Chapter 38 Skin and Soft Tissue Infections
General Principles
1 If patients with skin or soft tissue infection are seen with signs of systemic toxicity, what laboratory studies should be undertaken?
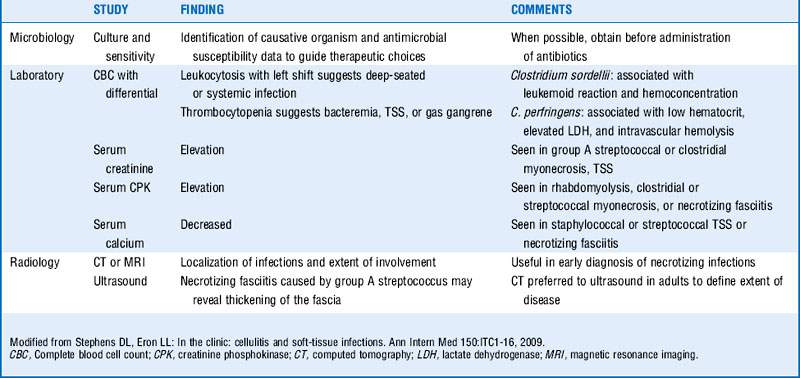
Blood cultures, cultures of drainage from skin infection site, complete blood cell count with differential, and serum creatinine, bicarbonate, creatine phosphokinase, glucose, albumin, and calcium levels should be obtained. (See Table 38-1.)
3 Which common causative organisms have shown emerging antibiotic resistance?
 Staphylococcus aureus (methicillin resistance with resistance to all β-lactams except ceftaroline): Assume resistance because of high prevalence of methicillin-resistant S. aureus (MRSA), both community and hospital acquired.
Staphylococcus aureus (methicillin resistance with resistance to all β-lactams except ceftaroline): Assume resistance because of high prevalence of methicillin-resistant S. aureus (MRSA), both community and hospital acquired.
 Streptococcus pyogenes (erythromycin resistance): Resistance is increasing to macrolides (approximately 7% in the United States, 2% to 32% reported in Europe), although the majority remain susceptible to clindamycin, and all are susceptible to penicillin.
Streptococcus pyogenes (erythromycin resistance): Resistance is increasing to macrolides (approximately 7% in the United States, 2% to 32% reported in Europe), although the majority remain susceptible to clindamycin, and all are susceptible to penicillin.
Cellulitis
6 Lack of response to initial therapy could signify what?
 If a patient does not respond to initial therapy, consider the possibility of resistant strains, atypical organisms, deeper processes such as necrotizing fasciitis or abscess (which may require surgical intervention), as well as underlying conditions such as diabetes, chronic venous insufficiency, or lymphedema (which may slow the clinical response to antimicrobial therapy).
If a patient does not respond to initial therapy, consider the possibility of resistant strains, atypical organisms, deeper processes such as necrotizing fasciitis or abscess (which may require surgical intervention), as well as underlying conditions such as diabetes, chronic venous insufficiency, or lymphedema (which may slow the clinical response to antimicrobial therapy).
 Timely administration of appropriate antibiotic therapy is essential. One study found that each hour of delay between documented hypotension and administration of antibiotics was associated with an average decrease in survival of 7.6% across all sources of infection; subgroup analysis for patients with skin and soft tissue infections demonstrated a significant increase in the adjusted odds ratio of death. This same study found that time to initiation of effective antimicrobial therapy was the strongest predictor of hospital survival. Despite the impact of delayed therapy, the study found that the median time to effective therapy was 6 hours.
Timely administration of appropriate antibiotic therapy is essential. One study found that each hour of delay between documented hypotension and administration of antibiotics was associated with an average decrease in survival of 7.6% across all sources of infection; subgroup analysis for patients with skin and soft tissue infections demonstrated a significant increase in the adjusted odds ratio of death. This same study found that time to initiation of effective antimicrobial therapy was the strongest predictor of hospital survival. Despite the impact of delayed therapy, the study found that the median time to effective therapy was 6 hours.
7 What risk factors predispose individuals to development of cellulitis?
 Previous episodes of cellulitis in the same location (may result in damage to lymphatics)
Previous episodes of cellulitis in the same location (may result in damage to lymphatics)
 Toe-web abnormalities (i.e., maceration, tinea pedis)
Toe-web abnormalities (i.e., maceration, tinea pedis)
 Breach in skin barrier, such as ulcers, trauma, fungal infection, eczema
Breach in skin barrier, such as ulcers, trauma, fungal infection, eczema
 Surgical procedures that affect lymphatic drainage such as radical mastectomy with lymph node dissection or coronary artery bypass graft for which the saphenous vein has been harvested
Surgical procedures that affect lymphatic drainage such as radical mastectomy with lymph node dissection or coronary artery bypass graft for which the saphenous vein has been harvested
 Chronic medical conditions such as diabetes, arterial insufficiency, chronic venous insufficiency, chronic renal disease, neutropenia, cirrhosis, hypogammaglobulinemia
Chronic medical conditions such as diabetes, arterial insufficiency, chronic venous insufficiency, chronic renal disease, neutropenia, cirrhosis, hypogammaglobulinemia
8 What organisms are associated with cellulitis in:
 Cat or dog bites? Pasteurella multocida, Capnocytophaga canimorsus
Cat or dog bites? Pasteurella multocida, Capnocytophaga canimorsus
 Fresh water exposure? Aeromonas hydrophila
Fresh water exposure? Aeromonas hydrophila
 Saltwater exposure? Vibrio vulnificus and other vibrios
Saltwater exposure? Vibrio vulnificus and other vibrios
 Exposure to fish farming and aquaculture? Streptococcus iniae
Exposure to fish farming and aquaculture? Streptococcus iniae
 Exposure to meatpacking or shellfish? Erysipelothrix rhusiopathiae
Exposure to meatpacking or shellfish? Erysipelothrix rhusiopathiae
 Preorbital cellulitis in children? Haemophilus influenzae
Preorbital cellulitis in children? Haemophilus influenzae
 Hosts with deficiencies in cell-mediated immunity? Cryptococcus neoformans
Hosts with deficiencies in cell-mediated immunity? Cryptococcus neoformans
Cutaneous abscesses
9 How are abscesses managed?
 Large abscesses should be incised and drained, with careful attention to the potential for loculated cavities (and the disruption of these cavities through probing of the pus pocket).
Large abscesses should be incised and drained, with careful attention to the potential for loculated cavities (and the disruption of these cavities through probing of the pus pocket).
 Once drained, the lesion can be left packed or unpacked depending on its extent.
Once drained, the lesion can be left packed or unpacked depending on its extent.
 In the absence of multiple lesions, gangrene, impaired host defenses, fever, or systemic signs and symptoms of infection, once a cutaneous abscess is drained, systemic antimicrobial therapy may not be needed.
In the absence of multiple lesions, gangrene, impaired host defenses, fever, or systemic signs and symptoms of infection, once a cutaneous abscess is drained, systemic antimicrobial therapy may not be needed.
Necrotizing skin and soft tissue infections
11 Is necrotizing fasciitis usually monomicrobial or polymicrobial?
 Both. Organisms seen in monomicrobial infection include S. pyogenes, V. vulnificus, A. hydrophila, S. aureus, and anaerobic streptococci. An average of five different organisms is cultured in the case of polymicrobial infections. Surgical procedures involving the bowels, penetrating abdominal trauma, decubitus ulcer, perianal abscesses, infection at the site of injection drug use, and spread for a Bartholin abscess are associated with polymicrobial necrotizing fasciitis.
Both. Organisms seen in monomicrobial infection include S. pyogenes, V. vulnificus, A. hydrophila, S. aureus, and anaerobic streptococci. An average of five different organisms is cultured in the case of polymicrobial infections. Surgical procedures involving the bowels, penetrating abdominal trauma, decubitus ulcer, perianal abscesses, infection at the site of injection drug use, and spread for a Bartholin abscess are associated with polymicrobial necrotizing fasciitis.
 Necrotizing fasciitis is categorized as type I (usually mixed aerobic and anaerobic) and type II (caused usually by group A Streptococcus but also S. aureus).
Necrotizing fasciitis is categorized as type I (usually mixed aerobic and anaerobic) and type II (caused usually by group A Streptococcus but also S. aureus).
 Vibrio infections have been associated with saltwater exposures. Individuals with hepatic dysfunction are at greater risk for Vibrio infection.
Vibrio infections have been associated with saltwater exposures. Individuals with hepatic dysfunction are at greater risk for Vibrio infection.
12 Which organisms cause gas gangrene?
 Clostridial gas gangrene, or myonecrosis, is caused by Clostridium perfringens, Clostridium septicum, Clostridium histolyticum, and Clostridium novyi.
Clostridial gas gangrene, or myonecrosis, is caused by Clostridium perfringens, Clostridium septicum, Clostridium histolyticum, and Clostridium novyi.
 Predisposing factors include penetrating trauma, crush injuries, and intravenous (IV) drug abuse.
Predisposing factors include penetrating trauma, crush injuries, and intravenous (IV) drug abuse.
 C. perfringens is the most common cause of trauma-related gas gangrene—symptoms develop within 24 hours of infection. C. septicum is the most common cause of spontaneous gangrene and is associated with neutropenia and gastrointestinal malignancies.
C. perfringens is the most common cause of trauma-related gas gangrene—symptoms develop within 24 hours of infection. C. septicum is the most common cause of spontaneous gangrene and is associated with neutropenia and gastrointestinal malignancies.
 Antimicrobial therapy includes clindamycin and penicillin because 5% of strains of C. perfringens are clindamycin-resistant.
Antimicrobial therapy includes clindamycin and penicillin because 5% of strains of C. perfringens are clindamycin-resistant.
 Rapid surgical debridement is the most important determinant of outcome.
Rapid surgical debridement is the most important determinant of outcome.
13 What is appropriate antimicrobial therapy for necrotizing skin and soft tissue infections?
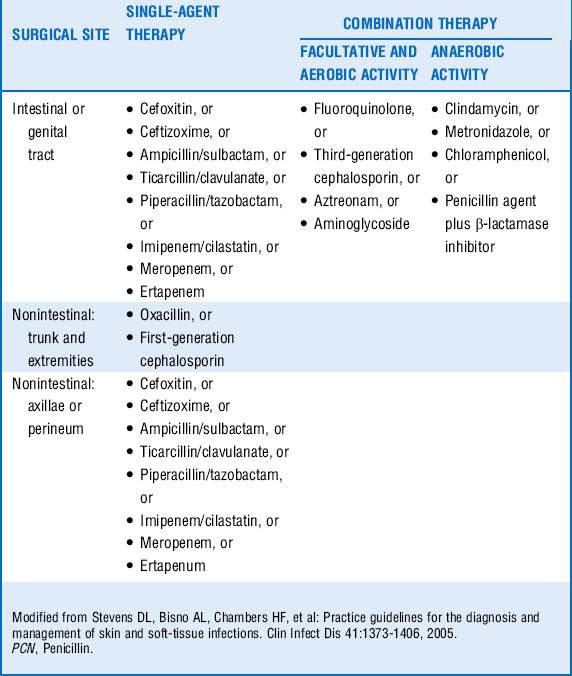
 For mixed infection, ampicillin-sulbactam plus clindamycin plus ciprofloxacin or a third-generation cephalosporin. For patients with severe allergies to penicillin, clindamycin or metronidazole plus an aminoglycoside or fluoroquinolone can be substituted.
For mixed infection, ampicillin-sulbactam plus clindamycin plus ciprofloxacin or a third-generation cephalosporin. For patients with severe allergies to penicillin, clindamycin or metronidazole plus an aminoglycoside or fluoroquinolone can be substituted.
 For streptococcal infections, including streptococcal toxic shock syndrome (TSS), treat with penicillin plus clindamycin. In patients with severe allergies to penicillin, vancomycin, linezolid, quinupristin-dalfopristin, or daptomycin can be substituted for penicillin.
For streptococcal infections, including streptococcal toxic shock syndrome (TSS), treat with penicillin plus clindamycin. In patients with severe allergies to penicillin, vancomycin, linezolid, quinupristin-dalfopristin, or daptomycin can be substituted for penicillin.
 The value of IV immunoglobulin (IVIG) in these circumstances has yet to be fully defined. One study showed no improved survival in patients with TSS randomly assigned to receive IVIG, whereas a retrospective cohort analysis did demonstrate improved outcomes. A more recent study in the pediatric population found no difference in outcomes for patients treated for TSS with and without IVIG.
The value of IV immunoglobulin (IVIG) in these circumstances has yet to be fully defined. One study showed no improved survival in patients with TSS randomly assigned to receive IVIG, whereas a retrospective cohort analysis did demonstrate improved outcomes. A more recent study in the pediatric population found no difference in outcomes for patients treated for TSS with and without IVIG.
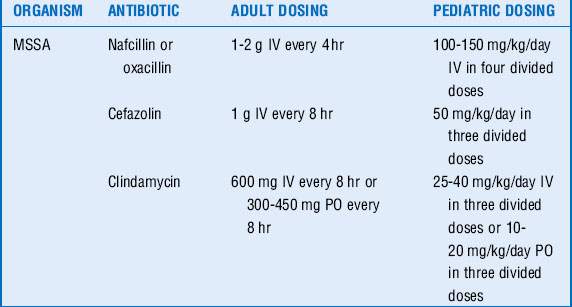
 For S. aureus infections, nafcillin, oxacillin, or cefazolin are drugs of choice for susceptible strains. If concern exists for methicillin resistance, vancomycin or clindamycin are options.
For S. aureus infections, nafcillin, oxacillin, or cefazolin are drugs of choice for susceptible strains. If concern exists for methicillin resistance, vancomycin or clindamycin are options.
Infections after animal bites
14 Which organisms are commonly isolated after cat bites?
Pasteurella spp., most commonly, but these infections are usually polymicrobial. Common organisms found in the oral cavity of cats include Bartonella henselae, Moraxella spp., staphylococci, streptococci, and anaerobes. Cats with outdoor exposure can additionally carry Leptospira, Listeria, and Nocardia spp. as well as Francisella tularensis, Streptobacillus moniliformis, Erysipelothrix rhusiopathiae, and Coxiella burnetii, but these organisms are uncommon causes of cat-bite infections. (See Table 38-3.)
| Aerobes | Anaerobes | |
|---|---|---|
| Cat bites | Pasteurella spp., Streptococcus spp., Staphylococcus spp., Moraxella spp. | Fusobacterium spp., Bacteroides spp., Porphyromonas spp. |
| Dog bites | Pasteurella spp., Streptococcus spp., Staphylococcus spp., Neisseria spp. | Fusobacterium spp., Bacteroides spp., Porphyromonas spp., Prevotella spp., Capnocytophaga spp. |
Note: Most infections include a mix of aerobes and anaerobes.
Data from Oehler RL, Velez AP, Mizrachi M, et al: Bite-related and septic syndromes caused by cats and dogs. Lancet Infect Dis 9:439-447, 2009.
Infections after human bites
22 What are the potential complications of human bite infections?
 Deep infection of the synovium, joint capsule, and bone in the case of closed-fist injuries—early evaluation by a hand surgeon is recommended. Hospitalization for empiric IV antibiotics may be needed and should be directed at S. aureus, Haemophilus spp., E. corrodens, and β-lactamase–producing anaerobes.
Deep infection of the synovium, joint capsule, and bone in the case of closed-fist injuries—early evaluation by a hand surgeon is recommended. Hospitalization for empiric IV antibiotics may be needed and should be directed at S. aureus, Haemophilus spp., E. corrodens, and β-lactamase–producing anaerobes.
 Radiographs can be useful in identifying foreign bodies (i.e., retained teeth).
Radiographs can be useful in identifying foreign bodies (i.e., retained teeth).
Surgical site infections
23 How common are surgical site infections (SSIs), and what factors are related to their incidence?
 The development of a SSI depends on a variety of factors, including location and type of surgery; duration of the surgery; whether or not the wound was classified as “clean,” “clean-contaminated,” “contaminated,” or “dirty,” and a series of patient-related risk factors, including diabetes, obesity, smoking, colonization or nasal carriage with S. aureus, and systemic steroids, among other factors.
The development of a SSI depends on a variety of factors, including location and type of surgery; duration of the surgery; whether or not the wound was classified as “clean,” “clean-contaminated,” “contaminated,” or “dirty,” and a series of patient-related risk factors, including diabetes, obesity, smoking, colonization or nasal carriage with S. aureus, and systemic steroids, among other factors.
24 What techniques have been shown to reduce the risk of SSI?
 Proper skin preparation: avoidance of preoperative use of a razor for removing hair at the incision site (clippers should be used if hair removal is needed), use of chlorhexidine-alcohol or iodophor-alcohol skin antiseptics
Proper skin preparation: avoidance of preoperative use of a razor for removing hair at the incision site (clippers should be used if hair removal is needed), use of chlorhexidine-alcohol or iodophor-alcohol skin antiseptics
 Surgical techniques: gentle traction during surgery, effective hemostasis, removal of devitalized tissues, obliteration of dead space, irrigation of tissues, use of nonabsorbable monofilament suture material, closed-suction drains, and wound closure without tension
Surgical techniques: gentle traction during surgery, effective hemostasis, removal of devitalized tissues, obliteration of dead space, irrigation of tissues, use of nonabsorbable monofilament suture material, closed-suction drains, and wound closure without tension
 Antimicrobial prophylaxis: preoperative administration of antibiotics within 1 hour before the incision is recommended. Cefazolin is a common choice, with clindamycin or vancomycin in patients allergic to penicillin. Vancomycin should also be considered in the case of institutions where the rate of MRSA is high and in patients with known history of or current infection with MRSA (See Table 38-4).
Antimicrobial prophylaxis: preoperative administration of antibiotics within 1 hour before the incision is recommended. Cefazolin is a common choice, with clindamycin or vancomycin in patients allergic to penicillin. Vancomycin should also be considered in the case of institutions where the rate of MRSA is high and in patients with known history of or current infection with MRSA (See Table 38-4).
Key Points Skin and Soft Tissue Infections
1. Selection of empiric antimicrobial therapy. In a patient with skin and soft tissue infection, consider host factors including comorbidities, prior microbiologic history, and epidemiologic background.
2. Risk factors that predispose to cellulitis. Obesity, prior cellulitis in the same location, toe-web abnormalities, breach in skin barrier, surgical procedures that affect lymphatic drainage, diabetes, arterial insufficiency, chronic venous insufficiency, chronic renal disease, neutropenia, cirrhosis, and hypogammaglobulinemia are predisposing factors.
3. Appropriate antimicrobial therapy for streptococcal TSS. Penicillin and clindamycin are first-line therapy for patients with severe allergies to penicillin, vancomycin, linezolid, quinupristin-dalfopristin, or daptomycin can be substituted. For S. aureus TSS, use vancomycin if concern exists for MRSA.
4. Human bites. Always treat with prophylactic antibiotics; involve surgical service early if complications including deep infection are suspected.
5. SSI rates. SSI rates depend on many factors, including location and type of surgery; duration of the surgery; surgical classification of the wound, and a series of patient-related risk factors.
1 Anaya D.A., Dellinger E.P. Necrotizing soft-tissue infection: diagnosis and management. Clin Infect Dis. 2007;44:705–710.
2 Chen I., Kaufisi P., Erdem G. Emergence of erythromycin- and clindamycin-resistant Streptococcus pyogenes emm 90 strains in Hawaii. J Clin Microbiol. 2011;49:439–441.
3 Henry F.P., Purcell E.M., Eadie P.A. The human bite injury: a clinical audit and discussion regarding management of this alcohol-fueled phenomenon. Emerg Med J. 2007;24:455–458.
4 Kumar A., Roberts D., Wood K.E., et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34:1589–1596.
5 Liu C., Bayer A., Cosgrove S.E., et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011;52:1–38.
6 Mangram A.J., Horan T.C., Pearson M.L., et al. Guideline for prevention of surgical site infection, 1999. Infect Control Hosp Epidemiol. 1999;20:247–278.
7 Oehler R.L., Velez A.P., Mizrachi M., et al. Bite-related and septic syndromes caused by cats and dogs. Lancet Infect Dis. 2009;9:439–447.
8 Seaton R.A. Daptomycin: rationale and role in the management of skin and soft tissue infections. J Antimicrob Chemother. 2008;62(suppl 3):iii15–iii23.
9 Sebeny P.J., Riddle M.S., Peterson K. Acinetobacter baumannii skin and soft-tissue infection associated with war trauma. Clin Infect Dis. 2008;47:444–449.
10 Shah S.S., Hall M., Srivastava R., et al. Intravenous immunoglobulin in children with streptococcal toxic shock syndrome. Clin Infect Dis. 2009;49:1369–1376.
11 Stevens D.L., Bisno A.L., Chambers H.F., et al. Practice guidelines for the diagnosis and management of skin and soft-tissue infections. Clin Infect Dis. 2005;41:1373–1406.
12 Stevens D.L., Eron L.L. In the clinic: cellulitis and soft-tissue infections. Ann Intern Med. 2009;150:ITC1–16.
13 Talan D.A., Citron D.M., Abrahamian F.M., et al. Bacteriologic analysis of infected dog and cat bites. N Engl J Med. 1999;340:85–92.
14 Tsai Y.H., Wen-Wei Hsu R., Huang K.C., et al. Comparison of necrotizing fasciitis and sepsis caused by Vibrio vulnificus and Staphylococcus aureus. J Bone Joint Surg Am. 2011;93:274–284.
15 Winner J.S., Gentry C.A., Machado L.J., et al. Aztreonam treatment of Pasteurella multocida cellulitis and bacteremia. Ann Pharmacother. 2003;37:392–394.