Spinal cord syndromes
Spinal cord disease and injury account for major long-term morbidity. The most common causes in young people are spinal cord trauma, which has a prevalence of 50 per 100 000, and multiple sclerosis affecting the spinal cord (60 per 100 000). The spinal cord terminates at the lower border of L1; most lumbar spine diseases cause radiculopathy and not spinal cord syndromes (p. 82).
Clinical presentation
The clinical presentation of spinal cord disease depends on:
A spinal lesion can only affect function below the level of the lesion. In assessing a patient, there will be a motor level (the highest myotome affected), a reflex level (the reflex with the highest segmental supply affected) and a sensory level. The lesion must be at or above the highest level. Pain at the level of the lesion may radiate along a nerve root level – myeloradiculopathy (p. 82) – and the spine may be tender at this level. Structural spine abnormalities, for example tumour, cause pain exacerbated by coughing, straining or sneezing. At the level of the lesion, reflexes may be lost from associated root or anterior horn cell involvement.
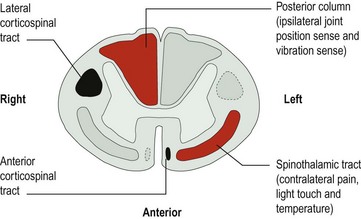
The parts of the spinal cord affected
The clinical picture will vary depending on which spinal tracts are affected. These tracts cross at different levels which determines which side is symptomatic. There are four main tracts involved (Fig. 1):
Patterns of spinal cord lesion
There are five main patterns of spinal cord lesion:
Pathological processes
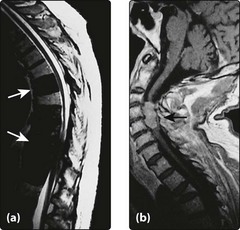
Neoplasms
These are usually extrinsic malignant metastases to the vertebrae and cause neurological compromise by expansion into the vertebral canal or by vertebral collapse (Fig. 2a). Common primary malignancies are bronchus, breast, myeloma, lymphoma and prostate. Primary extrinsic tumours are usually benign neurofibromas or meningiomas (Fig. 2b). Malignant lesions are painful and present acutely or subacutely. Benign lesions are usually painless and may develop very slowly.
Inflammatory spinal cord disease
This is most commonly due to multiple sclerosis (p. 84) but may represent an isolated episode, sometimes after infection. Other causes include sarcoidosis or collagen vascular diseases, for example Sjögren’s syndrome or systemic lupus erythematosus. They typically cause a neurological deficit evolving over a few days, but some slower syndromes occur.
Infection
This is a rare but important cause of acute, subacute or chronic syndromes. Paraspinal or epidural abscesses are painful and may present acutely (pyogenic) or more insidiously (tuberculous) with associated systemic symptoms (fever, sweats and weight loss). Brucellosis is an important cause of a subacute syndrome in parts of the world where unpasteurized milk is consumed. Myelopathy can develop chronically in infection with syphilis or HIV (p. 100). It is also seen in patients from the tropics with human T-cell lymphotropic virus I (HTLV-I) infection: ‘tropical spastic paraparesis’.
Degenerative cervical disc disease
This is the most common cause of spinal cord compression, especially in the neck (Fig. 3); its frequency increases with age. Cord compression can be due to:
 degeneration of interverterbral discs with extrusion of disc material into the spinal canal – acute disc
degeneration of interverterbral discs with extrusion of disc material into the spinal canal – acute discPain is variable and the rate of progression may be acute or chronic. There is often associated root disease (p. 82).
Treatment
Specific treatment
Radiotherapy and chemotherapy and sometimes surgery are used for the treatment of malignant tumours. High-dose corticosteroids are used for non-infective inflammatory causes. Surgical decompression at the foramen magnum may help syringomyelia, if there is an associated Chiari malformation. Long-term rehabilitation is discussed on page 122.