24.3 Spinal injury
Introduction
Injuries to the spine and spinal cord are less common in children than adults. The injuries have different distributions and frequency in different-aged children, dependent upon the developmental, anatomical and physiological differences with age. Children account for up to 10% of all spinal injuries, but the mortality among spine-injured children is higher than in adults, with estimates ranging from 25–30%, with death most often due to associated injuries to other organs, especially the brain.1
The incidence of spinal cord injury amongst spine-injured children is probably about 1%.1,2 In neurologically impaired survivors the injuries are most commonly at the C1–C2 level, or in the lower cervical or thoracic spine.1 The common causes of spine and spinal cord injuries in children are motor vehicle crashes, falls, diving accidents, sports injuries and, occasionally, non-accidental injury.1,3,4
The majority of injuries in children occur in the cervical spine. In children under 8, most (about 80%) occur in the C1–C3 region, whereas after 8 years of age the incidence is similar to that in adults, with the majority in the lower three cervical vertebrae.2,5,6 The thoracolumbar junction is the most commonly injured area outside the cervical spine, with the thoracic and lumbar spines having roughly equal incidence of about 25%. There is an increased incidence of neurologic injury in fractures of the thoracolumbar junction. The relatively high incidence of injuries in this region is due to the large range of motion and the changing orientation of the facet joints.1,7 Approximately 30% of patients with spinal cord injury have fractures at more than one spinal level. A majority of these are in contiguous vertebral segments, but 5–15% may be in different regions.7
Developmental anatomy and physiology
The atlas ossifies from three ossification centres: two ossification centres of the lateral masses and one ossification centre for the body. The ossification centre for the body does not ossify until about 1 year of age. The posterior arches fuse by 3 or 4 years of age, while the synchondrosis between the lateral masses and the body fuses at approximately 7 years of age.3,5
The axis ossifies from seven ossification centres. The five primary ossification centres are two for the lateral masses, two for the odontoid (which are usually fused at birth but occasionally persist as a dens bicornis), and one for the body. The odontoid is separated from the body by a synchondrosis, which fuses between 3 and 6 years old. The two secondary ossification centres are the tip of the odontoid process (which appears at about 3 years of age and is usually fused by 12 years of age), and the inferior ring apophysis (which, like other ring apophyses, generally ossifies after 8 years of age and fuses in the early 20s).3,5
The remainder of the cervical vertebrae each contain three primary ossification centres, one for the body and one for the two neural arches, and two secondary ossification centres, the ring apophyses. The neural arches fuse posteriorly by the age of 3, and anteriorly the three ossification centres fuse between 3 and 6 years of age. Importantly, the vertebral bodies are wedge-shaped until the age of 7 when they begin to square off.3,4
The thoracic and lumbar spines develop in a similar way, with secondary ossification centres for the spinous process and the transverse processes added. By the time the child is 8–10 years of age the spine has reached near-adult size.3,4
There are a number of other differences of importance for the spine. The fulcrum of movement of the neck is located at C2–C3 in the infant, at C3–C4 by the age of 6, and by the age of 8 the fulcrum is at C5–C6, as it is in the adult. There is a relatively large head and weak neck muscles; laxity of the ligaments and joint capsule; and relatively horizontal positioning of the facet joints with underdevelopment of the uncinate processes.1,3,4 All these features increase the risk of injury to the child’s spine.
Spinal immobilisation
Spinal immobilisation is currently a controversial issue, especially in young children. A balance must be found that will diminish the risk of further injury to the child’s spine, but not interfere with the assessment, or the normal physiological functions, of the child. Traditionally the spine has been immobilised in a rigid cervical collar, on a spine board with a head immobiliser and straps, or with sandbags and tapes, thus providing adequate control of the entire spine (Table 24.3.1).3,8,9
There are a number of potential problems with this immobilisation (Table 24.3.2). Cervical collars are not made to fit infants and alternative immobilisation is needed. An ill-fitting collar may cause the chin to become trapped under the chin support and may cause airway obstruction. The young child may become distressed from being rigidly immobilised, making further assessment difficult, and potentially raising intracranial pressure. Rigid immobilisation in a collar and head immobiliser on a spinal board has also been shown to decrease tidal volume and respiratory excursion.10 In addition, because the young child’s head is disproportionately large, the neck is flexed when immobilised on a standard spinal board. This causes flexion of the cervical spine, which may cause movement at the site of injury. To prevent this, a spinal board with a recess for the head or padding that elevates the torso is needed for children less than 8 years old (Fig. 24.3.1).11–13
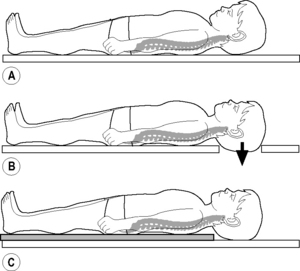
Fig. 24.3.1 Effects of spine-board on cervical spine position in children.
Modified from Herzenberg et al 1989 Emergency transport and positioning of young children who may have an injury of the cervical spine: The standard backboard may be hazardous. Journal of Bone & Joint Surgery 71(1): 15–22.
For children who have less major trauma but are at risk of spinal injury, a degree of judgement is needed by the clinician as to the level of immobilisation that is appropriate. However, in all patients with multiple or significant other injuries immobilisation is still recommended. If the child is not on a spine board, immobilisation solely in a cervical collar, maintaining alignment of the neck and the entire spine, is appropriate. Using sandbags and tape or other means to immobilise the head by fixing it to the bed risks further complications, including airway compromise, and the risks are likely to outweigh the benefits.14,15
To limit discomfort and the likelihood of pressure sores a child should be kept on the spinal board for the shortest possible time. Once resuscitation and urgent procedures and investigations are completed the board should be removed. This is especially important in patients with suspected spinal cord injury.16
Cervical spine injuries
As the cervical spine is the most common region injured and accounts for the majority of spinal cord injuries, a thorough knowledge of injuries in this region and the appropriate assessment of the spine both clinically and radiographically is mandatory. In children younger than 8 years of age the majority (but not all) injuries occur above the fourth cervical vertebra. After 8, the pattern of injury is similar to that seen in adults (the majority of injuries below C4).2,17
Mechanisms of injury
The mechanism of injury is an important historical factor, as it will determine the type and possible instability of the underlying injury (Table 24.3.3).15
Source: Modified from Rosen P et al 1997. Emergency Medicine, 4th edn. Mosby, St. Louis, MO, USA.
Clinical assessment
After immobilisation and resuscitation of the injured child and as part of the secondary survey the neck should be examined. This is done to look for neck abrasions and signs of injury to other structures in the neck as well as to examine the cervical spine. The decision to evaluate the cervical spine for injury should only be made in children who are conscious and alert, who are not drug or alcohol affected, and who do not have other injuries that are painful or distracting enough to make assessment of neck pain difficult.2,17–19
The cervical collar should be removed while another person holds the head inline. No traction should be applied to the neck. The cervical spine is palpated for tenderness over the spinous processes. If there is tenderness over a specific region the collar should be reapplied and the spine evaluated with X-ray. If there is no tenderness (or only soft tissue tenderness) the child should be allowed to gently move the head from side to side. If this produces pain posteriorly in the neck the collar should be reapplied and the spine X-rayed. If there is no pain on movement the collar and cervical spine protection can be removed.2,17–19
Radiographic images
Radiological evaluation is required for all children who do not meet all the criteria for clinical clearance of the cervical spine. As part of the secondary survey in major trauma patients the cross-table lateral cervical spine X-ray would have been performed. This is a guide to the presence of serious cervical spine trauma only and cannot be used to exclude cervical spine injury.2,17 All patients who require radiological evaluation require a full cervical spine series.
The cervical spine series consists of a lateral film, an anterior-posterior film and an odontoid view. Using these three views all abnormal cervical spines will be detected, allowing further investigation to fully delineate the individual injuries.2,5 All seven vertebrae must be included in the lateral view, along with the cervicothoracic junction. If this is not visible gentle traction should be applied to the arms and the film repeated, or a swimmer’s view (transaxillary) should be obtained. Oblique views of the cervical spine may also be of assistance, especially if the cervicothoracic junction is difficult to visualise. Oblique views, however, do not provide any more information regarding the likelihood of injury than the standard three views.2,5,17
In young children, getting co-operation for the odontoid (open mouth) view is difficult. It has been shown that this view can be excluded in children under 5 years of age with little likelihood of missing a fracture.20,21
Other specialised radiological investigations have been used to evaluate cervical spine injuries:
Flexion and extension
Lateral cervical spine radiographs have been used to assess the spine for ligamentous injury. The suggested indications have been symptomatic patients with normal plain X-rays, or the unconscious patient with normal X-rays and/or CT scans. These images have become popular in assessing adult patients but investigations to date have consistently failed to show a benefit over other imaging, with a significant number of studies limited by inadequate motion in the acute setting.22 Most paediatric cervical-spine guidelines do not call for the routine use of these views.23
Computerised tomography (CT)
CT of the cervical spine is common. There have been a number of indications for routine CT suggested, with the most widely accepted being for further evaluation and elucidation of fractures identified, or to view areas not seen adequately on the initial cervical spine series.17 Other suggested indications are for the assessment of the unconscious patient with normal initial radiographs, and for patients having a CT of the brain. Proponents of CT suggest scanning the entire spine in both of these instances and clearing the spine if scans are normal19 (or progressing to flexion-extension views).17,24 Another group suggests just scanning the upper cervical vertebrae in children under 8 as most injuries occur in this region.25,26 There are no studies that have systematically evaluated the role of CT in the evaluation of paediatric cervical spine injuries. CT appears to be as good as any other modality in identifying injuries but the radiation exposure of young children needs to be considered.23
Magnetic resonance imaging (MRI)
MRI is the imaging method of choice for assessing ligamentous injuries and for spinal cord injuries. MRI will visualise most ligamentous injuries and all spinal cord injuries. In many instances MRI will alter the specifics of surgical management in those who require surgical stabilisation. MRI provides prognostic information in children with spinal cord injury.17,27
Radiographic evaluation
Once the X-rays have been obtained, care needs to be taken to interpret the images accurately and correlate the findings with the history and physical examination. Due to the physiological differences described above, a number of normal radiological findings in children are significantly different from those in adults. The common findings that cause concern are: pseudosubluxation of C2 on C3 (seen in up to 25% of children); exaggerated atlantodens distance (seen in 20% of children under 8 years of age); and radiolucent synchondrosis between the odontoid and C2 (seen in all children under 4 and in 50% of those under 10 years of age). Other normal findings that can be misinterpreted include a variable anterior soft tissue width – altering with head positioning and crying – the anterior ring apophyses of the vertebral bodies, and the anterior wedging of the vertebral bodies (especially C3).17,28,29 All of these normal findings can be mistaken for acute traumatic injuries in children following trauma.
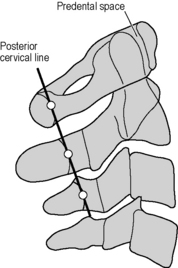
Evaluation of the lateral cervical spine radiograph begins with assessment of the four lines, corresponding to the anterior vertebral bodies, the posterior vertebral bodies, the spinolaminar line, and the tips of the spinous processes. All four of these lines should follow a smooth, even contour (Fig. 24.3.2). The articular facets should be parallel, the intervertebral disc spaces, at the posterior margin of the vertebral bodies, should be similar, and the distances between spinous processes should show no significant widening (fanning). Review of the soft tissue shadow should show a retropharyngeal space of not more than one half the AP diameter of the vertebral body at C2 and no wider than the full width of the vertebral body at C6. As mentioned, this may be difficult to interpret in the crying child.1,3,17
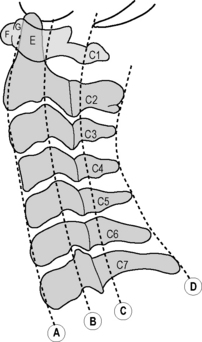
Fig. 24.3.2 Cervical spine lines.
Modified from Barkin et al 1994 Emergency Pediatrics, 4th edn. Mosby, St. Louis, MO, USA.
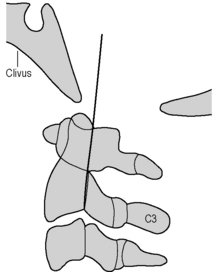
Assessment of these areas of possible abnormality has been made easier by the formulation of a series of normal measurements. For the atlantoaxial relationship (C1–C2), a measurement of the distance (on the lateral film) from the posterior border of the anterior arch of C1 to the anterior margin of the odontoid should be less than 5 mm in children under 8 years of age, and ≤3 mm in older children and adults. To assess the relationship of the basion of the skull to the atlas, the most reliable measurement in children is Harris’s posterior axial line (Fig. 24.3.3), which should lie within 12 mm of the basion of the skull.
The subluxation of C2 on C3 and C3 on C4 consistently causes difficulty in interpretation of paediatric cervical spine films. Swischuk’s line (posterior cervical line), which joins the spinolaminar line of C1 to that of C3, allows assessment of the likelihood of the subluxation being physiological (Fig. 24.3.4). The spinolaminar junction of C2 should lie within 2 mm of this line. If the distance is greater than 2 mm a fracture or pathological subluxation is likely.
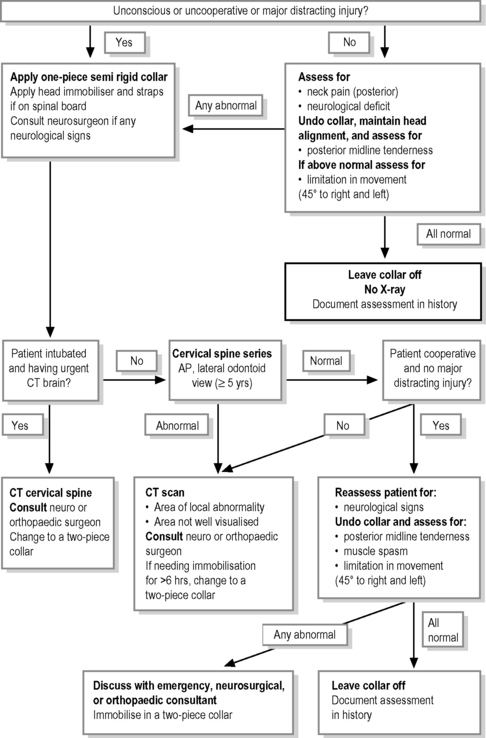
Cervical spine clearance guidelines
With the knowledge of mechanism of injury, immobilisation needed, clinical examination, and radiographic interpretation, it is possible to devise guidelines (Fig. 24.3.5) that allow safe and effective management of the potentially injured cervical spine while minimising the investigations needed. There is as yet no guideline that is well established for young children.30,31 The guideline should include the following points:
Atlantoaxial rotary subluxation
Fixed rotary subluxation at the atlantoaxial joint is more common during childhood than adulthood. It can present after minor trauma, in conjunction with an upper respiratory tract infection, and often no inciting cause is found. The clinical picture is that of the head turned to one side and held in the ‘cock-robin’ position. The child is unable to turn its head past the midline, and attempts to move the head often cause pain. The spasm of the sternocleidomastoid (SCM) muscle is on the side to which the head is turned (ipsilateral side), as the muscle is trying to right the head. In contrast, in a wry neck the SCM spasm is on the side opposite to which the head is turned (contralateral side), with the spasm causing the head turning.1,15,17
Plain radiographs may be diagnostic, revealing the lateral mass of C1 rotated anterior to the odontoid on the lateral view, or rotation of the spinous processes to the ipsilateral side on the AP view. If clinical examination and plain radiographs cannot confirm the diagnosis, CT imaging should be considered.17
Rotary subluxation of short duration will often spontaneously reduce; those that do not or that have been present for a longer duration (days) may need traction or manipulation to reduce. Post-reduction immobilisation is needed to maintain reduction and the duration of immobilisation should vary according to the duration of subluxation.1,17,32
Thoracic and lumbar spine injuries
Fractures of the thoracic spine account for 25–30% of spine injury in children, while lumbar fractures account for 20–25%. Injuries to the thoracic spine and the thoracolumbar junction have a higher incidence of spinal cord injury, with neurological deficit seen in up to 40% of cases.1,7 The high incidence of cord injury is related to the relatively large size of the spinal cord in the thoracic region, the inherent stability of the thoracic spine requiring larger forces to cause bony injury. Multiple level injuries are seen in 30–40% of children with thoracic or lumbar spine fractures.7 Fractures of the lower thoracic and upper lumbar spine have associated small bowel and visceral injury in up to 50% of cases.1 Road traffic accidents and falls account for most of the injuries, but non-accidental injuries in these regions do occur.
Mechanism of injury
A number of bony injuries are caused by these mechanisms. Compression of the vertebral body with anterior wedging is the most common. However, a degree of anterior wedging is normal in children. Burst fractures occur where there is disruption of the endplates and herniation of the disc into the vertebral body. Retropulsed fragments can cause spinal cord injury. The ‘seat-belt’ fracture, associated with the lap-only seat belt, is a hyperflexion and distraction injury most commonly seen at the thoracolumbar junction, and is frequently associated with visceral or mesenteric injury. The posterior bony or ligamentous elements are disrupted and the fracture line extends horizontally into the vertebral body or through the intervertebral disc.1,4,7,33
Clinical assessment
Any patient who has pain or tenderness over the spine should have the spine evaluated by radiography. Patients without pain or tenderness who have altered conscious state or other significant injuries are at risk of having thoracic or lumbar spine injuries missed (as they are for cervical spine injuries).34 As multi-level injuries are common, any child with a proven cervical spine fracture or spinal cord injury should have the entire spine imaged with plain radiographs (see Fig. 24.3.5).
Radiographic evaluation
After clinical evaluation, radiographs should be taken on any child who is at risk of having a thoracic or lumbar spine injury (Table 24.3.4). The standard views for both areas are the anterior-posterior radiograph and the lateral film. In the thoracic region the radiographs need to be overexposed compared to a normal chest X-ray to allow adequate views of the spine. The shoulders often obscure the upper thoracic spine and a swimmer’s view may be needed to visualise the first two thoracic vertebrae.
The films should be evaluated by following the anterior and posterior vertebral body lines and the spinolaminar line on the lateral view. These three lines should have a parallel course. The height of each vertebral body should be assessed anteriorly and posteriorly, and a difference of more than about 3 mm treated as pathological. On the AP view the paraspinal lines should be closely inspected to detect evidence of paraspinal haematoma. The posterior elements should be visible through the vertebral body and should be in alignment. Each vertebra should be inspected; an apparently empty or invisible vertebral body indicates a fracture dislocation with distraction.1,33
There are a number of features on the radiographs that indicate an unstable fracture: vertebral body collapse with widening of the pedicles; greater than 33% compromise of the spinal canal by retropulsed fragments of the lamina, pedicles or body; translocation of more than 2.5 mm between vertebral bodies in any direction; bilateral facet joint dislocation; or greater than 50% anterior compression of the vertebral body associated with widening of the interspinous space.33
Some fractures in the thoracic region can be difficult to see on plain films, especially if there were technical difficulties in obtaining the films in multiply-injured patients. A number of secondary signs of thoracic spine injury exist and can help make the diagnosis. A paravertebral haematoma can usually be seen at the site of injury, blood in the pleural space may be seen as a pleural cap, and widening of the mediastinum may be present. Unfortunately these signs cannot differentiate a thoracic spine injury from an aortic arch injury.7
Management
Management must start with care of the airway, breathing and circulation. Only once these areas have been stabilised should management of the spine proceed. However, while the patient is being stabilised the spine should be maintained in alignment and the patient moved by log rolling. A thorough assessment and investigation of the abdomen and chest is mandatory for all patients with significant thoracic and upper lumbar spine injuries, and injuries to the pelvis must not be forgotten with lumbar spine injuries. As many of these injuries are associated with intra-abdominal injuries an ileus is common and nasogastric or orogastric tube should be inserted. Consultation with a paediatric orthopaedic surgeon or neurosurgeon should be sought for the definitive care of the injury. Surgical stabilisation is usually required for unstable fractures and those fractures associated with neurological injury.4,7,33
Spinal cord injury
The goal of management of injury to the spinal cord or cauda equina is to minimise the resulting neurological deficit. This commences with adequate immobilisation of the spine and complete and thorough investigation to detail the anatomy of the injury.35
Spinal cord injury should be suspected in any child who has multisystem trauma, minor trauma associated with spinal pain, sensory or motor symptoms, and any patient with altered consciousness. The patient must be adequately immobilised, such as on a spinal board with a cervical collar and head immobiliser (see section on spinal immobilization, p. 545), and any assessment of the back or patient movement accomplished by log rolling. Up to 50% of patients with spinal cord injury will have at least moderate head injury.35
Spinal cord injury syndromes
A number of patterns of neurological deficit are seen in patients with spinal cord injury, with the deficit dependant on the portion of the spinal cord damaged. Neurogenic shock – the manifestations of loss of sympathetic output to the cardiovascular system – is seen immediately after complete cord injury at the level of T6 or above. This should not be confused with spinal shock, which is the reversible dysfunction of the spinal cord associated with injury. It is likened to a concussion of the cord without permanent damage. It may exist alone or in combination with permanent cord injury. Its resolution is responsible for the improvement in neurological function seen in the first few days post-injury.15,35
Complete cord injury is usually seen in injuries of the thoracic spine and thoracolumbar junction. The spinal cord is large in relation to the size of the spinal canal at this level. Complete cord injuries that remain at 24 hours rarely regain any significant function. Cauda equina lesions – injuries at or below L2 – involve the peripheral nerves rather than the spinal cord and can show significant recovery of lower limb and sphincter function even weeks after the injury.15,35
Central cord syndrome is usually seen in hyperextension injury resulting in herniation of the intervertebral disc into the spinal cord. The resulting injury causes a motor deficit that is greater in the arms than legs and most extensive in the small muscles of the hand. The sensory deficit is variable. Brown–Sequard syndrome – hemisection of the cord – causes a contralateral loss of pain and temperature sensation and an ipsilateral motor paralysis and loss of proprioception below the level of injury. Approximately two-thirds of those with central cord syndrome and one-third with Brown–Sequard syndrome will recover.15,35
Clinical assessment
Initial steps in the management of a patient with a suspected spinal cord lesion are the assessment and resuscitation of the airway, breathing and circulation. The most immediate threats to life and spinal cord function of patients with spinal cord injury remain hypoxia and hypotension. Spinal cord lesions in the upper cervical spine may impair respiratory function and require early intubation and mechanical ventilation. The unstable cervical spine must be maintained in alignment without traction during treatment of the airway. The loss of sympathetic vasomotor tone after cervical spinal cord injury will result in vasodilatation, venodilatation, and reduced venous return to the heart causing hypotension. There should be an associated relative bradycardia for age and existing blood pressure, which will help distinguish this response from haemorrhagic shock.35
Radiographic evaluation
In all patients with suspected spinal cord injury the spine should be X-rayed. The radiographs should include the entire spine, as multiple levels of injury are common. Once the patient is stabilised, further investigation of the lesion should follow. The bony injuries should be investigated as discussed above. Investigation of the cord itself will require MRI. MRI should be performed as soon as possible after identification of a spinal cord injury, as it will allow identification of remedial intraspinal problems in patients with a partial neurological deficit. The appearance of the spinal cord on MRI also allows prediction of neurological outcome. Cord transection and major haemorrhage have a poor outcome, minor haemorrhage and oedema have a moderate to good outcome, and a normal MRI is associated with complete recovery.1
Treatment
Most of the treatment available for spinal cord injuries is supportive. The breathing and circulation must be supported as needed. As there will be a neurogenic bladder, catheterisation is necessary, and a nasogastric tube is needed to treat the gastric and bowel stasis that ensues. For transport, antiemetic is useful to prevent vomiting and spine movement or airway compromise. Subcutaneous low-molecular-weight heparin should be instigated once the patient is stable to prevent deep venous thrombosis.36
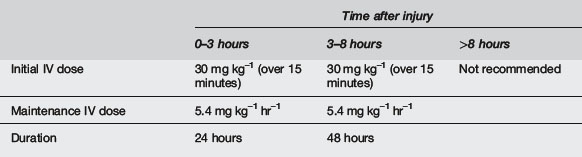
Specific treatment of the spinal cord lesion is controversial. Four substances have been studied in prospective, randomised trials – methylprednisolone, tirilazad, naloxone and GM-1 ganglioside. All studies to date have excluded children under 13 years of age. Tirilazad and naloxone have failed to show any benefit in trials to date. There is conflicting evidence regarding the benefits of methylprednisolone and documented evidence that its use increases the risk of bacterial infection. It is recommended that it be used with knowledge of the risks and possible benefits.15,36 The current regimens for use are seen in Table 24.3.5. GM-1 ganglioside has yet to be shown to offer significant benefit in spinal cord injury, and is not recommended for routine use.
SCIWORA
Spinal cord injury without radiographic abnormality (SCIWORA) is defined as objective signs of myelopathy as a result of trauma with no evidence of fracture or ligamentous instability on plain X-rays or tomography.37 SCIWORA is most frequently seen in younger children (especially <8 years of age), and in injuries of the cervical spine. Postulated causes include ligamentous laxity and bony immaturity allowing excessive, transient movement during trauma, causing distraction or compression of the spinal cord, or cord ischaemia due to vascular injury or hypoperfusion. The incidence reported in children is 1–10% of all spinal cord injuries.1,15,38,39
Younger children tend to have more profound neurological injury, and hence less long-term improvement.38,39 A number of children will present with minor neurological injury and progress to complete or partial spinal cord injury. The incidence of this delayed presentation of the serious symptoms is 5–50%. The delay to presentation of full symptoms has been as long as 4 days.1,3 Because of these presentations, all children with history of neurological symptoms or any neurological deficit should be treated as patients with potential spinal cord injuries.
After the primary survey, resuscitation and secondary survey and radiographic evaluation, any patient with any neurological deficit should remain immobilised until all bony, ligamentous and spinal cord injury is excluded or treated. Further investigation with a CT scan focused at the level of symptoms and MRI to view the cord should be performed. MRI provides the same prognostic information in SCIWORA injuries as in other spinal cord injuries.15
1 Roche C., Carty H. Spinal trauma in children. Pediatr Radiol. 2001;31(10):677-700.
2 Viccellio P., Simon H., Pressman B.D., et al. A prospective multicentre study of cervical spine injury in children. Paediatrics. 2001;108(2):e20.
3 Dormans J.P. Evaluation of children with suspected cervical spine injury. Instr Course Lect. 2002;51:401-410.
4 Reynolds R. Pediatric spinal injury. Curr Opin Pediatr. 2000;12(1):67-71.
5 Jaffe D.M., Binns H., Radkowski M.A., et al. Developing a clinical algorithm for early management of cervical spine injury in child trauma victims. Ann Emerg Med. 1987;16(3):270-276.
6 Platzer P., Jaindl M., Thalhammer G., et al. Cervical spine injuries in pediatric patients. J Trauma-Injury Infect Crit Care. 2007;62(2):389-396. discussion 94–6
7 Brandser E.A., el-Khoury G.Y. Thoracic and lumbar spine trauma. Radiol Clin North Am. 1997;35(3):533-557.
8 Jaffe D.M. Evaluation of children for cervical spine injuries. In Strange G.R., editor: Paediatric emergency medicine: a comprehensive study guide, 2nd ed, New York: McGraw-Hill, 2002.
9 Woodward G. Neck trauma. In Fleisher G., Ludwig S., editors: Textbook of Paediatric Emergency Medicine, 4th ed, Philadelphia: Lippincott Williams & Wilkins, 2000.
10 Schafermeyer R.W., Ribbeck B.M., Gaskins J., et al. Respiratory effects of spinal immobilisation in children. Ann Emerg Med. 1991;20:1017-1019.
11 Herzenberg J.E., Hensinger R.N., Dedrick D.K., Phillips W.A. Emergency transport and positioning of young children who have an injury of the cervical spine. The standard backboard may be hazardous. J Bone Joint Surg Am. 1989;71(1):15-22.
12 Treloar D.J., Nypaver M. Angulation of the pediatric cervical spine with and without cervical collar. Pediatr Emerg Care. 1997;13(1):5-8.
13 Curran C., Dietrich A.M., Bowman M.J., et al. Pediatric cervical-spine immobilization: achieving neutral position? J Trauma. 1995;39(4):729-732.
14 Anonymous. Cervical spine immobilization before admission to the hospital. Neurosurgery. 2002;50(Suppl. 5):S7-17.
15 Mathison D.J., Kadom N., Krug S.E. Spinal cord injury in the pediatric patient. Clin Ped Emerg Med. 2008;9:106-123.
16 Quigley S., Curley M. Skin integrity in the pediatric population: preventing and managing pressure ulcers. JSPN. 1996;1(1):7-18.
17 Anonymous. Management of pediatric cervical spine and spinal cord injuries. Neurosurgery. 2002;50(Suppl. 3):S85-S99.
18 Hoffman J.R., Mower J.R., Wolfson A.B., et al. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. N Engl J Med. 2000;343:94-99.
19 Hutchings L., Willett K. Cervical spine clearance in pediatric trauma: a review of current literature. J Trauma-Injury Infect Crit Care. 2009;67(4):687-691.
20 Buhs C., Cullen M., Klein M., Farmer D. The pediatric trauma C-spine: is the ‘odontoid’ view necessary? J Pediatr Surg. 2000;35(6):994-997.
21 Swischuk L.E., John S.D., Hendrick E.P. Is the open-mouth odontoid view necesary in children under 5 years? Pediatr Radiol. 2000;30:186-189.
22 Insko E., Gracias V., Gupta R., et al. Utility of flexion and extension radiographs of the cervical spine in the acute evaluation of blunt trauma. J Trauma. 2002;53:426-429.
23 Rana A.R., Drongowski R., Breckner G., Ehrlich P.F. Traumatic cervical spine injuries: characteristics of missed injuries. J Pediatr Surg. 2009;44(1):151-155. discussion 55
24 Berne J.D., Velmahos G.C., El-Tawil Q., et al. Value of complete cervical helical computed tomographic scanning in identifying cervical spine injury in the unevaluable blunt trauma patient with multiple injuries: a prospective study. J Trauma-Injury Infect Crit Care. 1999;47(5):896-902. discussion 02-3
25 Browne G.J., Cocks A.J., McCaskill M.E. Current trends in the management of major paediatric trauma. Emerg Med (Fremantle). 2001;13(4):418-425.
26 Hutchings L., Atijosan O., Burgess C., Willett K. Developing a spinal clearance protocol for unconscious pediatric trauma patients. J Trauma-Injury Infect Crit Care. 2009;67(4):681-686.
27 Holmes J., Mirvis S., Panacek E., et al. Variability in computed tomography and magnetic resonance imaging in patients with cervical spine injuries. J Trauma. 2002;53:524-530.
28 Swischuk L. The cervical spine in childhood. Curr Probl Diagn Radiol. 1984;13:1-26.
29 Kriss V.M., Kriss T.C. imaging of the cervical spine in infants. Pediatr Emerg Care. 1996;13(1):44-49.
30 Ehrlich P.F., Wee C., Drongowski R., Rana A.R. Canadian C-spine Rule and the National Emergency X-Radiography Utilization Low-Risk Criteria for C-spine radiography in young trauma patients. J Pediatr Surg. 2009;44(5):987-991.
31 Garton H.J., Hammer M.R. Detection of pediatric cervical spine injury. Neurosurgery. 2008;62(3):700-708. discussion 00-8
32 Subach B.R., McLaughlin M.R., Albright A.L., Pollack I.F. Current management of pediatric atlantoaxial rotatory subluxation. Spine. 1998;23(20):2174-2179.
33 Clark P., Letts M. Trauma to the thoracic and lumbar spine in the adolescent. Can J Surg. 2001;44(5):337-345.
34 Meek S. Lesson of the week: fractures of the thoracolumbar spine in major trauma patients.[comment]. Br Med J. 1998;317(7170):1442-1443.
35 Chiles B.W., Cooper P.R. Acute spinal injury. N Engl J Med. 1996;334(8):514-520.
36 Anonymous. Pharmacological therapy after acute cervical spinal cord injury. Neurosurgery. 2002;50(Suppl. 3):S63-S72.
37 Pang D., Pollack I. Spinal cord injury without radiographic abnormality in children – The SCIWORA syndrome. J Trauma. 1989;29(5):654-664.
38 Pang D., Wilberger J. Spinal cord injury without radiographic abnormalities in children. J. Neurosurg.. 1982;57:114-129.
39 Anonymous. Spinal cord injury without radiographic abnormality. Neurosurgery. 2002;50(Suppl. 3):S100-S104.