26 Somatization Disorder
Clinical Presentation
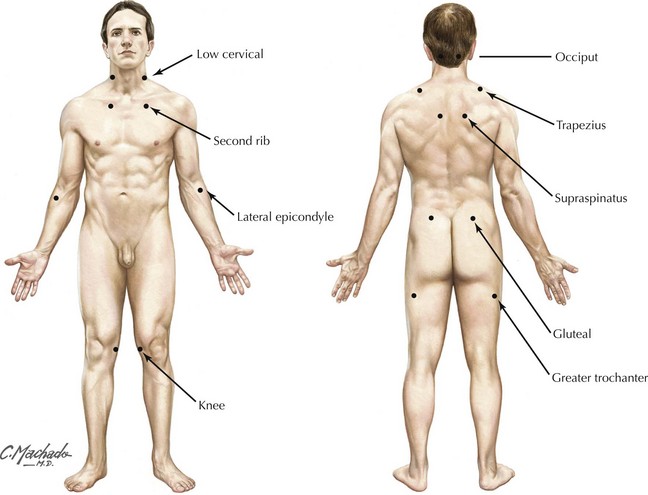
Fibromyalgia (see Fig. 28-1) is a common clinical syndrome typically found among women. It is characterized by complaints of widespread, migratory body pain, particularly myalgias and arthralgias (Fig. 26-1). These individuals frequently experience various combinations of psychological symptomatology, including an incapacitating fatigue, anxiety, depression, and poor sleeping. Often such patients are obsessed with finding a specific organic disorder as an explanation. In the neurologic clinic, one may see individuals who are convinced that they have a peripheral neuropathy, radiculopathies, or even complex regional pain syndromes. Because there is some clinical overlap with various neurologic and rheumatologic disorders, it is sometimes difficult to make a differential diagnosis in these patients between an organic versus somatoform disorder. As there is no specific neurologic testing modality that allows one to assign a formal pathophysiologic mechanism in these individuals, and the most detailed evaluations, including electromyography and muscle biopsy are normal, many neurologists conclude that these patients have a somatoform process. However, the neurologist must always maintain an open mind as each patient is evaluated.
Allen LA, Woolfolk RL, Escobar JI, et al. Cognitive-behavioral therapy for somatization disorder: a randomized controlled trial. Arch. Intern. Med. 2006;166(14):1512-1518.
Andrade C, Singh NM, Bhakta SG. Simultaneous true seizures and pseudoseizures. J Clin Psychiatry. 2006 Apr;67(4):673.
Eames P. Hysteria following brain injury. Journal of Neurology, Neurosurgery, and Psychiatry. 1992;55:1046-1053.
Kroenke K. Efficacy of treatment for somatoform disorders: a review of randomized controlled trials. Psychosom Med. 2007 Dec;69(9):881-888.