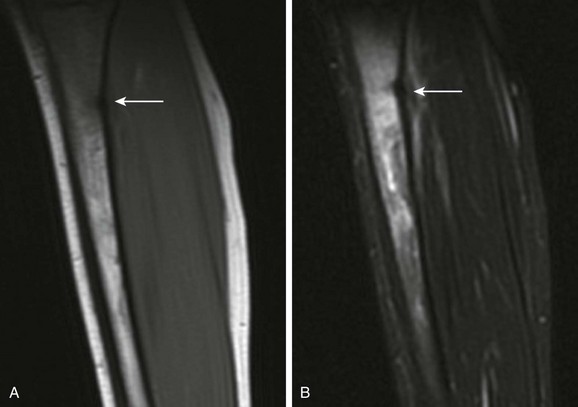
e-Figure 145-5 A 17-year-old boy with vastus intermedius direct muscle contusion.
A, A T1-weighted axial image demonstrates hyperintense material, consistent with blood products, located in the vastus intermedius muscle belly (asterisk). B, A T2-weighted fat suppression axial image demonstrates fiber muscle disruption and extensive infiltrative myositis and tearing of the vastus intermedius muscle fibers and deep fascial edema.
Treatment and Follow-up: Treatment varies, depending on the location of the apophyseal avulsion injury. In the pelvis, the majority of apophyseal avulsion injuries are treated conservatively with rest. Surgical reduction and fixation may be necessary when the avulsed fracture fragment is greater than 2 cm.3 During the healing phase, radiographs may be helpful to monitor callus formation and healing. Apophyseal avulsion fractures elsewhere are usually treated conservatively, and surgical reduction is based on degree of apophyseal displacement. For instance, medial epicondylar avulsion fractures are treated surgically when the displaced fragment is greater than 5 mm.5
Myotendinous tears are treated conservatively with 2 to 3 weeks of rest before returning to sport activities.4 DOMS is also treated conservatively and symptoms usually resolve within a week.
Hyperextension Injuries of the Knee
Etiology: The anterior compartment of the knee is composed of the quadriceps tendon, patellar bone, patella tendon, and tibial tuberosity. Patellar bone is a sesamoid equivalent for the quadriceps mechanism. Acute forceful concentric or eccentric contraction of the quadriceps muscle may lead to acute avulsion injuries of the inferior patellar pole (chondro-osseous avulsion injury, patellar sleeve fractures) and tibial tuberosity (apophyseal avulsion injury), as well as tendinopathy of the patella tendon. Sinding-Larsen-Johansson disease is the term used for chronic avulsive injuries affecting the inferior patellar pole. Osgood-Schlatter disease is the equivalent injury affecting the tibial tuberosity.1 When only a patella tendon tear is present, it is called jumper’s knee and tends to occur in patients who are skeletally mature. Sinding-Larsen-Johansson and Osgood-Schlatter diseases usually occur during adolescence and often affect both knees. Bone and tendon injuries often may occur in the same knee.
Imaging: Although imaging is helpful for the diagnosis of Sinding-Larsen-Johansson and Osgood-Schlatter diseases, the diagnosis for these chronic conditions is made clinically with radiographic confirmation of findings, not by imaging alone. Advanced imaging confirms the diagnosis and excludes alternative etiologies. MRI should not be performed routinely on these patients if radiography and clinical diagnosis confirm the disease.
Patellar sleeve fractures represent an acute avulsion fracture located along the inferior pole of the patella. This occurs at the chondro-osseous junction of the patella tendon origin. On radiography and MRI, a small linear or curvilinear fleck of bone may be identified (Fig. 145-7). On MRI, edema of the patellar bone, edema in the superior aspect of Hoffa’s fat pad, and peripatellar edema are often present in the acute setting. This should be differentiated from chronic repetitive avulsive injuries to the inferior patellar pole leading to Sinding-Larsen-Johansson disease. With Sinding-Larsen-Johansson disease, the inferior patellar bone has had time to remodel related to chronic avulsive injury. Therefore, on radiography and MRI, well-formed variable size ossicles may be seen (Fig. 145-8). On MRI, edema within the inferior pole ossicles is related to the acute or chronic nature of the injury.
Acute tibial tuberosity avulsion fractures results from forceful contraction of the patella tendon leading to a tibial tuberosity–sided linear or curvilinear avulsion fracture fragment at the level of the chondro-osseous junction (Fig. 145-9) or to uplifting of the entirety of the tibial tuberosity, with resultant Salter-Harris type injury with physeal equivalent widening (Fig. 145-10). On MRI, often, edema is seen within the tibial tuberosity, and this may extend posteriorly to involve the remainder of the tibial epiphysis. Inferior Hoffa’s fat pad and pretibial edema are often present. These changes should be differentiated from chronic repetitive avulsive injury affecting the tibial tuberosity and leading to Osgood-Schlatter disease. With Osgood-Schlatter disease, rather than linear avulsion fracture fragments, the tibial tuberosity and tibial tuberosity avulsion fragments have had time to remodel. Therefore, on radiography and MRI, well-formed variable size well-corticated ossicles may be seen (e-Fig. 145-11). On MRI, edema within the avulsed separate ossicles and tibial tuberosity are present and are related to the acute or chronic nature of the injury. In addition, edema within Hoffa’s fat pad and pretibial edema are often present as well.

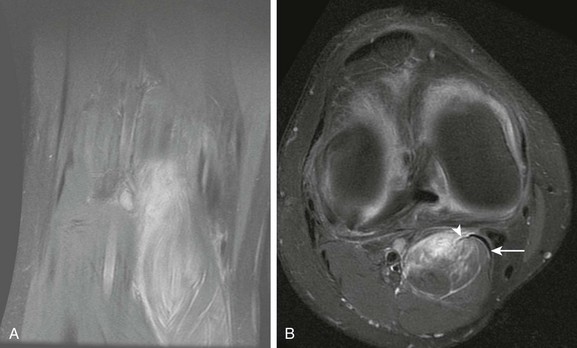
Figure 145-9 A T2-weighted fat suppression sagittal image from a 13-year-old boy demonstrates an acute nondisplaced partial tibial tuberosity avulsion fracture (arrow).
Note that some patella tendon fibers remain intact (arrowhead).
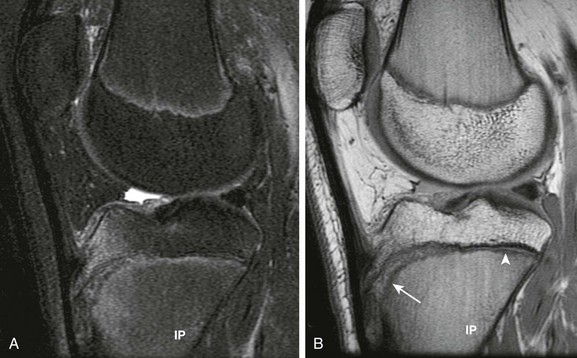
Figure 145-10 A 14-year-old girl with tibial tuberosity equivalent physeal widening.
A, A T2-weighted fat suppression sagittal image demonstrates diffuse edema of the tibial tuberosity, physis, and deep metaphyseal equivalent region of the tibia. B, A proton density sagittal image delineates physeal equivalent widening of the tibial tuberosity (arrow). Note the physeal equivalent widening compared with the normal posteriorly located tibial physis (arrowhead).

e-Figure 145-11 A 15-year-old with Osgood-Schlatter disease.
A, Lateral radiograph. B, Proton density sagittal image of the knee demonstrates tibial tuberosity fragmentation. C, A T2-weighted fat suppression sagittal image demonstrates edema of the tibial fragmentation (arrow) and adjacent Hoffa’s fat pad.
Patella tendinopathy and patellar tears (e-Fig. 145-12) may be evaluated by ultrasonography or MRI. On MRI, thickening of the tendon with longitudinally or transversely oriented tears may be seen as well as edema within the prepatellar soft tissues and Hoffa’s fat pad. MRI diagnosis of jumper’s knee should ideally be made on longer echo time sequences to avoid “magic angle artifact.”
Treatment and Follow-up: Sinding-Larsen-Johansson disease, Osgood-Schlatter disease, and jumper’s knee are all treated conservatively with rest. When displaced, acute avulsion fractures of the inferior patellar pole or tibial tuberosity may be treated by open reduction with patellar tendon reconstruction, particularly if patella alta is also present.6 For avulsion fractures, care should be made to determine if the fracture is complete, incomplete, displaced, or nondisplaced. If the avulsion fracture is incomplete (see Fig. 145-9), affected children may benefit from conservative nonsurgical treatment.
Patellar Dislocation and Patellofemoral Dysplasia
Etiology: The patella is a sesamoid equivalent bone of the quadriceps mechanism. Patellar bone has two primary facets: medial and lateral. The lateral facet is usually the dominant and larger facet, and articulates with the lateral aspect of the trochlear fossa. Patellar bone lies within the concave shaped femoral trochlear fossa. With knee flexion, the patella will concentrically locate within the trochlear fossa. With knee extension, patellar bone preferentially subluxes laterally in patients with or without underlying patellofemoral dysplasia because the lateral patellofemoral articulation is shallow compared with the medial articulation and the vastus lateralis activates when the knee is extended.
Multiple variables may predispose a patient to patellar dislocation. This includes a large Q-angle, muscle imbalance with dominant vastus lateralis musculature, patella alta, rotational abnormalities of the tibia and femur, and overall ligamentous laxity. The Q-angle is calculated by the angle derived from the intersection of two lines: (1) center of patella and anterosuperior iliac spine and (2) center of patella and tibial tuberosity. The normal Q-angle measures approximately 15 degrees. The Q-angle is usually larger in females. Larger Q-angles direct the quadriceps muscle vector force on the patella laterally. Patella alta occurs when the ratio of patellar tendon length to patellar bone length is greater than 1 : 2. Patellar bone captures within the trochlear groove with knee flexion. In the setting of patella alta, it takes relatively more knee flexion for the patellar bone to capture. Excessive external tibial torsion may also predispose a child to patellar dislocation, as well as increased femoral anteversion.7,8 The normal degree of external tibial torsion is approximately 28 degrees at age 4 years and increases to approximately 38 degrees at skeletal maturity.9 The normal degree of femoral anteversion is approximately 40 degrees at birth and approximately 15 degrees at skeletal maturity.
Imaging: Radiographs should be reviewed to identify loose bodies, subjective determination of patella alta, and patellofemoral dysplasia. The “sunrise view” is helpful to evaluate for patellar sleeve fractures for both acute (Fig. 145-13) and old injuries (e-Fig. 145-14). Acute patellar sleeve fractures are sliverlike, whereas old injuries are round and corticated. These patellar sleeve fractures occur along the medial pole and are a result of avulsion injury at the medial retinacular attachment to the chondro-osseous junction of the medial patellar pole. The sunrise view is also useful for evaluating for patellofemoral dysplasia. Features suggesting patellofemoral dysplasia include a lateral dominant patellar facet and a flat or even convex appearing trochlear fossa. With progressive patellofemoral dysplasia, the trochlear fossa becomes more convex in appearance and the patellar bone loses its normal angular appearance.

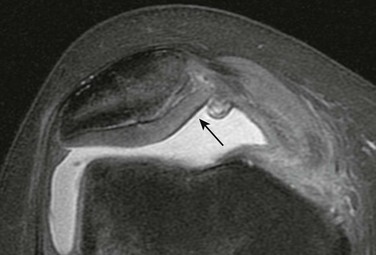
Figure 145-13 An 18-year-old with acute patellar dislocation, with acute, medial patellar sleeve fracture (arrow).
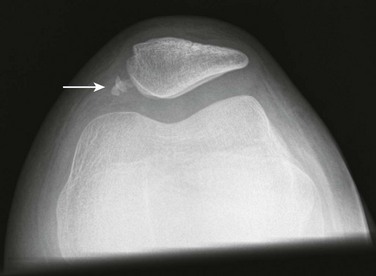
e-Figure 145-14 An 11-year-old girl with old, medial patellar sleeve fracture (arrow) caused by prior patellar dislocation.
These fracture fragments are corticated (indicative that they are old) in contrast to acute fracture fragments that are not yet corticated (see Fig. 145-13).
Computed tomography (CT) may be obtained in the workup of patellofemoral dysplasia. CT may be used to determine tibial and femoral version. As external tibial torsion and femoral anteversion increases, the child is at higher risk for patellar instability and tilt.7,8 CT may also be performed with the knees at various degrees of flexion (e-Fig. 145-15). The patella locates with increasing knee flexion and subluxes with increasing knee extension. Three separate CT acquisitions are obtained at different degrees of knee flexion (e.g., 45, 30, and 15 degrees). If the patella dislocates at 15 degrees but is located at 45 and 30 degrees, it is considered a mild degree of patellar dislocation. However, if the patella dislocates at 30 or 45 degrees of knee flexion, it is a more severe degree of patellar dislocation. CT for patellar dislocation should also be used to evaluate the degree of patellofemoral dysplasia and secondary patellofemoral osteoarthritis, with changes similar to what may be seen on sunrise-view radiographs. Lateralization of the tibial tuberosity should also be determined. This represents the distance between the midpoint of the tibial tuberosity and the deepest component of the trochlear groove on axial slices. If the tibial tuberosity is greater than 2 cm lateral with respect to the trochlear groove, a higher incidence of patellar instability exists.10
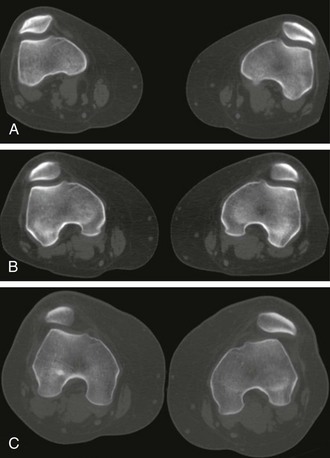
e-Figure 145-15 A dynamic computed tomography scan of bilateral patellofemoral joints at 45 degrees (A), 30 degrees (B), and 15 degrees (C) of knee flexion.
Note with progressive knee extension, the patellar subluxes and tilts laterally, left greater than right.
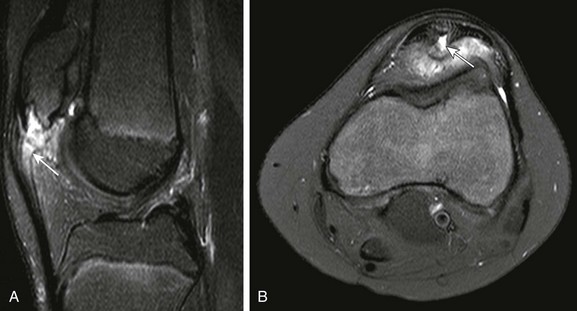
MRI complements radiography and CT findings. Sometimes, children are referred for knee pain, and the diagnosis of patellar dislocation and patellofemoral dysplasia may be first suspected on MRI. On MRI for acute patellar dislocation, characteristic bone contusions may be seen along the medial patellar pole and anterolateral femoral condyle (Fig. 145-16). The bone contusions occur in relation to relocation of the patella after patellar dislocation. Other findings that may be seen include patellar sleeve fractures, medial retinacular tears, cartilage injuries, and loose bodies. Patellofemoral dysplasia (Fig. 145-17) and secondary degenerative changes should also be assessed by MRI.
Treatment and Follow-up: Treatment for patellar dislocation should be approached from two perspectives: (1) treat biomechanical instability, which can be addressed by physical therapy and operative repair, and (2) treat mechanical symptoms related to sequelae from acute dislocation usually from loose bodies or chondral injuries.
Patients with first-time patellar dislocation and those with recurrent patellar dislocation are treated conservatively with physical therapy and bracing. The goal of treatment is to improve gluteal and vastus medialis muscle activity, which facilitates medial location of the patella.10 Should physical therapy not improve symptoms, surgical repair should be considered, although no one effective surgical technique has been advocated in the literature. Surgical approaches include lateral retinacular release, medial retinacular repair and reconstruction, trochleoplasty (deepen the sulcus), tibial tubercle transfers (medialization of the tibial tubercle), as well as rotational osteotomies to treat excessive tibial torsion and femoral version. The surgical goal is to facilitate patellar bone capture by the trochlear fossa and medialization of patellar biomechanical vector forces.
When loose bodies or cartilage injury is identified and the child has mechanical symptoms such as locking, arthroscopy may be performed to remove the loose bodies and perform cartilage debridement to stabilize and smoothen the patellofemoral articulation.10
Anterior Cruciate Ligament Complex Injuries
Etiology: The anterior cruciate ligament (ACL) complex is composed of the ACL, its femoral origin, and its tibial insertion. The femoral and tibial chondro-osseous attachments of the ACL complex are relatively weak in the skeletally immature, and are predisposed to chondro-osseous avulsion fractures.11 Chondro-osseous avulsion fractures occur far more commonly at the tibial eminence insertion compared with the femoral origin. The ACL is composed of two fiber bundles: the anteromedial and posterolateral bundles, which extend from the medial aspect of the lateral femoral condyle to the level of the tibial eminence.12 Coexisting full-thickness ACL tear and complete tibial eminence fractures are unusual since the force of injury usually is dissipated by either the ACL tear or the avulsion fracture. However, in most cases, arthroscopic evidence of ACL incomplete fiber tears is often present in the setting of a complete tibial eminence avulsion fracture. ACL tears are often seen in children with a narrow intercondylar notch, and ACL tibial eminence avulsion fractures tend to occur in children with a wider intercondylar notch.13,14
Imaging: Radiographic findings that may indicate an ACL complex injury includes Segond (e-Fig. 145-18) and tibial eminence avulsion fractures (Fig. 145-19). A Segond fracture represents an anteromedial capsular avulsion fracture at the chondro-osseous junction of the lateral tibial plateau. Tibial eminence avulsion fractures should be categorized as a single bone avulsion fracture or comminuted, since this may affect treatment strategies. Because of ligamentous instability related to an ACL deficient knee, anterior translation of the tibia may be present on the lateral view.
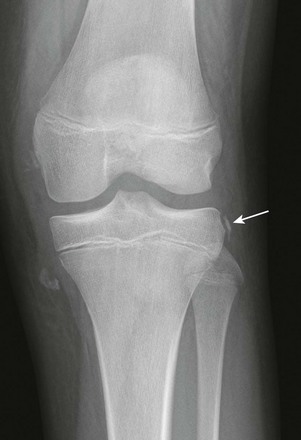
e-Figure 145-18 An 11-year-old girl with Segond fracture (arrow), as well as medial wall femoral condylar chondro-osseous fragments.
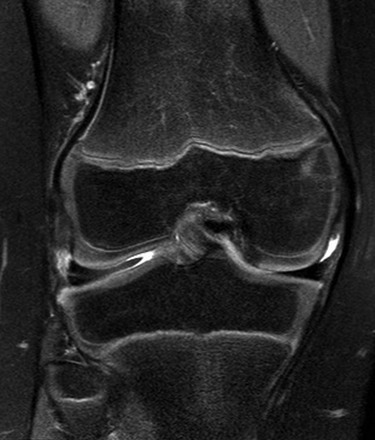
On MRI, identification of complete disruption of the ACL should be confirmed on all three orthogonal planes (Fig. 145-20). ACL tears should be subcategorized as partial (rare) versus full-thickness tears (more common). Some of the additional features to suggest ACL complex injuries are bone contusions related to anterior translation and twisting of the tibia, including anteromedial or anterolateral femoral condylar bone contusions, with kissing posteromedial or posterolateral tibial plateau contusions (see Fig. 145-20). When bone contusions are evident, a T1-weighted or proton-density sequence is useful for determining is the presence of an underlying subchondral fracture. When subchondral bone contusions are present, the presence or absence of overlying articular cartilage injury should be identified. Tibial eminence avulsion fractures are also demonstrated by MRI but are more readily identifiable on radiographs (see Fig. 145-19).

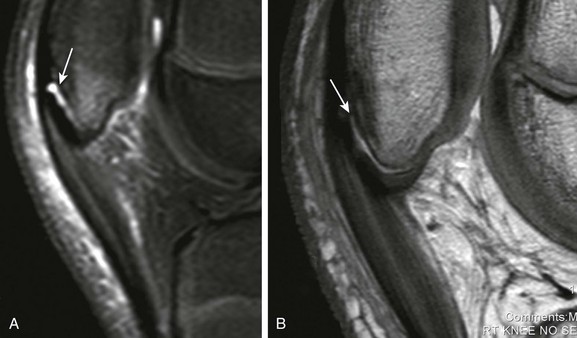
Figure 145-20 A 16-year-old boy with full thickness anterior cruciate ligament (ACL) tear.
A, Proton density sagittal image demonstrates full-thickness tear of the ACL near its femoral origin with residual tibial insertion fibers (arrow). B, Proton density fat suppression coronal image demonstrates full-thickness tear with residual femoral origin ACL fibers (arrowhead). C, A T2-weighted fat suppression sagittal image demonstrates characteristic kissing contusion pattern related to ACL mechanism injury (asterisk).
Additional findings on MRI include medial collateral ligament tears (e-Fig. 145-21) and meniscal tears. When describing medial collateral ligament tears, its location (femoral or tibial sided) must be identified and the presence of additional involvement of the medial meniscofemoral or medial meniscotibial ligament determined. Meniscal tears can be seen in up to 69% of ACL injuries in children (e-Fig. 145-22).15 The most common location for meniscal tears is the posterior horn of the lateral meniscus.

e-Figure 145-21 A 16-year-old boy with full thickness medial collateral ligament tear (arrow) with retraction from the tibial insertion.
Note disruption of meniscotibial and meniscofemoral ligaments as well.

e-Figure 145-22 A 14-year-old boy with peripheral vertical tear of the posterior horn of the lateral meniscus (arrows).
This should be distinguished from the meniscofemoral ligament that can simulate a tear because of its superior sulcus. Meniscofemoral sulci should only involve the peripheral aspect of the superior articular surface of the posterior horn of the lateral meniscus.
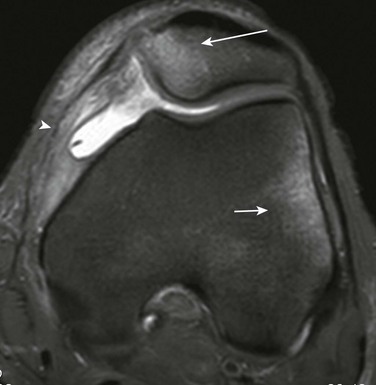
Classification of meniscal tears includes vertical (see e-Fig. 145-22), horizontal (e-Fig. 145-23), displaced (Fig. 145-24), and location (red or white zone) types. Vertical tears by definition extend from the superior to inferior articular surface. They are subclassified into radial, longitudinal, or parrot-beak tears. Horizontal tears usually extend to only one articular surface and are usually degenerative in nature. Displaced tears include bucket handle tears (see Fig. 145-24) and displaced free fragment tears. Bucket handle tears by definition are vertical longitudinal tears.

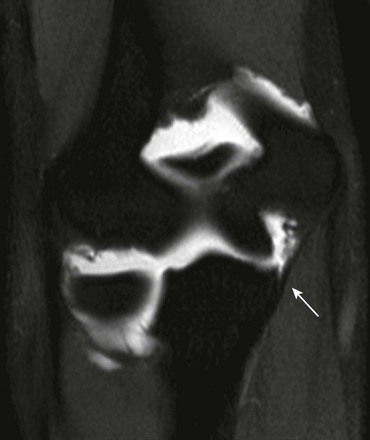
Figure 145-24 A 14-year-old girl with a lateral meniscus bucket handle tear.
Proton density sagittal image shows that the posterior horn of the lateral meniscus has flipped anteriorly (arrow), leading to a double anterior horn sign.
Treatment and Follow-up: Treatment for full-thickness ACL tears is surgical. The natural evolution of ACL deficient knees includes early osteoarthritis with cartilage injury and meniscal tears.16 Diagnosing high-grade partial ACL tears should be approached with extreme caution, since partial ACL tears may heal nonsurgically with appropriate physical therapy and rest. High-grade partial ACL tears are surgically significant if clinical examination suggests an ACL deficient knee or progressive instability of the knee occurs after initial injury. Surgical treatment includes primary ACL or tibial eminence repair, with physeal sparing, transepiphyseal, and transphyseal approaches. Boys over age 16 years, girls age 14 years or older, or those at Tanner stage 5 with closed or near closed physes, can be treated with conventional adult methods for ACL reconstruction.16 MRI is important presurgically to identify not only the ACL injury but also additional meniscal and cartilage injuries so that these areas can be repaired or débrided during ACL reconstruction.
Discoid Lateral Meniscus
Etiology: Discoid menisci most frequently affect the lateral meniscus. This represents a congenital enlargement of the lateral meniscus with respect to the lateral tibiofemoral joint compartment. The relative disproportionate size of the lateral meniscus alters the biomechanics of the lateral tibiofemoral compartment and the meniscus is predisposed to tears and degeneration. The utilization of approximate coverage of the lateral joint space is preferred compared with reference measurement of meniscal size in children. Using the adult reference of 12 mm width for normal meniscal size may be inaccurate in children, particularly in preschoolers who present with suspected lateral discoid menisci.17
The Watanabe arthroscopic classification of discoid lateral menisci includes (1) complete, (2) incomplete, and (3) Wrisberg variant.18 The Wrisberg variant is absence of normal posterior meniscocapsular fascicles and coronary ligaments, with the meniscofemoral ligament being the only attachment.19 The discoid lateral meniscus subtype of the Wrisberg variant describes the lack of posterior meniscocapsular attachment only and is not predicated on lateral meniscal size. Type 1 and 2 discoid lateral menisci are usually stable, and type 3 is unstable because of its lack of posterolateral meniscocapsular attachment.
Imaging: Radiographs may show relative widening of the lateral tibiofemoral joint space in the setting of a discoid lateral meniscus. Radiographs are not adequate to suggest or exclude the diagnosis, since the lateral joint space may be artifactually widened by patient positioning or weightbearing status.
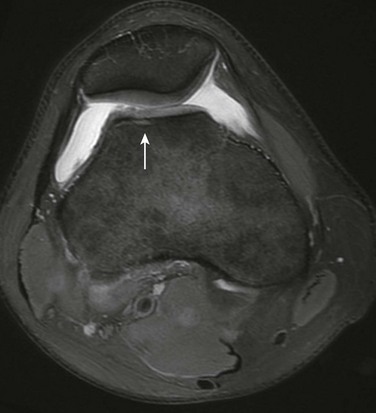
MRI is the optimal method for diagnosing a discoid lateral meniscus. All three orthogonal planes should be used to determine size of the lateral meniscus and degree of coverage of the lateral tibiofemoral joint compartment. When a discoid lateral meniscus is present, it can be partial (e-Fig. 145-25), complete (Fig. 145-26), or a Wrisberg variant. Counting sagittal slices to determine meniscal size is not useful, since no meniscal size references are available for children. The Wrisberg variant may be suggested when normal fascicles connecting the posterior horn of the lateral meniscus with the capsule are absent, independent of the size and shape of the lateral meniscus.
e-Figure 145-25 A 6-year-old boy with a partial discoid lateral meniscus.
It is important to describe the discoid lateral meniscus morphology, including presence or absence of tears or degeneration, and the nature of the discoid morphology. Discoid lateral meniscus may be uniformly enlarged or may be asymmetrically enlarged with a dominant posterior, midbody, or anterior horn.19
Treatment and Follow-up: Asymptomatic discoid lateral meniscus is usually observed. Treatment of symptomatic discoid lateral meniscus is surgical. Discoid lateral menisci are usually trimmed and saucerized to conform to the expected normal size and shape of the lateral meniscus and any tears that may also be present are repaired. Tears are débrided and trimmed until a stable margin is created.
Osteochondral Injuries
Etiology: Osteochondral lesions represent a broad spectrum of acute or chronic injuries with variable involvement of the articular and epiphyseal cartilage, spherical growth plate, and epiphyseal ossification center. Osteochondral lesions are separated into two basic lesions: (1) acute osteochondral fractures and (2) osteochondritis dissecans. Osteochondritis dissecans results from chronic repetitive injury.
The two types of osteochondritis dissecans are the juvenile and adult types.20 Juvenile osteochondritis dissecans tends to involve epiphyseal and spherical growth plates with either growth disturbance or injury to the epiphyseal ossification center. These tend to spontaneously heal. Adult osteochondritis dissecans affects articular cartilage and the epiphyseal bone. These lesions occur when the epiphyseal ossification is mature and usually only articular cartilage remains; they less commonly heal spontaneously and are more likely to be unstable compared with the juvenile variant.
Osteochondritis dissecans most commonly affects the knee but also can occur in the ankle and elbow (Table 145-2). These locations often have different prognostic significance, symptoms, and underlying etiology. For instance, osteochondritis dissecans of the talus tends to be asymptomatic and incidentally noted when the medial talar dome is involved, whereas lateral talar dome lesions tend to be symptomatic. At the level of the elbow, capitellar osteochondritis dissecans often is seen in throwing athletes. Because of repetitive valgus loading of the elbow, capitellar osteochondritis dissecans occurs related to repetitive compressive forces of the radial head abutting the capitellum in the lateral elbow compartment.
Table 145-2
Common Locations for Osteochondritis Dissecans
| Location of Osteochondritis Dissecans | Most Common Areas | Less Common Areas |
| Elbow | Capitellum | Radial head |
| Knee | Lateral aspect of the medial femoral condyle | Lateral femoral condyle, trochlear fossa, patella |
| Ankle | Medial talar dome | Lateral talar dome, midtalar dome |
Osteochondritis dissecans may also occur as a secondary process when the underlying epiphyseal bone is abnormal, as can be seen in the setting of Perthes disease (e-Fig. 145-27).
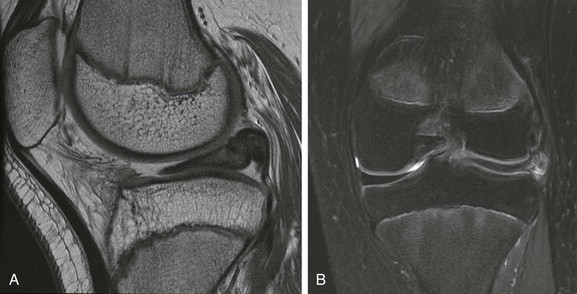
Imaging: Radiography should be the first line of imaging for osteochondral lesions. Purely cartilaginous lesions are better evaluated by MRI. In osteochondritis dissecans, subchondral fragmentation may be seen (Fig. 145-28). Tunnel views are often ordered in the evaluation of osteochondritis dissecans of the knee, but these are often misleading, since they delineate the posterior femoral condylar area in which normal femoral condylar irregularities are usually seen (Fig. 145-29).
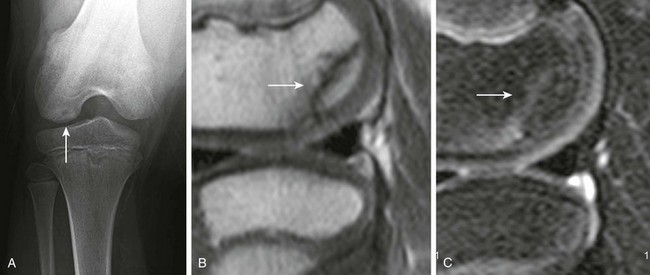
Figure 145-29 A 10-year-old boy with normal femoral condylar irregularity.
Magnetic resonance imaging of normal femoral condylar irregularities. A, Tunnel view demonstrates lateral femoral condylar subchondral irregularities (arrow). B, Proton density sagittal image. C, A T2-weighted fat suppression sagittal image demonstrates subchondral semilunar sharp demarcation between the condylar irregularity and epiphyseal parent bone (arrow). Because edema of the subchondral irregularity is not present and because the overlying articular cartilage and spherical growth plate are intact, this is considered a normal finding, not osteochondritis dissecans.
Acute chondral or osteochondral fractures are classified as partial (Fig. 145-30), full-thickness (Fig. 145-31), or delamination injuries (Fig. 145-32). When only cartilage is involved, these should technically be referred to as acute chondral fractures (see Fig. 145-30). The presence or absence of a chondral or osteochondral loose body should be documented when reporting an osteochondral injury.
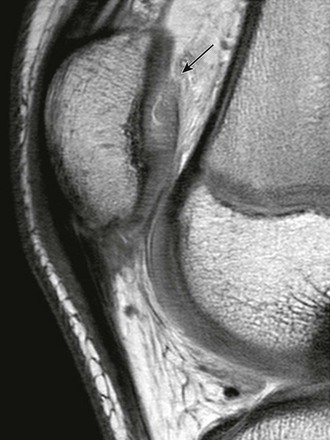
Figure 145-30 A proton density sagittal image demonstrates acute partial thickness cartilage injury (arrow) of the patella.
Osteochondritis dissecans are classified as unstable (Fig. 145-33) or stable (Fig. 145-34). Determining instability is more of an issue related to adult type osteochondritis dissecans, since in most cases, juvenile type osteochondritis dissecans is stable. Instability is suggested when fluid insinuates between the parent bone and osteochondritis dissecans (see Fig. 145-33), junctional cysts are present, the overlying cartilage is deficient, or loose bodies are present. Juvenile osteochondritis dissecans may have features of instability on MRI, but unlike adolescent and adult patients with the same lesion, they are more likely to spontaneously heal without surgical intervention, most likely because their spherical growth plate remains open.

Figure 145-34 A 13-year-old boy with lateral femoral condylar stable osteochondritis dissecans.
A, A T1-weighted coronal image. B, A proton density fat suppression coronal image demonstrates a well-demarcated osteochondritis dissecans with edema and tiny fluid lakes (arrow), but without discrete linear fluid signal to suggest instability.
Osteochondritis dissecans should be differentiated from normal condylar fragmentation, which is usually identified along the far posterior, non-weightbearing portion of the femoral condyles (see Fig. 145-29).
Treatment: Nonsurgical therapy is recommended when imaging features suggest stability. Juvenile osteochondritis dissecans and osteochondritis dissecans in patients with an open physis are most likely to heal spontaneously, compared with osteochondritis dissecans in older children.20 Surgical management includes arthroscopic drilling or microfracture methods to improve blood supply and healing, removal of any potential loose bodies, autologous osteochondral plugs, and autologous chondrocyte implantation are some methods used to treat unstable osteochondritis dissecans.20
Throwing Injuries
Etiology: “Little league shoulder” is an overuse injury that may occur with throwing activities, leading to a chronic Salter-Harris I injury of the proximal humerus.21 The physeal injury occurs related to rotational torque created during throwing.
Little league elbow represents a constellation of medial and lateral compartment soft tissue, cartilage, and bone injuries related to throwing. With overhead throwing, repetitive elbow valgus stress occurs and causes tensile forces along the medial joint line and compressive forces along the lateral joint line. Along the medial joint line, this results in medial epicondylar apophysitis and medial epicondylar avulsion fractures in younger children and anterior band ulnar collateral ligament injuries in adolescents who are skeletally mature.22 Along the lateral joint line, repetitive compressive forces lead to osteochondral lesions of the capitellum, and less frequently osteochondral lesions of the radial head. In younger children, Panner disease may result, rather than discrete osteochondral lesions of the capitellum.
Imaging: Radiographs of little league shoulder manifests with proximal physeal widening, juxtaphyseal metaphyseal fraying (Fig. 145-35), or proximal humeral metaphyseal periostitis. Imaging the contralateral asymptomatic shoulder may be necessary when the only finding present is physeal widening. This should be differentiated from physiologic proximal humeral physeal widening related to growth spurts. Physiologic proximal humeral physeal widening should be bilateral and symmetric.
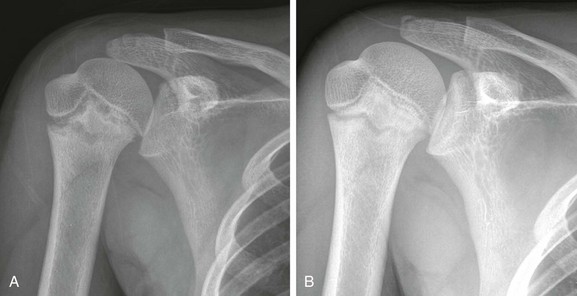
Figure 145-35 A 12-year-old with “Little League” shoulder.
A, An anteroposterior radiograph at presentation demonstrates proximal humeral physeal widening and metaphyseal fraying. B, An anteroposterior radiograph 3 months later shows resolution with rest.
Radiographic findings related to throwing injuries of the elbow include medial epicondylar avulsion fractures (Fig. 145-36). The avulsion injury may alternatively occur at the level of the chondro-osseous junction of the medial epicondyle with an intact medial epicondylar physeal equivalent region (e-Fig. 145-37). Radiographic features of capitellar osteochondritis dissecans include subchondral lucency (Fig. 145-38), fragmentation, and intraarticular loose bodies.

Figure 145-38 A 14-year-old boy with subchondral lucency and irregularity consistent with capitellar osteochondritis dissecans (arrow).

e-Figure 145-37 An 8-year-old boy with medial epicondylar chondro-osseous avulsion fracture (arrow).
When the medial epicondylar ossification center is disrupted, a chondro-osseous avulsion fracture, rather than a physeal equivalent avulsion fracture, may be suggested.
When radiographs are negative for medial epicondylar avulsion fractures, MRI may be helpful for evaluation of medial epicondylar pain. On MRI, diffuse marrow edema may be seen in the medial epicondyle and adjacent soft tissue. In older adolescents who are skeletally mature, common flexor tendon tears and ulnar collateral ligament tears are more commonly seen. The most common ligament that is torn is the anterior band of the ulnar collateral ligament at its insertion on the sublime tubercle of the ulna which is best evaluated by magnetic resonance arthrography (e-Fig. 145-39).
Treatment: Little league shoulder is treated nonsurgically with rest and activity modification. Surgical treatment is not indicated.21
For the elbow, medial epicondylitis and Panner disease are treated nonsurgically. Medial epicondylar avulsion fractures are surgically reduced if greater than 2 mm displacement exists. Anterior band ulnar collateral ligament tears are treated conservatively in most instances. In high-level athletes, reconstruction with tendon autograft may be performed.22 Osteochondritis dissecans of the capitellum are surgically treated (debridement, microfracture technique) if MRI features of instability are present.
Internal Derangement of the Hip
Etiology: Femoroacetabular impingement describes a constellation of femoral head or acetabular anatomic deformities causing hip joint incongruity that may lead to early osteoarthritis and labral tears. Femoral-sided deformities are classified as cam-type impingement, and acetabular-sided deformities are classified as pincer-type impingement. Usually both cam-type and pincer-type impingements coexist.
The diagnosis of femoroacetabular impingement is controversial, since many patients may have the anatomic deformity present and yet be asymptomatic.23,24 The diagnosis of femoroacetabular impingement may be suggested when positive clinical symptoms such as pain with hip flexion and hip internal rotation, as well as imaging findings of femoroacetabular impingement are present.
Common etiologies for cam-type femoroacetabular impingement in children include Perthes disease and slipped capital femoral epiphysis (SCFE).25 Perthes disease is a primary cam-type femoroacetabular impingement because the femoral head becomes aspherical. A secondary pincer-type femoroacetabular impingement may occur because the acetabulum is relatively too large compared with the aspherical small femoral head. SCFE may lead to an abnormal femoral head–neck offset with a cam-type femoroacetabular bump, which may impinge on the labral acetabular rim, leading to labral tears and acetabular chondral injuries. In more severe cases, a “pistol grip” deformity (loss of the normal concavity of the lateral femoral neck) may occur.
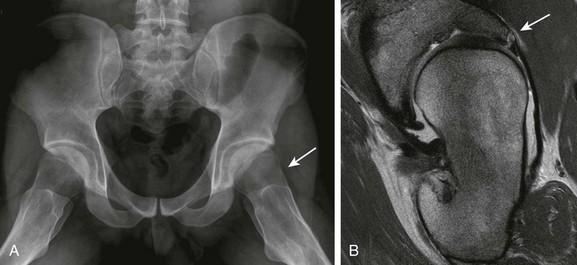
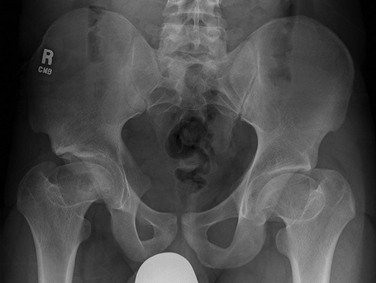
Developmental dysplasia of the hip (DDH) may cause a pincer-type impingement, cam-type impingement, or a combination of both. Cam-type femoroacetabular impingement results from a size mismatch between a small dysplastic acetabular cup and relatively large femoral head (Fig. 145-40). Subtrochanter varus osteotomy to relocate the hip may further exacerbate a cam-type impingement. Alternatively, periacetabular osteotomies such as a Salter osteotomy may increase the acetabular coverage, resulting in a pincer-type deformity.

Figure 145-40 A 19-year-old girl with left-sided untreated developmental dysplasia of the hip.
A T2-weighted fat suppression coronal sequence demonstrates size mismatch of relatively large femoral head and small acetabular fossa leading to cam-type impingement with resultant early labral degeneration with paralabral cysts (arrow).
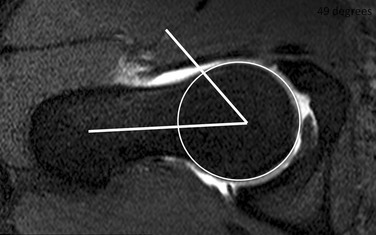
Imaging: Radiographic features of cam-type femoroacetabular impingement include junctional osteophytes at the level of the head–neck junction (Fig. 145-41). On MRI, anterosuperior labral tears are most frequently related to cam-type femoroacetabular deformities (Fig. 145-42). More obvious deformities leading to cam-type femoroacetabular impingement include Perthes disease (e-Fig. 145-43) and DDH (see Fig. 145-40). To assess labral tears, magnetic resonance arthrography with direct injection of diluted gadolinium is necessary.
1. Drawing a best-fit circle around the femoral head outlining the cortical margin
2. Drawing a parallel line with respect to the femoral neck terminating at the center of the circle
3. Drawing a line from the center of the circle and where the femoral head or neck protrudes from the circle
4. Calculating an angle between lines created from item 2 and 3 (Fig. 145-44)
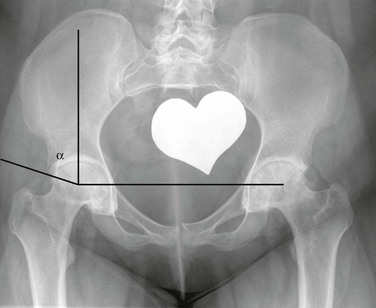
Pincer femoroacetabular impingement changes identified on radiography include the cross-over sign (Fig. 145-45) and a center edge angle greater than 29 degrees (e-Fig. 145-46). On frontal radiographs of the pelvis, the anterior acetabular wall is normally more medial with respect to the posterior acetabular wall (Fig. 145-47). The cross-over sign occurs when the anterior and posterior acetabular wall lines intersect, indicative of acetabular retroversion (see Fig. 145-45). The normal acetabulum is usually in 19 degrees of anteversion in adult patients.26 With acetabular retroversion, anterior overcoverage of the femoral head occurs. On CT or MRI, acetabular version should be calculated at the center of the hip joint.
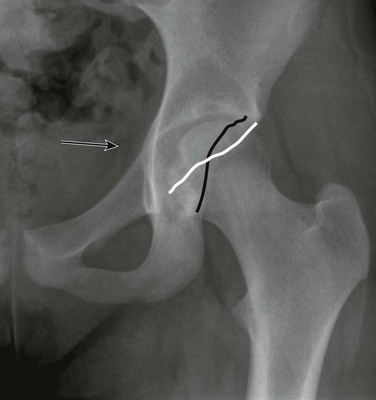
Figure 145-45 A radiograph of the cross-over sign indicative of acetabular retroversion.
The white line represents the anterior acetabular wall, the black line represents the posterior acetabular wall. Note the ischial spine sign is present as well (arrow), an additional indicator of a pincer deformity.

Figure 145-47 A normal anteroposterior radiograph of the hip showing no cross-over sign.
The white line represents the anterior acetabular wall, the black line represents the posterior acetabular wall.
Treatment: Treatment is predicated on symptoms, not on the degree of imaging deformity. Surgical treatment may be indicated when the child has positive clinical findings for impingement with supportive imaging features. Treatment focuses on surgically removing the anatomic cause of the impingement deformity to improve acetabular and femoral head joint congruity so that the acetabulum and the femoral head–neck junction do not abnormally abut during normal range of hip motion.27 This includes removing cam-type femoroacetabular osteophytes along the femoral head–neck junction as well as reshaping the femoral head to conform to a spherical shape and debridement of any labral tears or chondral injuries that may be present. This can be approached from an arthroscopic technique or an open technique. For pincer-type femoroacetabular deformity related to acetabular retroversion, a periacetabular rotational osteotomy may be performed to decrease the amount of anterior overcoverage.
Stress Injuries of Bone
Etiology: A fatigue fracture occurs when supraphysiologic repetitive stress is applied to normal bone. Insufficiency fractures occur when normal stress is applied to abnormal osteopenic bone.28 Stress injuries to bone can occur on either the compressive side or the tensile side of bone, leading to trabecular injury. A spectrum of bone changes may occur prior to the time a discrete fracture line may be seen on a radiograph or a cross-sectional image. These changes include periosteal edema, marrow edema, cortical edema, and microfractures (occult fractures not visible on imaging). With proper training, bone and muscle physiologic adaptation to repetitive stress is protective and may prevent stress reaction and stress fractures to bone.
Risk factors for stress injuries to bone include inadequate or improper athletic training, postpubertal females (female athlete triad: (1) menstrual irregularity, (2) disordered eating, (3) osteoporosis), and abnormal biophysical geometry of the child such as leg length discrepancies, varus alignment, abnormal femoral version, and pes cavus.29
Symptoms related to stress fractures are not present at rest but occur with physical activity.29 Shin splints, or medial tibial stress syndrome, is a vague term to describe pain that occurs over the posteromedial aspect of the distal third of the tibia.30 Proposed etiologies include muscle attachment inflammation, fascial edema, posterior compartment syndrome, and tibial stress fractures. Because of its nonspecific broad definition, shin splints should be reserved as a clinical diagnosis, not a radiologic diagnosis.
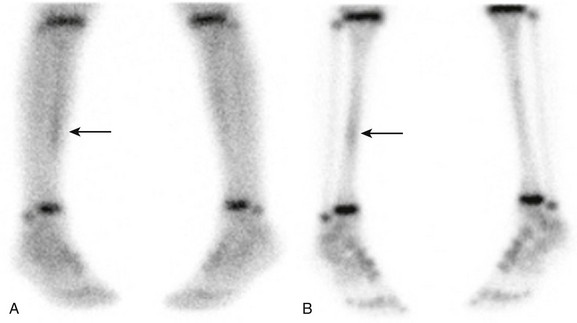
Imaging: With radiography, the spectrum of stress reaction to bone includes normal (most common), periostitis, and discrete fracture. Radiographs are the first line of imaging when suspected fracture is present. Bone scintigraphy and MRI are complementary tools when radiographs are normal.
With technetium-99m scintigraphy, a three-phase bone scan should be performed. With acute fractures all three phases are abnormal due to hyperemia (Fig. 145-48). When stress fractures are subacute or chronic, only the delayed phases may be abnormal, with no abnormal uptake during the blood-flow and blood-pool phases. Bone scintigraphy alone is limited in the evaluation of stress fractures of bone because it only measures osteoblastic activity, which can be seen in nontraumatic entities such as osteomyelitis and primary bone neoplasms. Therefore, bone scintigraphy should always be interpreted in conjunction with radiography.
MRI grading for bone stress injuries includes the spectrum from isolated periosteal edema (Fig. 145-49) to a true fracture (Fig. 145-50) (Table 145-3).29 MRI may also suggest alternative soft tissue etiologies for symptoms such as muscle tears or DOMS.
Table 145-3
Magnetic Resonance Grading of Stress Injuries to Bone
| Grade | T2 | T1 |
| 0 | Normal | Normal |
| 1 | Periosteal edema, no marrow edema | Normal |
| 2 | Periosteal edema, marrow edema | Normal |
| 3 | Periosteal edema, marrow edema | Periosteal edema, marrow edema |
| 4 | Fracture line present | Fracture line present |
Adapted from Fredericson M, Jennings F, Beaulieu C, et al. Stress fractures in athletes. Top Magn Reson Imaging. 2006;17(5):309-325.
Treatment: Treatment will vary, depending on location of fractures and symptoms. For nondisplaced stress fractures, treatment includes local pain control, including physical therapy and nonsteroidal antiinflammatory drugs. Weightbearing for normal activities is allowed. Eventually, return to athletic activity may begin if the child is pain-free for 10 to 14 days.29
References
1. Davis, KW. Imaging sports injuries: lower extremities. Radiol Clin N Am. 2010;48:1213–1235.
2. Ecklund, K. Magnetic resonance imaging of pediatric musculoskeletal trauma. Top Magnet Reson Imaging. 2002;13(4):203–218.
3. Sanders, TG, Zlatkin, MB. Avulsion injuries of the pelvis. Semin Musculoskelet Radiol. 2008;12:42–53.
4. Boutin, RD, Fritz, RC, Steinbach, LS. Imaging of sports-related muscle injuries. Radiol Clin North Am. 2002;40:333–362.
5. Cain, EL, Dugas, JR, Wolf, RS, et al. Elbow injuries in throwing athletes: a current concepts review. Am J Sports Med. 2003;31(4):621–635.
6. Gottsegen, CJ, Eyer, BA, White, EA, et al. Avulsion fractures of the knee: imaging findings and clinical significance. Radiographics. 2008;28(6):1755–1770.
7. Cameron, JC, Saha, S. External tibial torsion: an underrecognized cause of recurrent patellar dislocation. Clin Orthop Relat Res. 1996;328:177–184.
8. Boden, BP, Pearsall, AW, Garrett, WE, et al. Patellofemoral instability: evaluation and management. J Am Acad Orthop Surg. 1997;5(1):47–57.
9. Kristiansen, LP, Gunderson, RB, Steen, H, et al. The normal development of tibial torsion. Skeletal Rad. 2001;30(9):519–522.
10. Colvin, AC, West, RV. Patellar instability. J Bone Joint Surg Am. 2008;90:2751–2762.
11. Prince, JS, Laor, T, Bean, JA. MRI of anterior cruciate ligament injuries and associated findings in the pediatric knee: changes with skeletal maturation. AJR. 2005;185:756–762.
12. Milewski, MM, Sanders, TG, Miller, MD. MRI-arthroscopy correlation: the knee. J Bone Joint Surg Am. 2011;93(A):1735–1745.
13. Kocher, MS, Mandiga, R, Klingele, K, et al. Anterior cruciate ligament injury versus tibial spine fracture in the skeletally immature knee. J Pediatr Orthop. 2004;24(2):185–188.
14. Domzalski, M, Grzelak, P, Gabos, P. Risk factors for anterior cruciate ligament injury in skeletally immature patients: analysis of intercondylar notch width using magnetic resonance imaging. Int orthopaed. 2010;34:703–707.
15. Samora, WP, Palmer, R, Klingele, KE. Meniscal pathology associated with acute anterior cruciate ligament tears in patients with open physes. J Pediatr Orthop. 2011;31(3):272–276.
16. Schub, D, Saluan, P. Anterior cruciate ligament injuries in the young athlete: evaluation and treatment. Sports Med Arthrosc Rev. 2011;19(1):34–43.
17. Kelly, BT, Green, DW. Discoid lateral meniscus in children. Curr Opin Pediatr. 2002;14:54–61.
18. Watanabe, M, Takada, S, Ikeuchi, H. Atlas of arthroscopy. Tokyo: Igaku-Shoin; 1969.
19. Singh, K, Helms, CA, Jacobs, MT, et al. MRI appearance of Wrisberg variant of discoid lateral meniscus. AJR. 2006;187:384–387.
20. Kocher, MS, Tucker, R, Ganley, TJ, et al. Management of osteochondritis dissecans of the knee: current concepts review. Am J Sports Med. 2006;34(7):1181–1191.
21. Osbahr, DC, Kim, HJ, Dugas, JR. Little league shoulder. Curr Opin Pediatr. 2010;22:35–40.
22. Kijowski, R, Tuite, MJ. Pediatric throwing injuries of the elbow. Semin Musculoskelet Radiol. 2010;14:419–429.
23. Jung, KA, Restrpo, C, Hellman, M, et al. The prevalence of cam-type femoroacetabular deformity in asymptomatic adults. J Bone Joint Surg Br. 2011;93-B:1303–1307.
24. Laborie, LB, Lehmann, TG, Engesaeter, IO, et al. Prevalence of radiographic findings thought to be associated with femoroacetabular impingement in a population-based cohort of 2081 healthy young adults. Radiology. 2011;260:494–502.
25. Kassarjian, A, Belzile, E. Femoroacetabular impingement: presentation, diagnosis, and management. Semin Musculoskelet Radiol. 2008;12(2):136–145.
26. Dandachli, W, Ul Islam, S, Tippet, R, et al. Analysis of acetabular version in the native hip: comparison between 2D axial CT and 3D CT measurements. Skeletal Radiol. 2011;40:877–883.
27. Ganz, R, Parvizi, J, Beck, M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120.
28. Navas, A, Kassarjian, A. Bone marrow changes in stress injuries. Semin Musculoskelet Radiol. 2011;15(3):183–197.
29. Fredericson, M, Jennings, F, Beaulieu, C, et al. Stress fractures in athletes. Top Magn Reson Imaging. 2006;17(5):309–325.
30. Wilder, RP, Sethi, S. Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med. 2004;23:55–81.