Chapter 91 Spinal Deformity and Correction
The Fundamentals
Spinal deformity is a three-dimensional alteration of spinal alignment in both the coronal and sagittal planes. Scoliosis, strictly speaking, is a curvature greater than 10 degrees in the coronal (frontal) plane, as determined by measuring the Cobb angle (Fig. 91-1). There are many causes, and the condition may occur throughout life from infancy through adulthood. The type of deformity and patient age at presentation have a significant impact on the ultimate treatment of the condition. These topics will be discussed separately throughout this book and are beyond the scope of this chapter. Surgical treatment of these conditions varies depending on the age of the patient and the degree of the deformity. Adults with spinal deformity often seek surgical consultation for pain associated with the deformity, spinal imbalance, or neurologic signs/symptoms. Children and adolescents are most often sent for surgical evaluation for cosmetic concerns and risk of curve progression. Pain and/or neurologic compromise are rare in this patient cohort. For the purposes of this chapter, the authors will focus on the principles of spinal deformity and not the causes or specific treatments. These principles may be applied to most conditions affecting spinal alignment.
The treatment of spinal deformity is not new. Hippocrates attempted traction scoliosis, and Pare used an iron corset in the 16th century in an attempt to correct a similar deformity.1 Not until the development of Paul Harrington’s rod system in the 1960s did the surgical correction of spinal deformity take off.2 For the first time, Harrington’s distraction rod systems, then compression rod systems, permitted correction and improved arthrodesis of the deformed spine. This development truly revolutionized treatment of these dynamic and complex conditions. Early strategies for fixation focused largely on coronal plane correction. Often excellent results were obtained, but these resulted in flattening of the sagittal plane. Unfortunately, this often led to the development of decompensation in the sagittal plane and subsequent pain. This has been referred to as flatback deformity.3 The next phase in development was the application of hooks, then screws, in the thoracolumbar spine. The use of hooks and screw fixation of the spine permitted a greater control over the spine and corrective maneuvers. Greater degrees of correction could be obtained, fixation was improved, and shorter constructs could be used. Powerful control of individual segments of the spine with three-dimensional correction that was not limited by postoperative bracing became the basis for present-day deformity correction systems.4
Treatment Goals
Although the indications and strategies vary, depending on the age of the patient and the deformity encountered, the goals of surgical treatment are essentially the same. The primary goals are to halt curve progression, relieve pain, and improve cosmesis and function. The surgical goals are to obtain a solid arthrodesis with a well-balanced three-dimensional spine.5 In adolescents, the focus should be on curve correction, improving cosmesis, and halting curve progression. As mentioned earlier, treatment of axial and/or radicular pain is much less of a concern.6 In adults, the focus is much less on curve correction but rather on balancing the spine and attaining solid arthrodesis and neurologic decompression if required.
General Terms
A unique set of terms may be applied to spinal deformity and should be reviewed briefly. Spinal deformity involves a curvature and obligatory rotation (coronal plane) in either the coronal and/or sagittal planes. Curves in either plane are measured end vertebra to end vertebra. The end vertebra is the most cephalad and most caudal vertebra of a curve (Fig. 91-2). Lines extended along the end plates of the vertebral bodies that are part of the curve in question all converge toward a central point within the concavity of a curve. Lines extended along the end plates of vertebral bodies not involved become divergent. The most rostral or caudal vertebral body visualized is the end vertebra. The neutral vertebra is that vertebra between curves that demonstrates the least rotation. Both pedicles should be relatively symmetrical. The stable vertebra is the vertebra that is bisected by the center sacral vertical line. This line is determined by first drawing a line connecting the most rostral point on each of the iliac crests. A perpendicular drawn from the midpoint of the S1 vertebra superiorly defines this line. Surgeons often use the stable or neutral vertebra when deciding where to end a construct/fusion.
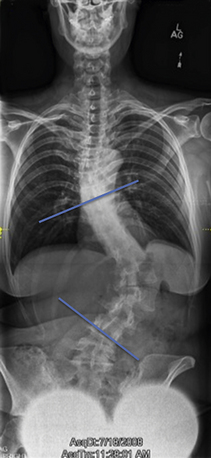
FIGURE 91-2 The end vertebrae are defined (blue lines) as the most rostral and caudal vertebrae in the curve.
Spinal balance is critical for optimal biomechanics. This is determined using a plumb line. In the coronal plane, the line is drawn from the center of the C7 vertebral body to the sacrum. This line should fall within 2.5 cm of the center of the sacrum.7 Deviation greater than this provides evidence of coronal decompensation. This may be determined using 36-inch scoliosis radiographs or directly on the patient, estimating the location of C7 and using the gluteal cleft as the midsacrum. In the sagittal plane, the line should extend from the center of the C7 vertebra and the dorsal aspect of the L5-S1 disc space.8 On the patient, a plumb line may be drawn from the external meatus of the ear, and the line should fall along the greater trochanter when the spine is balanced.
Causes of Spinal Deformity
Idiopathic Scoliosis
By far the most common type of spinal deformity is idiopathic scoliosis. As the name implies, the cause for the condition is unknown; however, significant evidence suggests genetic influences.3,9–11 These curves present in adolescence and have a risk of progression during growth of the spine. Surgery is not always required. A discussion of surgical indications is beyond the scope of this chapter and is related to curve magnitude, location, and maturity status of the patient’s spine.
Degenerative Deformities
As the spine progresses down the degenerative cascade as defined by Kirkaldy-Willis12 and does so asymmetrically, deformity may, and often does, occur. Classically, this involves the lumbar spine. Curvature, lateral listhesis, and rotation are usually seen. Patients may present with lumbar axial pain, radiculopathy, and/or neurogenic claudication. Treatment is dependent on the presenting symptomatology. Radicular pain may only require foraminotomy, whereas decompensation and axial mechanical pain may require deformity correction and stabilization.
Scheuermann Kyphosis
This type of kyphosis, which may occur solely in the thoracic or thoracolumbar spine, may present at any time between adolescence and adulthood. The cause is thought to involve asymmetrically higher ventral intradiscal pressures, which may lead to focal disc herniation of the end plates, generating Schmorl nodes. There may be injury to the growth plate, disproportional loss of ventral vertebral body height, irregularities of the end plates, and narrowing of the disc interspaces.11 Patients may present with pain, progression of kyphosis, or cosmetic concerns.
Principles of Deformity Correction
Cantilever Forces
This is probably the most common technique used for the correction of deformity. In general, a rod is bent to the desired contour for optimal alignment and is then connected sequentially to each pedicle screw or hook previously placed. The correction is greater with multiple points of fixation (i.e., multiple pedicle screws or hooks).13,14 As each screw is sequentially connected to the preformed rod, the spine begins to conform to the rod’s contoured design. The spine may be contoured in this manner in both the coronal and sagittal planes.
With rigid curves, the aforementioned technique may not be possible for significant correction. Ventral discectomies/osteotomies may be helpful for more significant correction. Dorsal osteotomies (complete facetectomies), with or without discectomies, also aid in further correction. Moreover, pedicle screws offer greater correction compared with hook constructs.15 The most difficult task with this correction maneuver is bringing the spine to the rod. Many options exist to aid in reduction and depend on the system used for stabilization. One available option is “reduction screws.” These screws have an extra long tulip, in which part of it may be broken off after the rod is secured to the screw. “Persuaders” may also be used, where the rod is pushed to the screw until a “cap” may be inserted. Surgeons must use extreme care in patients with osteoporosis or very rigid curves or when small-diameter pedicle screws have been used. Screws in these circumstances may easily pull out. Lastly, forces may be less on each individual screw if reduction is applied to multiple screws simultaneously as the spine is brought to the contoured implant.
Derotation
Practically speaking, forces applied to the spine (cantilever, compression, distraction) all result in translation of the vertebral bodies. Classically, derotation credited to Cotrel and Dubousset results in translation but not the desired rotation of the apical vertebrae.16 Newer frame-type constructs are now available in modern deformity instrumentation sets that may actually permit true derotation along with translation.
Typically, the direction of rotation is toward the concavity, or clockwise. This maneuver translates the apex of the curve toward the midline and into kyphosis. It is best to use monoaxial or uniaxial screws for this maneuver.17 Some systems have polyaxial screws that make connecting the rod to the screws much easier, but they may then be “locked” as monaxial screws during derotation.
Significant forces are applied to the spine during this maneuver. Care must be used in rigid curves or in those with osteoporosis. During derotation, the spine should be continuously assessed. Osteotomies may be necessary for optimal translation. With all corrective maneuvers, the sagittal plane must be assessed following coronal correction. Compression/distraction or in situ bending may be necessary to gain more correction.
Ventral Releases
With the wide use of pedicle screws, the need for ventral release procedures has been questioned. The additional release procedures expose the patient to increased morbidity, especially pulmonary. It also appears that dorsal-only surgery results in similar outcomes compared with anterior/posterior procedures. Good et al. recently demonstrated that dorsal-only adult scoliosis surgery achieved similar correction to anterior/posterior surgery while decreasing blood loss, operative time, and length of hospital stay, as well as avoiding additional anesthesia. Complications, radiographic outcomes, and clinical outcomes were similar at follow-up of longer than 2 years.18
Osteotomies
Smith-Petersen Osteotomy
Smith-Petersen osteotomies (SPOs) were originally described for the treatment of ankylosing spondylitis.10 Currently, the osteotomy is more widely applied for the treatment of sagittal plane deformities. SPOs are generally indicated for the treatment of gentle “swooping” as opposed to focal “sharp” curves, especially in the thoracic spine (i.e., Scheuermann kyphosis).19 Approximately 5 degrees of correction may be attained per level. Multiple SPOs may be performed to achieve greater overall correction.
Technically, SPOs involve shortening of the posterior column while lengthening the anterior column. The axis or rotation is based on the middle column. The lower half of the lamina and spinous process of the upper level as well as the upper half of the lamina and spinous process of the lower level are removed. The inferior and superior articulating processes as well as the ligamentum flavum are removed bilaterally. Following placement of screws or hooks, compression may be applied across the osteotomy(ies). As mentioned earlier, this involves shortening the posterior column along the axis of the middle column and lengthens the anterior column. For this to occur and permit correction, the anterior column must not be ankylosed. SPOs are not possible in the face of multiple ventral bridging osteophytes. Careful scrutiny of preoperative imaging is required prior to including SPOs in the plan for deformity correction. Care must be taken to avoid complications during the performance of single or multiple SPOs. Potential major complications directly attributed to the osteotomy include vascular and neurologic complications. Extension or lengthening of the anterior column may include injury to major vascular structures such as the aorta or its vessels. Neurologic complications have been reported in up to 30% of cases.20 Neurologic complications may be minimized with careful wide osteotomies, including the surrounding lamina, so there is no direct compression of neurologic structures when closing or compressing across the osteotomy. Minor complications include extensive blood loss, especially with multiple SPOs, durotomy, and pseudarthrosis.
Pedicle Subtraction Osteotomy
Thomason introduced pedicle subtraction osteotomy (PSO) in 1985.21 Similar to SPOs, PSO is largely indicated for the treatment of sagittal plane deformities. It also may be performed asymmetrically for the correction of both coronal and sagittal plane deformities. This type of osteotomy is powerful and able to correct approximately 30 degrees per PSO. It is technically more demanding compared with the SPO and associated with greater morbidity.19
Various schemes have been developed to not only help determine at which level to perform the osteotomy but also how much of the vertebral body to remove.22 A rule of thumb is that for every 1 cm of osteotomy, there is 10 degrees of correction in the sagittal plane. Therefore, a dorsal osteotomy of approximately 3 cm permits about 30 degrees of correction.
Morbidity may be high with a PSO. Similar to an SPO, major risks include damage to vascular and neurologic structures. Bleeding may be excessive and continues until the osteotomy is closed.23
Vertebral Column Resection
Complete resection of one or multiple vertebral levels and spinal shortening may be required for severe rigid curves, usually more than 80 degrees, fixed trunk translation, or asymmetry between the length of the convex and concave columns to be corrected.19,24 The goal of vertebral column resection (VCR) is to balance the spine in both planes while shortening the length of the spinal column.
VCR may be performed using a combined anterior/posterior approach or by a dorsal-only strategy.25,26 The dorsal-only approach may reduce operative time, complications, and effort associated with the combined procedure.
Similar to other osteotomies, the complication rate of a VCR may be high. Bradford and Tribus reported on 24 patients treated with a VCR.24 They noted 31 complications in 14 of the patients, in which 13% were neurologic but none resulted in paralysis. Significant bleeding may be encountered until final correction is obtained. Recently, Lenke et al.11 published a report on dorsal VCR patients with a minimum 2-year follow-up. They noted spinal deformity correction rates between 51% and 60% for the various categories of deformity, and more importantly, reported no spinal cord–related complications. However, they did note the complexity of the reconstruction: surgeons should be well versed in spinal deformity surgical treatment before embarking on this technically demanding procedure. A similar report evaluating pediatric and adult VCR patients confirmed these findings.25
Bess R.S., Lenke L.G., Bridwell K.H., et al. Comparison of thoracic pedicle screw to hook instrumesntation for the treatment of adult spinal deformity. Spine. 2007;32(5):555-561.
Cotrel Y., Dubousset J., Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop Relat Res. 1988;227:10-23.
Kim Y.J., Bridwell K.H., Lenke L.G., et al. Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a minimum 5-year follow-up study. Spine (Phila Pa 1976). 2007;32(20):2189-2197.
Kim Y.J., Lenke L.G., Cho S.K., et al. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2004;29(18):2040-2048.
Lee S.M., Suk S.I., Chung E.R. Direct vertebral rotation: a new technique of three-dimensional deformity correction with segmental pedicle screw fixation in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2004;29(3):343-349.
Lenke L.G., O’Leary P.T., Bridwell K.H., et al. Posterior vertebral column resection for severe pediatric deformity. Minimum two-year follow-up of thirty-five consecutive patients. Spine (Phila Pa 1976). 2009;34(20):2213-2221.
Takahashi S., Delécrin J., Passuti N. Surgical treatment of idiopathic scoliosis in adults: an age-related analysis of outcome. Spine (Phila Pa 1976). 2002;27(16):1742-1748.
Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop Relat Res. 1985;194:142-152.
Wiggins G.C., Ondra S.L., Shaffrey C.I. Management of iatrogenic flat-back syndrome. Neurosurg Focus. 2003;15(3):E8.
Yang B.P., Chen L.A., Ondra S.L. A novel mathematical model of the sagittal spine: application to pedicle subtraction osteotomy for correction of fixed sagittal deformity. Spine J. 2008;8(2):359-366.
Yong-Hing K., Kirkaldy-Willis W.H. The pathophysiology of degenerative disease of the lumbar spine. Orthop Clin North Am. 1983;14(3):491-504.
1. Heary R.F. Overview of spinal deformity. In: Heary R.F., Albert T.J., editors. Spinal deformities. New York: Thieme; 2007:3-11.
2. Harrington P.R. Treatment of scoliosis. Correction and internal fixation by spine instrumentation. J Bone Joint Surg [Am]. 1962;44:591-610.
3. Kulkarni S., Nagarajan P., Wall J., et al. Disruption of chromodomain helicase DNA binding protein 2 (CHD2) causes scoliosis. Am J Med Genet A. 2008;146A(9):1117-1127.
4. Cotrel Y., Dubousset J., Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop Relat Res. 1988;227:10-23.
5. Buttermann G.R., Glazer P.A., Hu S.S., et al. Anterior and posterior allografts in symptomatic thoracolumbar deformity. J Spinal Disord. 2001;14(1):54-66.
6. Smith J.A. Adult deformity: management of sagittal plane deformity in revision adult spine surgery. Orthopedics. 2001;12(3):206-215.
7. Emami A., Deviren V., Berven S., et al. Outcome and complications of long fusions to the sacrum in adult spine deformity: Luque-Galveston, combined iliac and sacral screws, and sacral fixation. Spine (Phila Pa 1976). 2002;27(7):776-786.
8. Berven S.H., Deviren V., Smith J.A., et al. Management of fixed sagittal plan deformity: results of the transpedicular wedge resection osteotomy. Spine (Phila Pa 1976). 2001;26(18):2036-2043.
9. Gao X., Gordon D., Zhang D., et al. CHD7 gene polymorphisms are associated with susceptibility to idiopathic scoliosis. Am J Hum Genet. 2008;80(5):957-965.
10. Gurnett C.A., Alaee F., Bowcock A., et al. Genetic linkage localizes an adolescent idiopathic scoliosis and pectus excavatum gene to 18q. Spine (Phila Pa 1976). 2009;34(2):E94-E100.
11. Lenke L.G., O’Leary P.T., Bridwell K.H., et al. Posterior vertebral column resection for severe pediatric deformity. Minimum two-year follow-up of thirty-five consecutive patients. Spine (Phila Pa 1976). 2009;34(20):2213-2221.
12. Suk S.I., Kim J.H., Kim W.J., et al. Posterior vertebral column resection for severe spinal deformities. Spine (Phila Pa 1976). 2002;27(21):2374-2382.
13. Bess R.S., Lenke L.G., Bridwell K.H., et al. Comparison of thoracic pedicle screw to hook instrumentation for the treatment of adult spinal deformity. Spine (Phila Pa 1976). 2007;32(5):555-561.
14. Cuartas E., Rasouli A., O’Brien M., et al. The use of all-pedicle-screw constructs in the treatment of adolescent idiopathic scoliosis. J Am Acad Orthop Surg. 2009;17(9):550-561.
15. Kim Y.J., Lenke L.G., Cho S.K., et al. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2004;29(18):2040-2048.
16. Lee S.M., Suk S.I., Chung E.R. Direct vertebral rotation: a new technique of three-dimensional deformity correction with segmental pedicle screw fixation in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2004;29(3):343-349.
17. Kuklo T.R., Potter B.K., Polly D.W.Jr., et al. Monaxial versus multiaxial thoracic pedicle screws in the correction of adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2005;30(18):2113-2120.
18. Good C.R., Lenke L.G., Bridwell K.H., et al. Can posterior-only surgery provide similar radiographic and clinical results as combined anterior (thoracotomy/thoracoabdominal)/posterior approaches for adult scoliosis? Spine (Phila Pa 1976). 2010;35(2):210-218.
19. Bridwell K.H. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine (Phila Pa 1976). 2006;31(Suppl 19):S171-S178.
20. Stoddard A., Osborn J.F. Scheuermann’s disease or spinal osteochondrosis: its frequency and relationship with spondylosis. J Bone Joint Surg [Br]. 1979;61(1):56-58.
21. Smith-Petersen M.N., Larson C.B., Aufranc O.E. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. Clin Orthop Relat Res. 1969;66:6-9.
22. Suk S.I., Chung E.R., Lee S.M., et al. Posterior vertebral column resection in fixed lumbosacral deformity. Spine (Phila Pa 1976). 2005;30(23):E703-E710.
23. Bridwell K.H., Lewis S.J., Edwards C., et al. Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine (Phila Pa 1976). 2003;28(18):2093-2101.
24. Bradford D.S., Tribus C.B. Vertebral column resection for the treatment of rigid coronal decompensation. Spine (Phila Pa 1976). 1997;22(14):1590-1599.
25. Lenke L.G., Sides B.A., Koester L.A., et al. Vertebral column resection for the treatment of severe spinal deformity. Clin Orthop Relat Res. 2010;268:687-699.
26. Ogilvie J. Adolescent idiopathic scoliosis and genetic testing. Curr Opin Pediatr. 2010;22(1):67-70.








