CHAPTER 11 Splints and Bracing at the Elbow
INTRODUCTION
Elbow splints are frequently employed at the elbow and function in several capacities: protection both static and dynamic, to deliver flexion or extension torque. Specifically, the four types of braces or splints used in the postoperative and postinjury management of the elbow include resting and hinged splints, and dynamic and static adjustable splints.10
STATIC AND PROTECTIVE SPLINTS
Prophylactic bracing is occasionally employed at the elbow, typically to avoid excessive extension in the athlete.9 Further static splinting for the elbow is commonly used for short periods as a protective measure after injury or surgery. Previously used commonly in those with rheumatoid arthritis, largely because of the effectiveness of disease remitting agents, this type of splinting is uncommonly indicated today (Fig. 11-1).
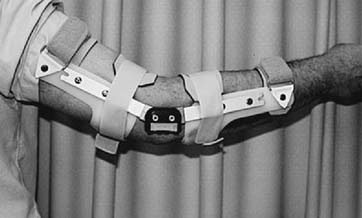
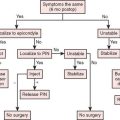
For the unstable elbow a hinged splint is used (Fig. 11-2). By initially locking the hinge, the same device can be used as a resting static splint; some designs allow conversion to a movable stabilizing device. Hinged splints allow active motion and are employed primarily for ligament healing. Occasionally, a hinged brace is prescribed for the resected elbow, but compliance is variable, and I rarely use this type of device.
ELBOW STIFFNESS
The most common complication of elbow injury, and even in some arthritic conditions, is stiffness. The most important means of avoiding this after a fracture is rigid fixation accompanied by early motion of the joint (see Chapter 22). After fracture dislocation, it has been demonstrated that immobilization lasting for more than 4 weeks resulted in less satisfactory outcome in each patient,2 and despite the recognized value of early motion after injury or surgery stiffness of the elbow remains a common problem in the orthopedic practice. Unfortunately, in the author’s experience the use of aggressive physical therapy to address post-traumatic stiffness is not always successful and, in fact, as often as not, makes the contracture worse. This justifies the use of splinting in this clinical setting, but to understand the rationale of splinting for this condition, it is necessary to understand the physiology of the process.
PATHOLOGY OF ELBOW CONTRACTURE
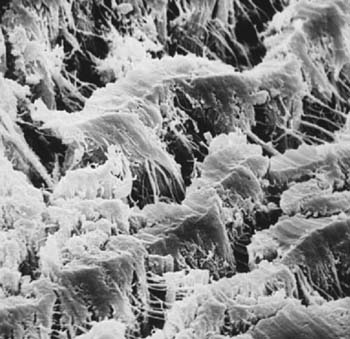
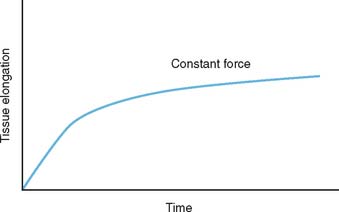
The exact reason that the elbow is so prone to joint contracture is not known with certainty. What is recognized is that the elbow is one of the most congruous joints in the body (see Chapter 2). Normally, the capsule is translucent, but with insult, it undergoes a marked hypertrophy and extensive cross-linking of the fibrils, as demonstrated on scanning electron microscopy (Fig. 11-3). In some instances, a severe elbow contracture has been observed after trivial insult or such as “strain” without fracture or dislocation. Under these circumstances, the elbow may contract rapidly, often within 2 to 3 weeks. An explanation of the rapid development of elbow contracture may be provided by the basic investigations on wound contracture. Experimental data demonstrate that dermal wounds undergo approximately 80% of the anticipated contracture within the first 3 weeks1 (Fig. 11-4).
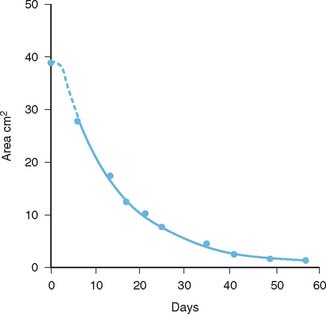
FIGURE 11-4 Experimental data showing that the majority of tissue contracture occurs in the first 3 weeks.
(With permission from Billingham, R. E., and Russell, P. S.: Studies on wound healing, with special reference to the phenomenon of contracture in experimental wounds in rabbits’ skin. Ann. Surg. 144:961, 1956, p. 964.)
Continuous motion, if properly used, has been shown to be an important adjunct to successfully alter this tendency and hence prevent contracture (see Chapter 10).
MANAGEMENT OF ELBOW STIFFNESS
PHYSICAL THERAPY
Physical therapy must be executed with extreme caution in the post-traumatic or inflamed elbow. The reason for this is that passive stretch, in and of itself, can introduce the very inflammation that one is trying to treat in the course of the therapy. Inflammation results in contracture and thus is an obstacle to the treatment goal. A well-trained experienced physical therapist who understands this principle can be of value, especially to assist in addressing concurrent shoulder and wrist stiffness. Such expertise is not possible in the author’s practice; therefore, I have never prescribed physical therapy for a patient of mine with elbow stiffness.
RESTORATIVE SPLINTING
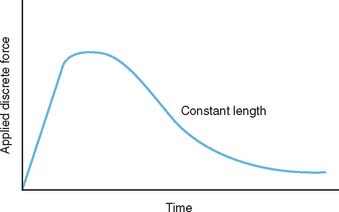
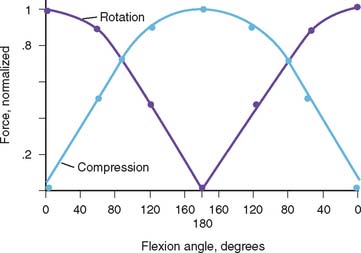
Restorative splinting can be used to assist in attaining elbow motion. Splints are designed according to two diverse philosophies: dynamic or static-adjustable. To comprehend the rationale of dynamic or static adjustable splinting, some understanding of the soft tissue about the elbow as viscoelastic tissue is necessary. If thesoft tissue at the elbow can be considered viscoelastic tissue, its response to a constant versus a variable force is different.12 The theoretical response to a constant force is shown in Figure 11-5. This load results in soft tissue deformation, which is called creep.8 However, what is not demonstrated in this illustration is the development of inflammation as a biologic response to this constant load. Inflammation can alter this idealized curve, and in the author’s opinion, inflammation is a common byproduct of dynamic splinting. Nonetheless, this remains an attractive option for many11 (Fig. 11-6). The alternate approach to the stiff elbow is the use of static adjustable splints. In this modality, a constant force is applied to the elbow that results in strain being imparted to the tissue. However, the force is not continuously applied, allowing stress relaxation to occur within the soft tissue sleeve over a period of time. This type of treatment has been employed extensively at the knee by serial casting and has also been effectively used at the elbow.14 It is believed that the stress-free relaxation lessens the likelihood of inflammation, and thus, the elbow in our practice and opinion is more amenable to this type of load application (Fig. 11-7). The constant force is applied so as to exceed the elastic limits of the tissue or result in a stretch. But if this load is maintained at a constant and is not further increased, tissue relaxation should occur over time. Finally, to further avoid the likelihood of inflammation, the patient controls the amount and duration of tension being applied. This is done within a very discrete set of recommendations and a very defined program (see Appendix). However, as with all torque generated across the elbow by whatever means, a compressive force is also applied to the system. This joint force can reach considerable proportions and is a function of the direction of the torque and the ankle of the elbow at the time of application13 (Fig. 11-8). Ideally, the splint hinge mechanism absorbs the majority of the force which is primarily compressive in nature whether the application is in flexion or extension.
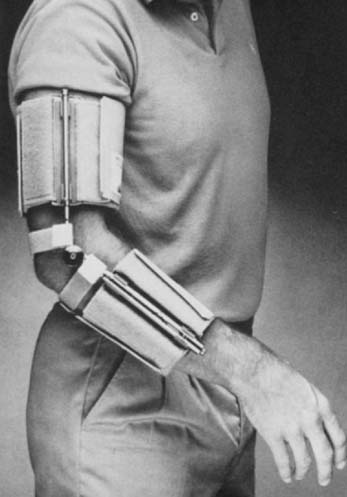
FIGURE 11-6 Commercially available dynamic splint. The tension and excursion may be adjusted by the patient.
DYNAMIC SPLINTING
Dynamic splinting has been a popular means of treating impending or developing stiffness. The concept has been used in hemophiliacs by employing a system of reverse dynamic slings at both the knee and at the elbow.3 The earliest examples of dynamic splinting employed rubber bands to deliver to torque. At the elbow, this has given way to much more sophisticated mechanics and devices. Data has been published to suggest the value of dynamic splinting to assist extension after triceps injury.7 Today, there are several readily available commercial devices that employ this concept (see Fig. 11-6). The splint is well tolerated at least initially but can cause pain and introduce reactive inflammation if used too aggressively.
STATIC ADJUSTABLE SPLINTS
The classic static adjustable splint is a turnbuckle type and use was reintroduced several years ago by Green and associates.6 He reported an 80% success rate in treating elbow contractures from various etiologies, especially those with a major flexion contracture. Two problems were identified with the use of these splints.
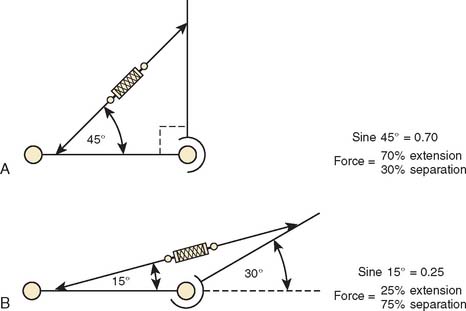
As the contracture decreases to less than 30 degrees, the effectiveness of a turnbuckle to develop an extension torque decreases. Applying an extension load at this angle results in the majority of the force distributed so as to separate the hinge, and less than 25% of the force actually exerts an extension torque on the elbow (Fig. 11-9). The ability of this concept to enhance post-traumatic elbow motion has been recently demonstrated in a clinical trial.4 In another study, 11 of 22 patients gained satisfactory motion after initiating turnbuckle type bracing in a sample of those who no longer were benefiting from physical therapy.5
Hence, to develop a more effective device, a means was developed to apply the force through a gear mechanism at the axis of flexion; by so doing the entire force is then applied as intended: either to extend or to flex. (Fig. 11-10). The brace was designed at our institution and is termed the “Mayo Elbow Brace (Don Joy, Orthopedics) and is able to hyperextend to enhance the ability to completely resolve the contracture (Fig. 11-11). However, with flexion to more than 100 or 110 degrees, the anterior soft tissue tends to bunch up, limiting further flexion. For this reason, the straps closest to the joint may be released to allow unencumbered flexion.

FIGURE 11-11 The same splint shown in Figure 11-10, but reversed and being used in the flexion mode; hence, the splint is called the universal splint in our practice. For flexion the straps nearest to the hinge are released to avoid impingement.
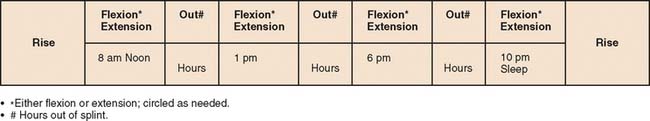
Over the 4-year period from the introduction of this device in 2003 through 2006, we have prescribed approximately 200 braces for patients with various expressions of elbow stiffness. This experience has resulted in the application program shown in Box 11-1 and Figure 11-12. It should be noted that an adequate amount of time should be spent with the patient to explain the rationale of the brace and specific use and goals for the specific device being used.
BOX 11-1 Basic Instructions for the Use of Static Adjustable Splints
After reading these instructions, contact your physician if you have any specific questions.
1 Billingham R.E., Russell P.S. Studies on wound healing, with special reference to the phenomenon of contracture in experimental wounds in rabbits’ skin. Ann. Surg. 1956;144:961.
2 Broberg M.A., Morrey B.F. Results of treatment of fracture dislocations of the elbow. Clin. Orthop. 1987;216:109.
3 Dickson R.A. Reversed dynamic slings: A new concept in the treatment of post-traumatic elbow flexion contractures. Injury. 1976;8:35.
4 Doornberg J.N., Ring D., Jupiter J.B. Static progressive splinting for posttraumatic elbow stiffness. J. Orthop. Trauma. 2006;20:400.
5 Gelinas J.J., Faber K.J., Patterson S.D., King G.J. The effectiveness of turnbuckle splinting for elbow contractures. J. Bone Joint Surg. 2000;82B:74.
6 Green D.P., McCoy H. Turnbuckle orthotic correction of elbow-flexion contractures after acute injuries. J. Bone Joint Surg. 1979;61A:1092.
7 Greer M.A., Miklos-Essenberg M.E. Early mobilization using dynamic splinting with acute triceps tendon avulsion. J. Hand Ther. 2005;18:365. quiz 371
8 Kottke F.J., Pauley D.L., Ptak R.A. The rationale for prolonged stretching for correction of shortening of connective tissue. Arch. Phys. Med. Rehab. 1966;47:345.
9 Lake A.W., Sitler M.R., Stearne D.J., Swanik C.B., Tierney R. Effectiveness of prophylactic hyperextension elbow braces on limiting active and passive elbow extension prephysiological and postphysiological loading. J. Orthop. Sports Phys. Ther. 2005;35:837.
10 Morrey B.F.. The use of splints with the stiff elbow. Heckman M.D., editor. Prospective in Orthopedic Surgery, Vol. I. Quality Medical Publishing, St. Louis, 1990;141. No. 1
11 Richard R., Shanesy C.P., Miller S.F. Dynamic versus static splints: A prospective case for sustained stress. J. Burn Care Rehab. 1995;16:284.
12 Richards R.L., Staley M.J. Biophysical aspects of normal skin and burn scar. In: Richard F.L., Staley M.J., editors. Burn Care and Rehabilitation: Principles and Practice. Philadelphia: F. A. Davis; 1994:65.
13 Szekeres M. A biomechanical analysis of static progressive elbow flexion splinting. J. Hand Ther. 2006;19:34.
14 Zander C.L., Healy N.L. Elbow flexion contractures treated with serial casts and conservative therapy. J. Hand Surg. 1992;17:694.