Smoke Inhalation and Thermal Injuries
After reading this chapter, you will be able to:
• List the anatomic alterations of the lungs associated with smoke inhalation and thermal injuries.
• Describe the causes of smoke inhalation and thermal injuries.
• List the cardiopulmonary clinical manifestations associated with smoke inhalation and thermal injuries.
• Describe the general management of smoke inhalation and thermal injuries.
• Describe the clinical strategies and rationales of the SOAPs presented in the case study.
• Define key terms and complete self-assessment questions at the end of the chapter and on Evolve.
Anatomic Alterations of the Lungs
Thermal Injury
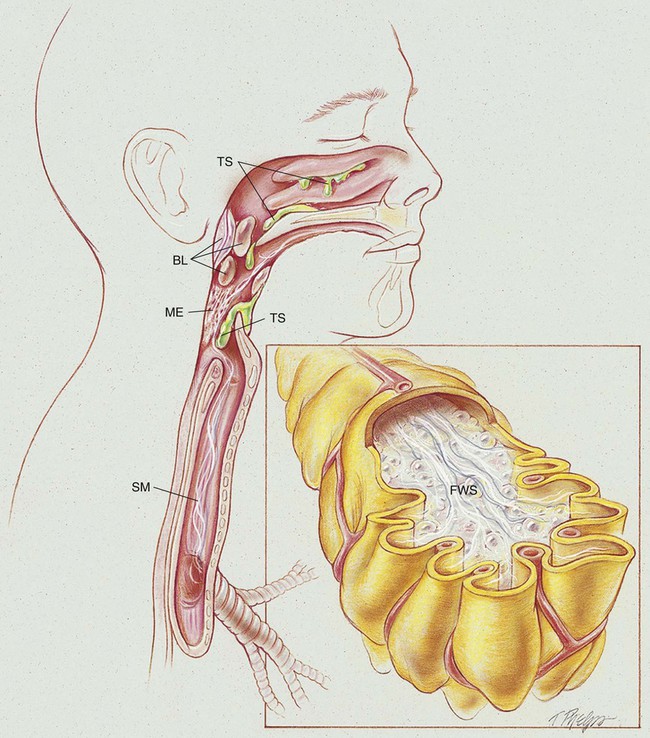
Even though thermal injury may occur with or without surface burns, the presence of facial burns is a classic predictor of thermal injury. Thermal injury to the upper airway results in blistering, mucosal edema, vascular congestion, epithelial sloughing, and accumulation of thick secretions. An acute upper airway obstruction (UAO) occurs in about 20% to 30% of hospitalized patients with thermal injury and is usually most marked in the supraglottic structures. When body surface burns require the rapid administration of resuscitative fluids, a UAO may develop rapidly (see Figure 41-1).
Smoke Inhalation Injury
Early Stage (0 to 24 Hours after Inhalation)
Smoke inhalation also may cause acute respiratory distress syndrome (ARDS), noncardiogenic high-permeability pulmonary edema—commonly referred to in smoke inhalation cases as “leaky alveoli.” Noncardiogenic pulmonary edema also may be caused by overhydration resulting from overzealous fluid resuscitation (see insert panel in Figure 41-1). In severe cases, ARDS also may occur early in the course of the pathology.
Late Stage (5 or More Days after Inhalation)
Thermal injury (upper airway—nasal cavity, oral cavity, and pharynx):
Smoke inhalation injury (tracheobronchial tree and alveoli):
• Inflammation of the tracheobronchial tree
• Excessive bronchial secretions and mucous plugging
• Decreased mucosal ciliary transport
• Alveolar edema and frothy secretions (pulmonary edema)
• COP (also called bronchiolitis obliterans organizing pneumonia [BOOP])
• Alveolar fibrosis, bronchial stenosis, bronchial polyps, bronchiolitis, and bronchiectasis (severe cases)
Pneumonia (Chapter 15) and pulmonary embolism (Chapter 20) often complicate smoke inhalation injury.
Etiology and Epidemiology
Smoke can result from either pyrolysis (smoldering in a low-oxygen environment) or combustion (burning, with visible flame, in an adequate-oxygen environment). Smoke is composed of a complex mixture of particulates, toxic gases, and vapors. The composition of smoke varies according to the chemical makeup of the material that is burning and the amount of oxygen being consumed by the fire. Table 41-1 lists some of the more common toxic substances produced by burning products that frequently are found in office, industrial, and residential buildings.
TABLE 41-1
Toxic Substances and Sources Commonly Associated with Fire and Smoke
| Substance | Source |
| Aldehydes (acrolein, acetaldehyde, formaldehyde) | Wood, cotton, paper |
| Organic acids (acetic and formic acids) | |
| Carbon monoxide, hydrogen chloride, phosgene | Polyvinylchloride (PVC) |
| Hydrogen cyanide, isocyanate | Polyurethanes |
| Hydrogen fluoride, hydrogen bromide | Fluorinated resins |
| Ammonia | Melamine resins |
| Oxides of nitrogen | Nitrocellulose film, fabrics |
| Benzene | Petroleum products |
| Carbon monoxide, carbon dioxide | Organic material |
| Sulfur dioxide | Sulfur-containing compounds |
| Hydrogen chloride | Fertilizer, textiles, rubber manufacturing |
| Chlorine | Swimming pool water |
| Ozone | Welding fumes |
| Hydrogen sulfide | Metal works, chemical manufacturing |
Body Surface Burns
Because the amount and severity of body surface burns play a major role in the patient’s risk of mortality and morbidity, an approximate estimate of the percentage of the body surface area burned is important. Table 41-2 lists the approximate percentage of surface area for various body regions of adults and infants. The severity and depth of burns usually are defined as follows:
TABLE 41-2
The Approximate Percentage of Body Surface Area (BSA) for Various Body Regions of Adults and Infants
| Anatomic Region | Percent of BSA in Adults | Percent of BSA in Infants |
| Entire head and neck | 9 | 18 |
| Each arm | 9 | 9 |
| Anterior trunk | 18 | 18 |
| Posterior trunk | 18 | 18 |
| Genitalia | 1 | 1 |
| Each leg | 18 | 13.5 |
First degree (minimal depth in skin): Superficial burn, damage limited to the outer layer of epidermis. This burn is characterized by reddened skin, tenderness, and pain. Blisters are not present. Healing time is about 6 to 10 days. The result of healing is normal skin.
Second degree (superficial to deep thickness of skin): Burns in which damage extends through the epidermis and into the dermis but is not of sufficient extent to interfere with regeneration of epidermis. If secondary infection results, the damage from a second-degree burn may be equivalent to that of a third-degree burn. Blisters usually are present. Healing time is 7 to 21 days. The result of healing ranges from normal to a hairless and depigmented skin with a texture that is normal, pitted, flat, or shiny.
Third degree (full thickness of skin including tissue beneath skin): Burns in which both epidermis and dermis are destroyed, with damage extending into underlying tissues. Tissue may be charred or coagulated. Healing may occur after 21 days or may never occur without skin grafting if the burned area is large. The resultant damage heals with hypertrophic scars (keloids) and chronic granulation.
General Management Smoke Inhalation and Thermal Injuries
General Emergency Care
Fluid resuscitation with Ringer’s lactate solution is usually initiated according to the Parkland Formula—4 mL/kg of body weight for each percent of body surface area burned (see Table 41-2) over a 24-hour period. The patient’s hemodynamic status will usually remain stable at this fluid replacement rate, with an average urine output target of 30 to 50 mL/hr and a central venous pressure (CVP) target of 2 to 6 mm Hg. Because this process often leads to overhydration and acute UAO and pulmonary edema, the patient’s fluid and electrolyte status (weight, input and output, and laboratory values) must be monitored carefully.
Respiratory Care Treatment Protocols
Oxygen Therapy Protocol
See Oxygen Therapy Protocol, Protocol 9-1.
Bronchopulmonary Hygiene Therapy Protocol
Because of the excessive mucous production and accumulation in the intermediate and late stages of smoke inhalation injuries, a number of respiratory therapy modalities may be used to enhance the mobilization of bronchial secretions. However, even though chest physical therapy is an excellent treatment modality to mobilize secretions, patients with severe chest burns or recent skin grafts do not tolerate chest percussion and vibration (see Bronchopulmonary Hygiene Therapy Protocol, Protocol 9-2).
Lung Expansion Therapy Protocol
Lung expansion techniques commonly are used to offset the alveolar atelectasis and consolidation associated with smoke inhalation injuries. The administration of continuous positive airway pressure (CPAP) via an endotracheal tube or mask (when the patient has no facial or neck burns) may help minimize the development of pulmonary edema. CPAP also supports the edematous airway and maintains or increases the patient’s functional residual capacity (see Lung Expansion Therapy Protocol, Protocol 9-3).
Aerosolized Medication Protocol
Both sympathomimetic and parasympatholytic agents commonly are used to produce vasoconstriction of the mucosa and to offset bronchial smooth muscle constriction. Bland (saline) aerosols may be helpful. Mucolytics and antiinflammatory agents also may be administered as part of the Aerosolized Medication Protocol (see Protocol 9-4).
Mechanical Ventilation Protocol
Mechanical ventilation with positive end-expiratory pressure (PEEP) usually is required for patients who develop pulmonary edema, ARDS, and pneumonia. Mechanical ventilation should be implemented in the presence of acute or impending ventilatory failure (see Mechanical Ventilation Protocols, Protocol 9-5, Protocol 9-6, and Protocol 9-7).
Respiratory Assessment and Plan
S Complains of productive cough, substernal chest pain when coughing, and dyspnea.
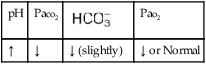
O Afebrile. BP 120/65, P 119 and regular, RR 35. Bilateral crackles, rhonchi, and expiratory wheezing. On 60% O2 by HAFOE mask: pH 7.54, Paco2 25,  20, and Pao2 38. CXR: Bilateral patchy infiltrates and consolidation. No cardiomegaly. Bronchoscopy—blackish eschar in oropharynx; reddened and inflamed larynx, trachea, and large airways. Thick, whitish-grey secretions noted.
20, and Pao2 38. CXR: Bilateral patchy infiltrates and consolidation. No cardiomegaly. Bronchoscopy—blackish eschar in oropharynx; reddened and inflamed larynx, trachea, and large airways. Thick, whitish-grey secretions noted.
• Smoke inhalation with thermal burns of the oropharynx, larynx, and large airways (history and bronchoscopy)
• Alveolar infiltrates and consolidation (CXR)
• Acute alveolar hyperventilation with severe hypoxemia (ABGs)
• Impending ventilatory failure (general history and clinical trend)
P Confer with attending physician to intubate and initiate mechanical ventilation care per Mechanical Ventilation Protocol. Oxygen Therapy Protocol: Fio2 at 1.0 via nonrebreather mask. Aerosolized Medication Protocol and Bronchopulmonary Hygiene Protocol: albuterol premix 2.0 mL via med. neb. q2h (alternate with epinephrine 6 drops in 2.0 mL normal saline). Gentle nasotracheal and oral suctioning after med. neb. treatments and prn. Check I&O status and daily weights. If physician commits patient to ventilator, consider in-line ultrasonic nebulizer treatments, for 30 min q4h.
Respiratory Assessment and Plan
S Complains of shortness of breath with any activity.
O Vital signs stable. Crackles heard over both lung bases. Some expiratory prolongation. ABGs (spontaneous breathing) (Fio2 = 0.35 by HAFOE): pH 7.46, Paco2 38,  24, and Pao2 63. Spo2 falls to 85% with exercise. PEFR 40% of predicted. CXR: Improvement in patchy lung infiltrates.
24, and Pao2 63. Spo2 falls to 85% with exercise. PEFR 40% of predicted. CXR: Improvement in patchy lung infiltrates.
P Complete pulmonary function tests ordered. Up-regulate Oxygen Therapy Protocol (increase Fio2 to 0.40 via a HAFOE). If obstructive pulmonary disease is confirmed, restart Bronchial Hygiene Protocol and Aerosolized Medication Protocol.
Discussion
At the time of the first assessment, the patient demonstrated most of the pathophysiologic correlates of smoke inhalation and thermal injuries to the lung. His dyspnea reflected the increased work of breathing associated with Bronchospasm (see Figure 9-11), Increased Alveolar-Capillary Membrane Thickness (see Figure 9-10), and Excessive Bronchial Secretions (see Figure 9-12). The bronchospasm was treated with the vigorous use of both bronchodilator (albuterol) and decongestant (epinephrine) aerosols. The excessive bronchial secretions were treated with ultrasonic bland aerosols and airway suctioning. No specific treatment was available for the changes that occurred in the alveolar-capillary membrane



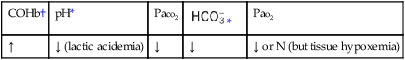
 values will be lower than expected for a particular Pa
values will be lower than expected for a particular Pa
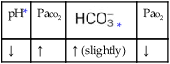
 values will be lower than expected for a particular Pa
values will be lower than expected for a particular Pa


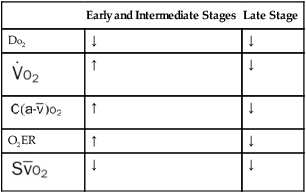
 may appear normal or increased when in actuality the tissue cells are extremely hypoxic. Typically these problems are not present during the intermediate and late stages in the presence of appropriate treatment.
may appear normal or increased when in actuality the tissue cells are extremely hypoxic. Typically these problems are not present during the intermediate and late stages in the presence of appropriate treatment.
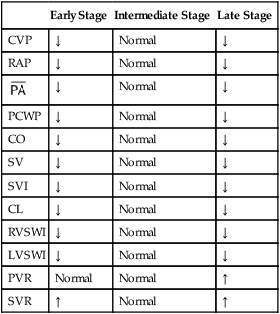
 , mean pulmonary artery pressure; PCWP, pulmonary capillary wedge pressure; PVR, pulmonary vascular resistance; RAP, right atrial pressure; RVSWI, right ventricular stroke work index; SV, stroke volume; SVI, stroke volume index; SVR, systemic vascular resistance.
, mean pulmonary artery pressure; PCWP, pulmonary capillary wedge pressure; PVR, pulmonary vascular resistance; RAP, right atrial pressure; RVSWI, right ventricular stroke work index; SV, stroke volume; SVI, stroke volume index; SVR, systemic vascular resistance. , CWP, CO, SV, SVI, CI, RVSWI, and LVSWI reflect the reduction in pulmonary intravascular and cardiac filling volumes. Hypovolemia causes a generalized peripheral vasoconstriction, which is reflected in an elevated SVR. When appropriate fluid resuscitation is administered, the patient’s hemodynamic indices usually are normal during the intermediate stage.
, CWP, CO, SV, SVI, CI, RVSWI, and LVSWI reflect the reduction in pulmonary intravascular and cardiac filling volumes. Hypovolemia causes a generalized peripheral vasoconstriction, which is reflected in an elevated SVR. When appropriate fluid resuscitation is administered, the patient’s hemodynamic indices usually are normal during the intermediate stage.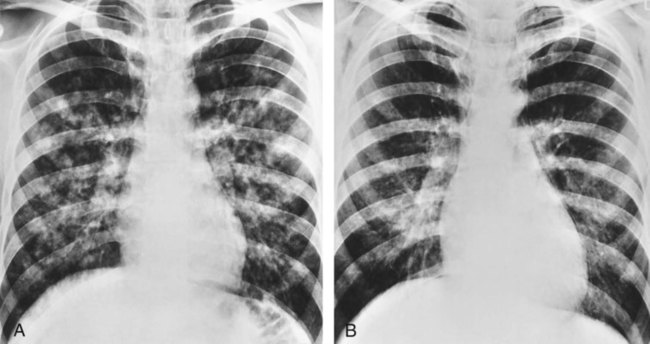
 21, and Pa
21, and Pa 20, and Pa
20, and Pa 24, and Pa
24, and Pa