Skeletal injuries
Anatomy and physiology
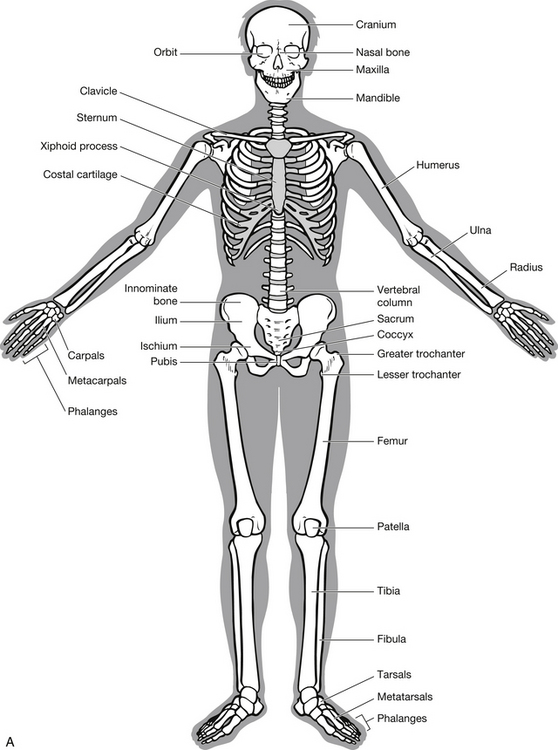
In order to appreciate the impact of injury, it is necessary for the emergency nurse to have a thorough understanding of the make-up and purpose of the human skeleton (Fig. 6.1) and skeletal muscle. The skeleton comprises two parts with specific functions:
• the axial skeleton, consisting of the skull, vertebral column, ribs and sternum – supports and protects vital organs
• the appendicular skeleton, consisting of the shoulder girdle, pelvic girdle and limbs – provides shape and facilitates movement.
Bone is a form of connective tissue comprising three major components:
• organic matrix of collagen – creates tensile strength
• mineral matrix of calcium and phosphate – creates rigidity and strength
• bone cells, including osteoblasts, osteoclasts, osteocytes and fibroblasts.
Compact cortical bone is found on outer parts of all bone; it forms the shaft of long bones and encloses marrow cavities (Fig. 6.2). Compact bone contains Haversian systems consisting of Haversian canals, blood vessels, connective tissues, nerve fibers and lymphatic vessels with osteocytes that facilitate the exchange of nutrients and waste. Cancellous bone is found at the ends of the long bone and in the vertebrae and flat bones. Cancellous bone is organized in a lattice system known as trabeculae and contains fewer Haversian canals. Red and fatty bone marrow fills the cavities in this lattice.
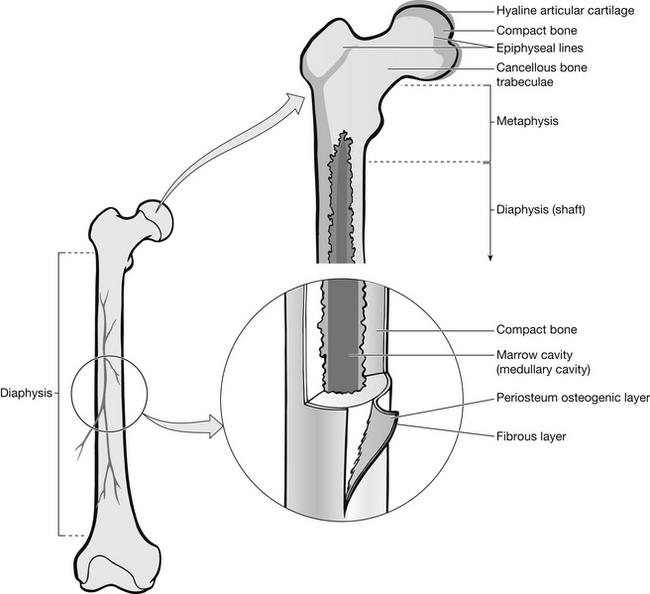
Figure 6.2 Cross-section of bone.
Bone cells
Osteoclasts are found near the bone surface. They destroy dead bone and are responsible for reabsorption of bone. They are very mobile and are found in great numbers where bone is undergoing erosion. Their activity is controlled by a number of hormones including parathyroid and thyroxin.
Joints
Cartilaginous joints permit limited movement because of flexible cartilage between bones. The symphyses have cartilage pads, or discs, between bones, e.g., symphysis pubis or intervertebral joints. Complex ligament arrangements stabilize these cartilage pads to limit movement and facilitate recoil. Synchondroses are cartilage joints that ossify into bone in adulthood preventing movement, e.g., epiphysis of long bone.
Synovial joints form most of the body’s joints. They are further classified by the type and range of movement they allow (see Table 6.1). All synovial joints have a number of similar structured features. They are enclosed in a capsule that is lined with a synovial membrane, which secretes synovial fluid. Bone ends are not in direct contact and are covered by hyaline cartilage. The fibrous capsule is held in place by a number of ligaments.
Table 6.1
Classification of synovial joints
| Type of joint | Site | Range of movement |
| Hinge | Elbow Fingers Ankle Toes |
Flexion Extension |
| Pivot | Vertebral column | Rotation |
| Gliding | Shoulder girdle Vertebral column |
Limited motion in several directions |
| Ball and socket | Hip Shoulder |
Extensive range ofmovement: flexion, extension, rotation |
| Saddle | Hand Base of thumb |
Flexion Extension Abduction Adduction Opposition |
| Ellipson | Wrist Hand Foot |
Flexion Extension Abduction Adduction Opposition |
Muscular system
Muscle tissue is formed to convert chemical energy into mechanical contraction, creating movement. Movements are generated both at joints and in soft tissue. Muscles also assist in maintaining body posture and muscular activity is associated with maintaining body heat.
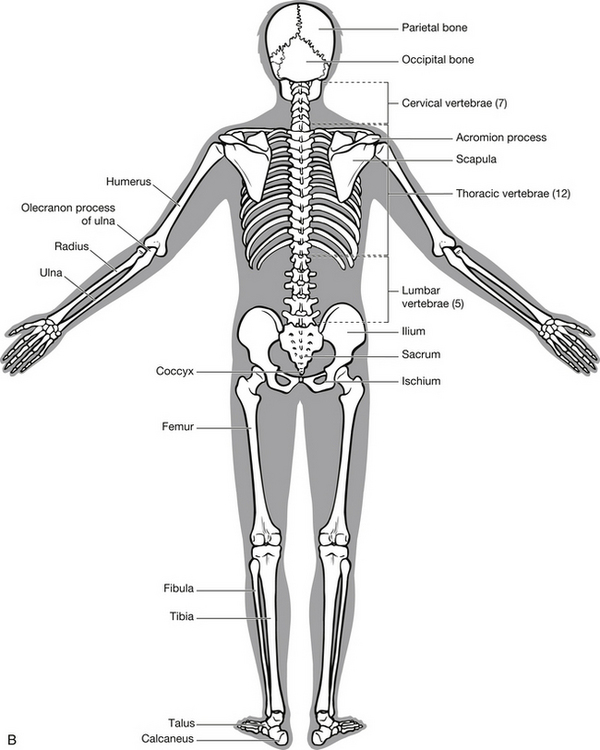
Pelvic injury
The pelvis is designed to provide structure, strength for weight-bearing and protection of internal organs. It houses the rectum, bladder and, in women, the reproductive organs. The pelvis forms a ring, comprising the sacrum and two innominate bones, each made up of an ilium, pubic bone and ischium (Fig. 6.3).
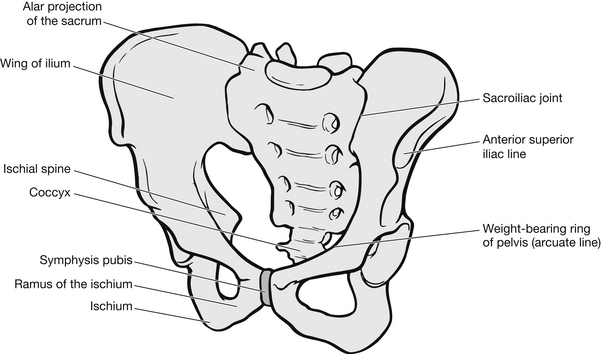
Figure 6.3 The pelvis.
Mechanism of injury
Major trauma to the pelvic girdle is relatively uncommon and accounts for approximately 3–6 % of all skeletal injuries and 20 % of polytrauma cases (Smith 2005); however, the mortality associated with major pelvic fractures may reach 57 % where shock is present on the patient’s arrival (Starr et al. 2002). Most pelvic fractures are caused by motorcycle accidents, accidents involving pedestrians, direct crush injuries, or falls from a height (American College of Surgeons 2008). Falls are also the second highest cause of unintentional death after motor vehicles (Middleton 2011).
Fracture patterns
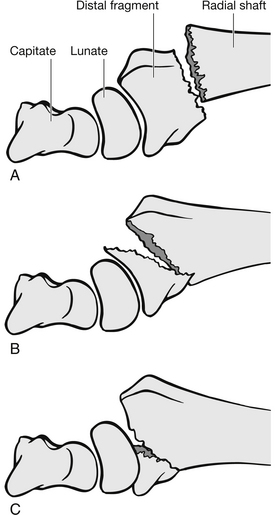
Lateral compression (LC) fractures (graded I, II, III) are caused by a side impact, usually to motorcyclists or pedestrians in collision with vehicles. A compression fracture of the pubic bone or rami is combined with compression fracture on the side of impact (Fig. 6.4A). With greater force of impact, the iliac wing on the side of the impact will also break; this is a grade II injury (Fig. 6.4B). A grade III injury involves an additional fracture on the opposite side to the impact (Fig. 6.4C).
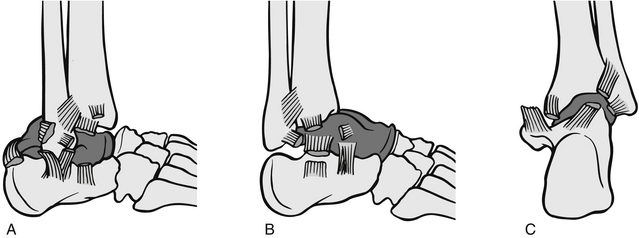
Anteroposterior compression (APC) fractures (graded I, II, III) are caused by direct pressure or crushing and result in the pelvis opening outwards from wings rather like a book. The result is the fracturing of the pubis or rami together with sacroiliac distribution. In grade I injuries, the symphysis is separated by less than 2 cm (Fig. 6.5A); in grade II injuries the sacrospinous and sacrotuberous ligaments rupture (Fig. 6.5B); and in grade III injuries the iliolumbar ligament can rupture (Fig. 6.5C). This type of pelvic fracture has double the mortality rate of the lateral compression injuries.
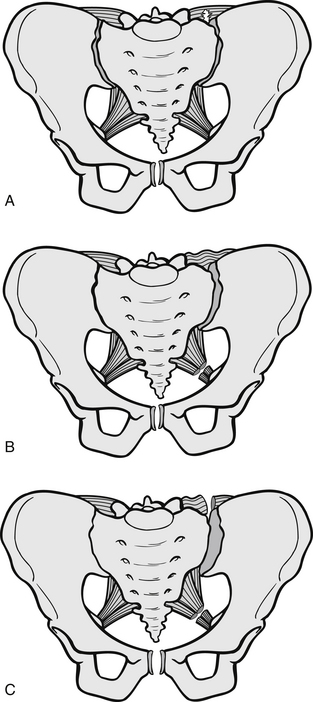
Figure 6.5 Anteroposterior compression fractures of the pelvis. (A) Grade I, (B) grade II, (C) grade III.
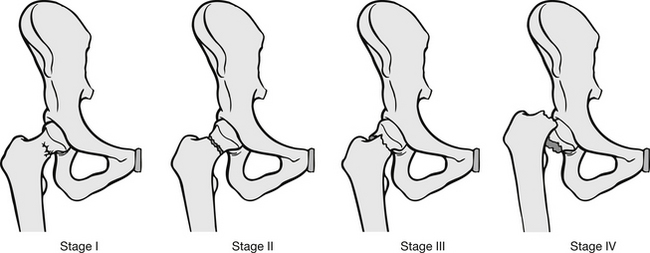
Vertical shearing force fractures result from falls or from knees hitting a car dashboard with great speed. The pattern of injury is similar to anteroposterior compression, but with vertical displacement (Fig. 6.6). With combined mechanical forces, such as being run over by a motor vehicle, a combination of the above fracture patterns may occur simultaneously.
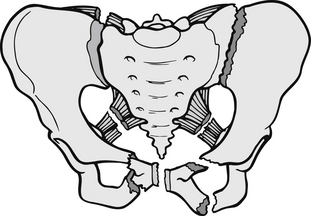
Figure 6.6 Pelvic ring fracture.
Patterns of single fracture injury to the pelvis include:
• acetabulum – these are not common in isolation, but can occur with direct force to the leg, driving the head of the femur into the acetabulum
• sacrum – again these are uncommon in isolation, but can result from a backward fall or falls from a height
• coccyx – this is often fractured by falls onto the buttocks, particularly in women where the coccyx is more prominent
• single pubic ramus – these appear to be common in elderly patients following falls; however, evidence suggests that they usually occur with other pelvic injuries that are not initially detected
• avulsion fractures – these occur in young athletes, where excessive muscle strain can avulse growth cartilage on the apophyseal plates
• iliac wing fractures – these injuries commonly result from direct trauma and should always be considered in conjunction with intra-abdominal injury.
Assessment of pelvic ring injury
Fractures involving the pelvic ring carry potentially life-threatening complications if not rapidly identified and treated. Because of the force exerted to cause such fractures, attendant injury to underlying organs and haemorrhage is common and associated with high morbidity and mortality rates. Injuries can include among others: neurological, 26 %; rectal/gastrointestinal tract, 7 %; renal, 7 %; and bladder, 10 % (Scalea & Burgess 2004); urethral, up to 24 % (Ingram et al. 2008); ureteral, 7 % (penetrating trauma) to 18 % (blunt trauma) (Lynch et al. 2005) as well as genitalia; haematuria and haemodynamic instability due to hypovolaemic shock (Routt et al. 2002).
Mechanisms of injury should give some clues as to a potential pelvic fracture. The assessing nurse should carry out a primary assessment following the ABCDE approach laid out in Advanced Trauma Life Support (ATLS) guidelines (American College of Surgeons 2008). A patient with a pelvic ring fracture will have severe pelvic pain and progressive flank, perianal or scrotal swelling and bruising. Disruption of the pelvic ring can also be identified by differences in leg length and external rotation of a leg without an associated limb fracture.
Mechanical instability of the pelvis can be tested by manual manipulation or compression of the pelvis. This should be carried out only once by an experienced clinician and only when X-rays have excluded unstable pelvic fractures. It is a very painful procedure for the patient and undue force carries the risk of exacerbating haemorrhage. When the clinician manipulates the pelvis, pressure should be applied gently to the iliac crest. If the pelvis has rotated, the clinician will be able to close the ring by gently pushing the iliac crests together. Most patients with a pelvic ring fracture will have moderate to severe hypotension.
Assessment should also include examination of the groin, perineal area and genitalia. Femoral pulses should be checked on both sides. Absent pulses are indicative of damage to the external iliac artery and emergency surgery is required to preserve the limb of the affected side. Decreased pulse pressure should be closely monitored, as it may be indicative of a worsening systemic condition or damage to the iliac artery. The perineum should be inspected for laceration and bleeding. Prophylactic antibiotics should be prescribed for wounds because of the high infection risk from faecal flora (Ruiz 1995).
Management of pelvic ring fractures
Pelvic fracture can be a life-threatening injury often accompanied by significant haemorrhage and injury to the genitourinary system (Hauschild et al. 2008). Arterial injuries occur in 20 % of patients and posterior fractures are more likely than anterior fractures to cause bleeding. Initial management focuses on volume replacement, stabilization of fractures and, therefore, the rate of haemorrhage and pain control. Fluid replacement should follow ATLS guidelines with a rapid infusion of warmed crystalloid fluid, ideally Ringer’s lactate or Hartmann’s solution (American College of Surgeons 2008). Ringer’s solution closely resembles the electrolyte content of plasma and therefore provides transient intravascular expansion followed by interstitial and intracellular replacement. Normal saline can be used, but large amounts are not recommended because it can induce hypercholaemic acidosis. After an initial 2 L, or 20 mL/kg in children, blood or colloid solutions should be commenced. The patient’s haemodynamic condition should be continuously monitored during this period.
Haemorrhage control relies on fracture stabilization. Early external fixation provides definitive haemorrhage control. As an interim measure, longitudinal skin traction can be used (American College of Surgeons 2008). The use of a pneumatic anti-shock garment (PASG) also known as military anti-shock trousers (MAST) serves a dual purpose of haemorrhage and pain control. It provides mechanical stabilization of the fractures and external counter-pressure. When used, circulation to extremities should be regularly checked as compartment syndrome is a known risk. Decompression should take place in a controlled environment, at a pace that does not exacerbate haemodynamic instability, generally in the operating theatre. The use of PASG in no longer emphasized in ATLS as Dickinson & Roberts (2004) found that there was no benefit from their use, while Mattox et al. (1989) demonstrated PASG increased morbidity and mortality. Pain control is initiated by fracture immobilization with intravenous opiates; inhaled analgesia, such as entonox in the conscious patient may be used where not contraindicated by other potential injuries.
Uncomplicated, isolated pelvic fractures not involving the pelvic ring should be assessed in a similar manner. The management of these injuries is usually conservative. Patients usually require hospital admission for initial bed rest, pain control and rehabilitation support. Most of these fracture injuries have an uncomplicated recovery pattern. Acetabular fractures, however, have a high morbidity rate. They are caused by extreme force, commonly road traffic accidents (RTAs), where the knees hit the dashboard at speed. Long-term prognosis is improved by surgical intervention (Snyder 2002).
Hip injury
Classification of fractures
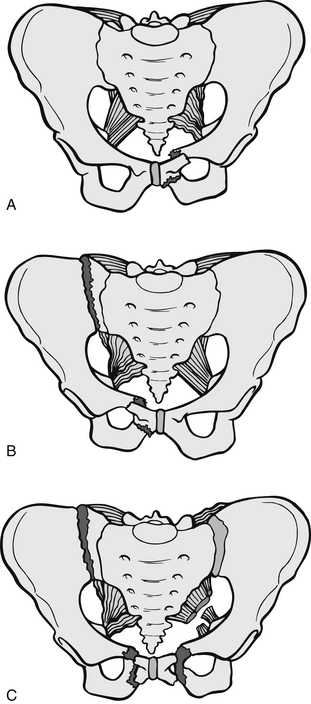
Garden’s classification of neck of femur (NOF) fractures has been used for almost 50 years (Garden 1964). He highlighted four stages of fracture (Fig. 6.7):
• Stage I represents impacted fractures. The trabeculae and cortex are pushed into the femoral head. This is considered a stable fracture as the inferior cortex usually remains intact. This type of fracture is not very susceptible to avascular necrosis and therefore operative treatment usually entails pinning rather than prosthetic replacement of the femoral head. Union rates are good and morbidity is low following this treatment (Ruiz 1995).
• Stage II is a non-displaced fracture across the entire femoral neck. Because there is no impaction, the fracture is unstable, but as there is no displacement the risk of avascular necrosis is low. These injuries are therefore fixed with screws.
• Stage III is a displaced fracture, with the femoral head abducted in relation to the pelvis. Fragments of the fracture are in contact with each other. Disruption of the blood supply is common and for this reason operative repair usually involves the insertion of a prosthesis to replace the femoral head.
• Stage IV are similar to stage III fractures in that they are displaced, but the femoral head is adducted in relation to the pelvis, fracture fragments are completely separated and avascular necrosis is likely. In most cases, prosthetic replacement of the femoral head is the treatment of choice in younger patients; however, attempts may be made to reduce and internally fixate the fracture. This prevents degeneration of the acetabulum caused over time by a prosthesis.
Intertrochanteric fractures
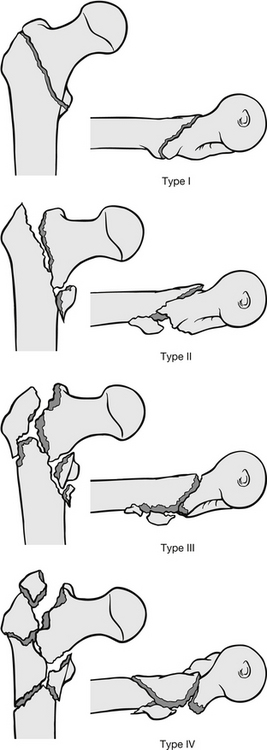
Several fracture classifications are used and all have slight variations from each other. To provide a general idea of fracture classification, Kyle et al. (1979) described four types of injury (Fig. 6.8):
• Type I – stable, undisplaced intertrochanteric fracture, requiring simple internal fixation.
• Type II – stable but displaced with fragmentation of the lesser trochanter; these are internally fixed.
• Type III – unstable fractures of the greater trochanter with posteromedial comminuted bone and deformity. These are fixed, but if a stable reduction cannot be achieved because of the amount of comminuted bone, osteotomy to the base of greater trochanter may be performed.
• Type IV – these have the components of type III fractures, but also have subtrochanteric fractures. Internal fixation is attempted using screws and sliding plates.
In children, NOF or intertrochanteric fractures are uncommon and are caused by severe force. Internal fixation is not the treatment of choice because of growth patterns. Children are treated with bed rest and traction.
Assessment of patients with hip injury
These patients are usually elderly, predominantly women, and commonly attend the ED following a fall. The average age of a person with a hip fracture is 84 years for men and 83 years for women; 76 % of fractures occur in women. Mortality is high; about 10 % of people with a hip fracture die within one month of injury and one-third within 12 months (National Clinical Guideline Centre 2011).
The patient usually complains of groin pain and pain through the thigh to the knee. Pain is worsened by any movement and the majority of patients will have been unable to weight-bear since injury. In most NOF and intertrochanteric fractures, the injured limb will be externally rotated and is shortened if displacement exists at the fracture site. Neurovascular integrity should be checked distally to the fracture, although damage of this type is extremely uncommon. The patient’s haemodynamic status should be regularly observed, particularly with intertrochanteric fractures where blood loss from surrounding tissues is higher than NOF fractures. The patient’s general health should be discussed and pre-existing medical conditions and medication established. It is also necessary to establish the cause of the fall to rule out medical reasons. The patient’s hydration and nutritional status should be assessed, as should skin integrity and risk level for pressure sores (Lisk et al. 2011).
Initial management
In most instances, these fractures can be broadly diagnosed clinically. X-rays provide supplementary information necessary for ongoing management. As a result, patients with clinically diagnosed fractures should receive appropriate analgesia, such as morphine sulphate, prior to X-ray. Hydration at an early stage reduces mortality, and therefore intravenous fluids should be commenced, particularly for patients with intertrochanteric fractures where blood loss is greater. Regular observations should be undertaken to ensure haemodynamic stability is maintained, and to ensure the patient is neither dehydrated nor becomes overloaded by fluid replacements. Early oxygen therapy has been demonstrated to be beneficial as hypoxaemia is evident in elderly patients with a fractured NOF. Most hospitals now have fast-track policies to get patients into a ward bed and off hard emergency trolleys (Audit Commission 2000). If tissue viability is to be maintained, this together with regular pressure area care is vital (Wickham 1997). If the patient’s general condition prohibits internal repair of the fracture, skin traction is advised at the earliest opportunity.
Limb injury
Classification of fractures
A break or fracture of the bone occurs when it is no longer able to absorb the mechanical energy placed on it. This usually results from trauma (Bickley & Szilagyi 2008). Fractures are classified into the following groups (Fig. 6.9):
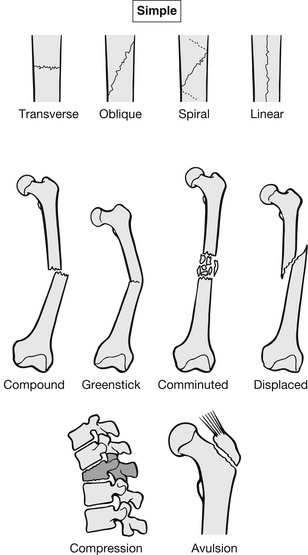
Figure 6.9 Fracture classification.
• simple – this is deemed a closed fracture because the skin is intact and the fracture is undisplaced. These can be further categorized by the direction in which the fracture travels:
 – oblique: at an angle to the length of the bone
– oblique: at an angle to the length of the bone
• compound – this is an open fracture where the skin has been punctured either internally by the bone or externally from the surface the skin came in contact with during the trauma. These can exist with any of the above types of fracture. It is also possible for fracture fragments to puncture blood vessels, nerves and organs. All compound fractures warrant prophylactic antibiotics and tetanus prophylaxis if not covered (Clasper & Ramasamy 2011)
• greenstick – these occur in children and are incomplete fractures, they are like a bent twig that disrupts the bone cortex but does not pass right through
• comminuted – fragmented fracture with two or more pieces
• displaced – bone ends are completely separated at the fracture site
• compression – adjacent bones are compacted
• avulsion – bone ends or condyles pulled off when the ligaments remain intact under extreme force.
Fracture healing follows a specific pattern. It has three main phases: inflammatory, reparative and remodelling.
The inflammatory phase lasts approximately 72 hours. Initially a homeostatic response to the physiological damage to bone, tissue and blood vessels occurs. A clot is formed in which the fibrin networks collect debris, blood and marrow cells. Capillary network increases over 24 hours and neutrophils invade the area. In the following 48 hours, phagocytosis takes place. In the reparative stage chondroblasts and osteoblasts proliferate. The chondroblasts unite fracture ends in a fibrous tissue called callus which begins to calcify after 14 days. During this phase osteoblasts create the trabeculae of cancellous bone while osteoclasts destroy dead bone. Remodelling takes several months: osteoblasts and osteoclasts restore bone shape, replacing cancellous with compact bone (Fig. 6.10).
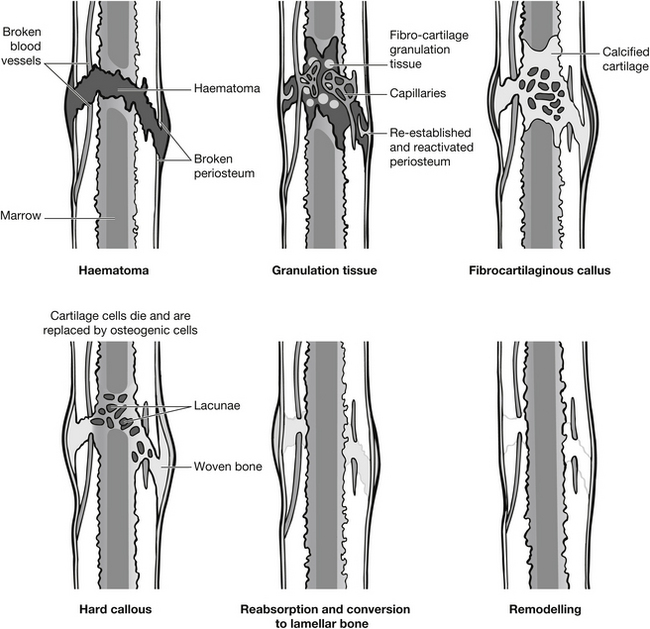
Figure 6.10 Bone healing process.
Assessment of limb injury
Following ATLS principles, assessment of extremity injury should take place after only the primary survey is completed and more serious injuries are dealt with. The assessment has three stages:
• identification and intervention in life-threatening haemorrhage (primary survey)
• identification and intervention in limb-threatening haemorrhage (secondary survey)
Assessment should follow a set pattern regardless of how severe or trivial an injury may appear. The assessing nurse should establish the history, perform an examination and, if appropriate, refer the patient for X-ray. When assessing the history, the nurse should establish a number of factors (Box 6.1). Mechanism of injury should include what happened, the direction and magnitude of force, and how long the patient was exposed to the force. When determining symptoms, the nurse should establish pain, loss of function and perceived swelling. The nurse should also enquire about the duration of symptoms and whether they are worsening or improving. Past history should include pre-existing injuries to that limb, medical conditions that affect the musculoskeletal system or bone density, and factors which would influence recovery.
Examination
Examination should follow a specific pattern, starting from the joint above, moving through the site of the injury, and finally checking neurovascular function distal to the injury. Principles of examination are shown in Box 6.2. Examination starts from the joint above the injury site to assess both function and limits of injury and to gain the patient’s cooperation and confidence. It should be systematic and considering of both the bony and soft tissue structures involved. The examination should also include assessment of pain, and factors influencing it, such as movement, pressure and guarding (Bickley & Szilagyi 2009).
If a patient presents with a mechanism of injury or the clinical examination is suggestive of a fracture then X-ray should be requested. X-rays should not, however, be performed for purely medico-legal reasons (Ward 1999).
Femoral fractures
The femur is the longest, strongest human bone. It is surrounded by muscles and is fed by the profunda femoris artery. The shaft of femur also has a good collateral blood supply in the periosteum. Most of the bleeding associated with femoral fracture is due to rupture of small branches of the profunda femoris artery. The femur only fractures under great force and the most common causes of injury are RTAs, particularly motorcycle accidents, pedestrian vs motor-vehicle accidents and falls (Nowotarski et al. 2000); particularly where bone density is compromised or the fall is from a significant height.
Assessment
Fractures of the femur fall into three anatomical categories: proximal, mid-shaft and distal. Examination findings are shown in Box 6.3. The patient should be carefully assessed for signs of hypovolaemic shock as blood loss from a closed shaft of femur fracture averages 1200 mL (Cadogan 2004). Although isolated femoral fractures rarely cause significant shock, fractures occurring with other traumatic injury do contribute to significant hypovolaemia. Observation should therefore be vigilant and X-ray will confirm diagnosis. Severe muscle spasms cause significant pain following femoral fracture and also cause the limb to shorten. Crepitus occurs over the fracture site as bone pieces move (O’Steen 2003).
Management priorities
Management priorities in the ED are twofold: preventing secondary damage and pain control. Preventing secondary damage includes managing blood loss by initiating intravenous fluid replacement. Reduction in blood loss and significant pain reduction can be achieved by correct application of an appropriate traction splint, such as a pneumatic Donway traction splint or a traditional Thomas half-ring splint or its modified version Hare traction splint may be used. These stabilize the fracture until definitive repair can take place. In doing this, the extent of the trauma to surrounding soft tissue is minimized. Pain is reduced because bone ends are immobilized. Distal and proximal pulses, capillary refill and sensation should be rechecked after splint application. If the fracture is open, broad-spectrum antibiotics should be given and the patient’s tetanus status checked. The wound should be covered with a damp dressing; care should be taken to avoid wound maceration if a delay to surgery is possible. Povidone-iodine soaks are commonly used because of the devastating effects of infection (see also Chapter 24). Intravenous analgesia should also be given. Fractured femurs take about 8–16 weeks to heal in an adult and 6–12 weeks in a child. Definitive treatment is usually internal fixation for an adult, which means they can usually be walking within two weeks post-surgery. Surgery is not recommended for children because of growth and speed of repair; therefore traction is recommended for older children, and plastering with hip spica for toddlers and small children.
Supracondylar fractures of the femur are assessed in the same way as shaft fractures. The mechanisms of injury are similar, with pain usually localized to the knee. Fractures involving the femoral condyles usually involve the knee joint and there may be associated knee joint injuries, particularly osteochondral fractures of the patella (Rowley & Dent 1997). These fractures do not cause the same extent of blood loss as shaft fractures and are repaired by either long leg casting or surgery.
Lower leg injury
Patellar fractures and dislocations
Patellar dislocation results from a direct blow to the medial aspect of the knee, common in football or similar contact sports. The knee locks and remains in a flexed position. On examination, obvious lateral deformity is present with medial tenderness and pain on attempted movement. Acute swelling between 2 and 12 hours of injury is likely to indicate haemarthrosis (Rourke 2003, Adams 2004). Treatment seeks to relocate the patella. This is usually straightforward and achieved by extension of the knee. It is painful because of muscle spasm and therefore analgesia and muscle relaxants should be used. A supportive long leg bandage should then be applied, or a long leg cast.
Tibial plateau fractures
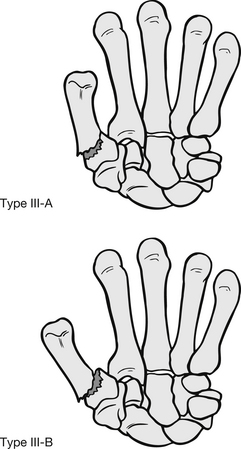
Tibial plateau injury commonly occurs from pedestrian/car accidents, usually at lower speeds where the car bumper hits the standing pedestrian. Fractures also occur as a result of a fall from a height, causing compression of the plateau, or they may occur in elderly patients with osteoporotic bones. Patients usually present with pain and swelling over the fracture site and inability to weight-bear. Swelling varies considerably, with haemarthrosis sometimes present. Diagnosis of tibial plateau fractures is usually by X-ray and is classified using the Schatzker classification system (Schatzker et al. 1979) which records six levels of injury:
• I: split lateral condyle without displacement
• II: split fragmented lateral condyle with depression of the fragment
• III: compression of the lateral (IIIA) or central (IIIB) condyle with depressed displacement
• VI: bicondylar with complete dissociation of metaphysis from diaphysis – extending into the tibial shaft.
Choice of treatment is dictated by the classification of the injury, displacement of fragments, and the condition of skin, tissue and muscles. Conservative treatment includes long leg plaster casting, traction and functional cast bracing and is reserved for classes I–IV where surgery is not otherwise indicated. Internal fixation is more common because of the morbidity risk of prolonged immobilization, particularly in older patients (Harris & Haller 1995).
Tibial shaft fractures
Mechanisms of injury are varied. The tibia has little muscular protection, so fractures from direct blows are the commonest long bone fracture. They are also the most common open fracture. As the tibia is vulnerable to torsional injuries, for example in sporting injuries, and force transmitted through the feet is high, the incidence of injury is high (Smith 2005), particularly in children. Similar mechanisms cause tibial and fibular fracture, although much more force is needed to break both bones. Direct trauma tends to cause transverse or comminuted fractures, and indirect trauma causes oblique and spiral fractures. The patient presents with localized pain and is usually unable to weight-bear. Surrounding soft tissue damage varies from a haematoma, causing swelling, to an open wound caused by fracture ends. Treatment for tibial fractures varies: children with greenstick fractures need casting for 6 weeks; in adults, displaced fractures may need internal fixation. ED documentation of the neurovascular status is vital as the risk of compartment syndrome is high. Therefore admission for 24 hours, observation and limb elevation should be considered in very swollen proximal tibial fractures. Pain is managed with intravenous opiates and the lower leg should be plastered as soon as possible. Circumferential casts must never be applied in the acute phase because of the inherent risk of compartment syndrome.
Tibial and fibular fractures
Combined tibial and fibular fractures are fairly common in contact sports, such as football. In injuries where indirect force causes the fracture, the tibia and fibula may be fractured in different places. Commonly, the tibial shaft fractures at the distal third, and because of a twisting mechanism the fibula fractures at the proximal end. This reinforces the need to assess from the joint above to the joint below the injury. If injury is caused by direct force and both bones are fractured at the same level, the leg will appear unstable and flexible at the fracture site. It is important that temporary immobilization occurs as soon as possible, both to reduce pain and to prevent further soft tissue damage. These fractures will need surgical fixation (Gordon et al. 2012).
Ankle fractures
Most ankle injuries seen in the ED are soft-tissue injuries (Eisenhart et al. 2003). Patients with fractures risk significant morbidity if these are not identified and treated early. The ankle is a complex hinge joint made up of three bones: the tibia, fibula and talus, and three collateral ligaments: the lateral, medial and interosseous. These ligaments stabilize the ankle joint; the lateral ligament allows for some inversion of the joint, whereas the medial and interosseous have less stretch (Fig. 6.11). Injury patterns can be classified by the mechanism of injury (Box 6.4 and Fig. 6.12).
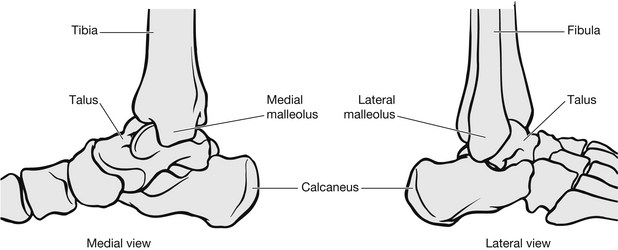
Figure 6.11 Bony anatomy of the ankle.
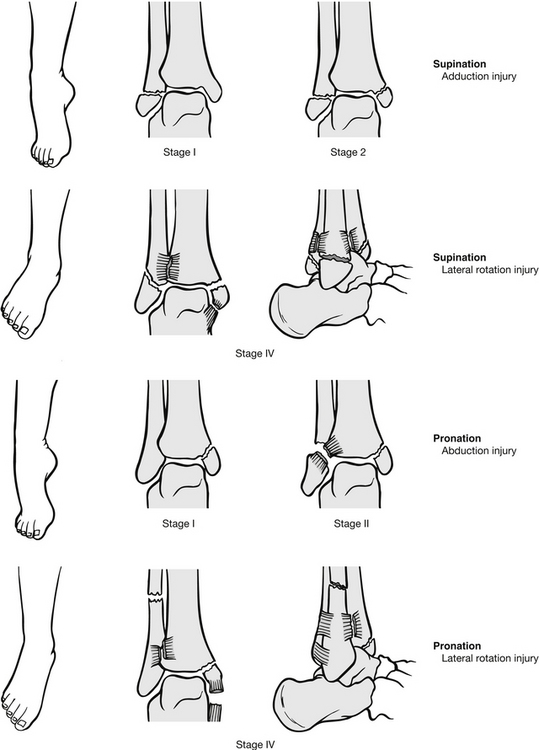
Figure 6.12 Ankle fracture (based on Lauge-Hansen classification). (After Mayeda DV (2009) Ankle and foot. In: Marx J, Hockberger R, Walls R, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice, 7th edn. St Louis: Mosby Year Book.)
Isolated lateral malleolar fractures can occur following inversion injury. Patients present with pain, swelling, ecchymosis and bony tenderness on the lateral aspect of the ankle and are usually unable to weight-bear (Hopkins 2010). Most isolated fractures are either a chip or avulsion fracture with ligament injury. These can be treated by a below-knee weight-bearing cast. Some fractures above the joint line or comminuted fractures may warrant surgical intervention. Isolated medial malleolar fractures are less common and usually result from a direct blow or eversion and, occasionally, inversion injury. The patient presents with pain over the medial aspect, swelling and limited range of movement. Usually, the patient will be non-weight-bearing (Wyatt et al. 1999). Simple avulsion fractures can be managed by below-knee casting. Fractures into the joint space should be referred for specialist opinion as internal fixation may be necessary.
Bi-malleolar fractures involve two of the lateral, medial and posterior malleoli, usually the lateral and medial. The patient presents with a history of inversion or eversion injury and will have bilateral bony tenderness and swelling, with or without deformity, and will be non-weight-bearing. These are unstable fractures with a significant risk of ankle dislocation. The ankle should be temporarily immobilized, adequate pain relief should be given and hospital admission facilitated. Restoration of function requires accurate medial malleolus reduction and joint space alignment (Mayeda 2009). Good outcomes are also dependent on skilled plastering and surveillance for weeks. Increasingly surgeons prefer to avoid these uncertainties by routine accurate internal fixation (McRae 2006). Lateral malleolar reduction is desirable but less crucial. This is usually achieved by open reduction and fixation in theatre, but can be achieved by closed methods if surgery is contraindicated.
The standard X-ray evaluation for the acutely injured ankle includes lateral, anteroposterior and mortice views. The requirement for X-ray of the adult ankle or foot may be determined using the Ottawa Ankle Rules (Stiell et al. 1992). These have shown that X-rays are only required for the ankle if there is any pain in the malleolar region and:
• bone tenderness over the posterior aspect of the distal 6 cm of the lateral malleolus or
• bone tenderness over the posterior aspect of the distal 6 cm of the medial malleolus or
• inability to weight-bear for at least four steps both immediately after the injury and at the time of assessment in ED.
Foot X-ray is required if there is pain in the midfoot region and:
• bone tenderness at the navicular or
• bone tenderness at the base of the fifth metatarsal or
• inability to weight-bear for at least four steps both immediately after the injury and at the time of assessment in ED.
The Ottawa ankle rules (Fig. 6.13) apply to adults (>18 years) and have a >98 % sensitivity for detecting clinically significant malleolar ankle injuries. They also reduce the number of ankle X-rays by up to 40 % (Bachmann et al. 2003).
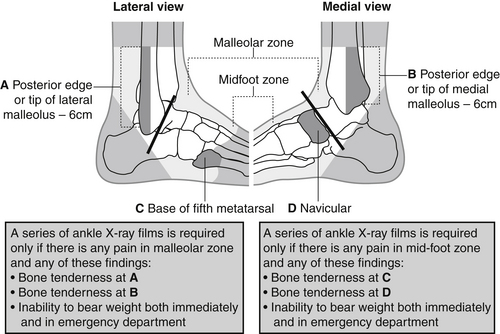
Figure 6.13 Ottawa ankle rules assessment.
Ankle dislocation
Dislocation occurs in one of four directions: anterior, lateral, superior and posterior. Posterior is the most common (Fig. 6.14). Stability of the ankle is normally maintained by tight articulation of the talus with the tibia and fibula. Isolated ankle dislocation is extremely rare (Georgilas & Mouzopoulos 2008) and may well be due to the amount of force required. It is usually associated with malleolar fractures and ligament rupture. Common causes of dislocation are sports injuries, direct force or RTAs (Harris 1995). Complicated dislocations associated with multiple ankle fractures are most common in osteoporotic women.
On examination the ankle will be oedematous, the joint locked, with the distal tibia prominent under stretched skin. Management priorities in the ED are to preserve neurovascular integrity. Early reduction is crucial, since delay may increase risk of neurovascular compromise or damage to articular cartilage. If there appears to be neurovascular compromise, the ankle dislocation should be reduced urgently, without waiting for X-rays. If neurovascular integrity appears intact, X-rays can be obtained, but the foot should remain supported to prevent further injury. Reduction should be carried out swiftly after X-ray. Nitrous oxide is a useful initial pain relief, for its therapeutic effects of analgesia, increasing oxygen intake and for its distraction potential, i.e., by getting the patient to concentrate on breathing (Bowie 2011). While the dislocation is being reduced, the patient should have adequate intravenous analgesia and muscle relaxant. The patient’s cardiac and respiratory function should be monitored during this procedure.
Foot fractures
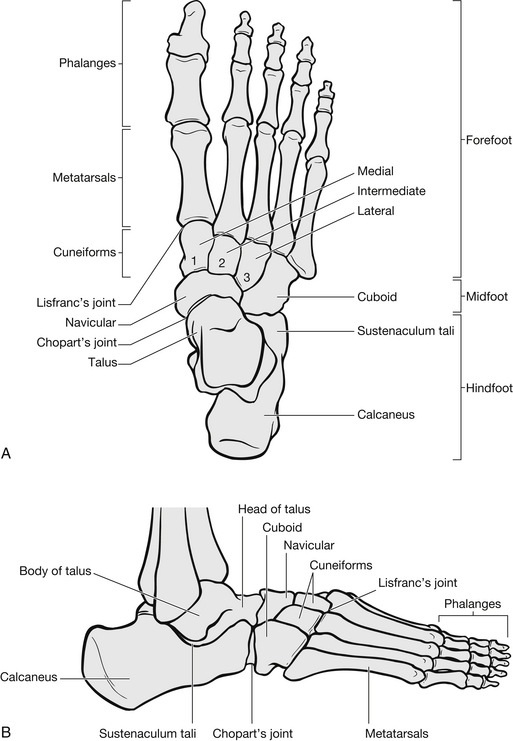
The foot has 28 bones with 57 articulating surfaces and is divided into three anatomical areas (Fig. 6.15). It is considered vital for balance, movement and as a shock absorber for movement.
The hindfoot
The talus supports the body weight and forces above by allowing movement at the ankle joint and between the calcaneus and midfoot. It is well secured by ligaments surrounding the ankle joint and therefore fracture is uncommon (Harris 1995). In the event of injury to the talus, the risk of complication is high because 60 % of the surface is covered by articular cartilage and vascular supply is low, creating a significant threat of avascular necrosis. It is usually injured as a result of falls, landing on the heel or forefoot, causing fractures through the body or neck of the talus. Fractures to the neck of the talus also result from head-on RTAs, where the driver’s foot is pressed against compressed floors or pedals, causing extreme dorsiflexion.
The calcaneus
The patient presents with pain over the rear of the foot and both sides of the heel. Swelling is usually present and patients are usually unable to weight-bear on their heel. If the presentation to ED is a few hours post-injury, a horseshoe-shaped bruise may be present. Calcaneal fractures are categorized into two groups: those involving the subtalar joint and those which do not, i.e., extra-articular fractures. The outcome for patients with extra-articular fractures is considerably better than those involving the subtalar joint. Extra-articular fractures are managed conservatively with compression and elevation in the first instance. After swelling has subsided, the injury is immobilized in a cast. The majority of fractures will involve the subtalar joint and the prognosis for these patients is poor. About 50 % have some long-term problems from the injury (Mayeda 2009), including restricted movement, pain and subtalar arthritis. Most are treated with internal fixation. Fractures to other bones of the foot are not uncommon, and patients with suspected calcaneum fractures, or those who have fallen over six feet, must have a full examination of the spine and lower leg (Larsen 2002).
The midfoot
This region includes the navicular, cuboid, cuneiform and metatarsal bones. The midfoot provides foot flexibility. Fractures to this area are uncommon and result from direct force, such as crush injuries. Transverse dislocation of the forefoot results from direct force. Patients present with localized tenderness and swelling. These injuries heal well and can usually be treated with below-knee non-weight-bearing casts. There are two exceptions to this: the first relates to avulsion fractures of the navicular, which occur as a result of eversion injury. If 20 % or more of the articular surface is avulsed, the fracture should be internally fixed, if less than 20 % is avulsed, a below-knee cast should be adequate. The second exception is the Lisfranc dislocation, which occurs when the forefoot is dislocated across the metatarsal joints. This is an extremely rare condition, occurring in one in 55 000 cases (Mayeda 2009). Neurovascular compromise is common, partly because the force necessary to cause dislocation also causes extensive soft tissue damage, resulting in oedema and vascular compromise. The patient presents with moderate to severe midfoot pain and large amounts of swelling which can hinder diagnosis. There is usually a shortening of the foot length, compared with the uninjured foot, and the injured foot will have transverse broadening.
The forefoot
The forefoot consists of the five metatarsal bones and the phalanges.
Metatarsal fractures
Fifth metatarsal fracture, also known as a Jones fracture is one of the most common foot injuries (Herrera-Soto et al. 2007). It usually results from an inversion injury causing sudden contraction of the peroneus brevis muscle. The tendons joining this muscle with the base of the fifth metatarsal can cause an avulsion fracture. The management of fifth metatarsal fractures is either neighbour (or buddy) strapping and crutches or a below-knee cast, depending on the patient’s pain. Occasionally, displaced fractures require internal fixation.
Phalangeal fractures
These result from stubbing injury or from dropping heavy objects on toes. The patient presents with pain, swelling and often bruising or a subungal haematoma. The clinical symptoms can make fracture diagnosis difficult and often X-rays do not offer much assistance (Mayeda 2009). If angulation or deformity of the toe exists, then X-rays are more helpful. Most fractures can be managed by neighbour strapping and elevation. Obviously angulated fractures should be reduced using a digital block, then the toe neighbour strapped. Big toe fractures needing reduction may warrant immobilization in a cast with toe support.
Shoulder injury
The shoulder girdle consists of three bones: the scapula, the clavicle and the humerus (Fig. 6.16). The shoulder attaches the arms to the axial skeleton. These are interconnected at the acromioclavicular, glenohumeral, coracoclavicular and sternoclavicular articulations and muscles from the rib cage and cervical spine. The glenohumeral joint (GHJ) is where the head of the humerus articulates with the glenoid fossa of the scapula providing the majority of the shoulder girdle movement. The sternoclavicular joint (SCJ) links the arm to the axial skeleton, via the clavicles, the upper and lateral manubrium sterni and the cartilage of the first rib. The SCJ deltoid, pectorals and trapezius muscles maintain the normal position of the shoulder. The acromioclavicular joint (ACJ) permits the ‘gliding’ motion of the articular end of the lateral clavicle on the medial aspect of the anterior acromion and rotation of the scapula on the clavicle during abduction of the arm (Knapton 1999). The clavicle is attached to the scapula by acromioclavicular and coracoclavicular ligaments, the latter incorporating both the conoid and trapezoid ligaments and is the stronger of the two. If any of the ligaments weaken or tear, the shoulder has a greater tendency to dislocate.
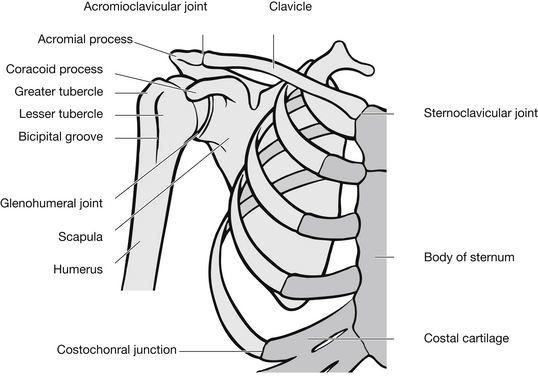
Figure 6.16 The shoulder girdle.
Scapular fractures
The scapula is situated above and lateral to the posterior thorax. It is well protected from injury by thick muscle and extreme force is necessary to fracture it. Injuries commonly result from high-speed road traffic accidents, crushing or falls. Occasionally, a scapular fracture occurs as a result of electric shock, when one or both scapulae are fractured (Rana & Banerjee 2006). Fractured scapulae most frequently occur in young men (O’Steen 2003) because of the force needed to cause fractures and associated injuries such as pneumothorax, chest wall injury or related shoulder girdle injuries.
Anatomically, scapular fractures fall into three categories (Fig. 6.17):
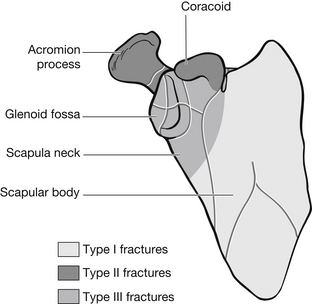
Figure 6.17 Classification of scapular fractures.
• Type I fractures are difficult to palpate because of thick muscle and pain. An adducted shoulder and the mechanism of injury should suggest possible fracture, which can be confirmed on X-ray (Knapton 1999). Treatment is usually conservative and involves pain relief and simple immobilization using a broad arm sling on the injured side. Controversy exists over the benefits versus risks of plating scapular body fractures. It has been suggested that scapular fractures have a better outcome when treated operatively (Cole 2002) despite reluctance by clinicians after historically choosing conservative therapy because of high post-operative complication rates as argued by Schmidt et al. (1992).
• Type II fractures involve the acromion and coracoid process. They occur from direct trauma and are similar in that patients have pain over the site of injury and adduction of the shoulder. They differ in that acromion fractures cause pain on elbow flexing, while in coracoid fractures the patient actively flexes the elbow as a form of pain relief. Both types are usually managed conservatively unless concurrent shoulder girdle injury exists, such as dislocation or clavicular fracture.
• Type III fractures involve the scapula neck or glenoid fossa. They result from lateral to medial rotation of the humeral head. The patient presents with pain around the humeral head and on shoulder adduction, and is usually supporting an injured arm. Treatment involves immobilization of the arm on the injured side; however, difficulty in regaining full range of movement following this injury is high.
Clavicular fractures
The clavicle provides anterior support for the shoulder. It is a slightly S-shaped bone that articulates laterally with the acromion process and medially with the sternum. The clavicle gives definition to body shape as well as providing protection for the subclavian neurovascular bundle. Clavicle fractures make up 5 % of all fractures, so are not uncommon and in children and adolescents it is a particularly common fracture (O’Steen 2003). Fracture of the clavicle is most commonly due to a violent upwards and backwards force such as a fall on the outstretched hand. Less commonly, the clavicle may be fractured by blows or falls on the point of the shoulder.
Clavicular fractures are divided into three groups: proximal third fracture, mid-clavicular fracture and distal fractures (Table 6.2).
Table 6.2
Classification of clavicular fractures
| Type | Mechanism of injury | Frequency (% of all clavicular fractures) |
| Proximal third | Direct blow to anterior chest | 5 |
| Mid-third | Indirect force to lateral aspect of shoulder | 80 |
| Distal third | Direct blow to top of shoulder | 15 |
Common presenting symptoms include pain over the fracture site, crepitus and sometimes a palpable deformity. The patient is usually supporting the arm of the injured side. In mid-clavicular fractures, deformity is common. The patient presents with a downward shoulder stump, sometimes rotated inward and forward. This is due to gravitational forces and contraction of the pectoralis major. The proximal fragment is displaced upward. Because of the location of the neurovascular bundles and the great blood vessels, a careful assessment of neurovascular function of the arm on the injured side must be carried out. Management of clavicular fracture is usually conservative. Immobilization with a simple sling is as effective as other less comfortable methods and is therefore the treatment of choice. Displaced fractures of the distal third often require surgical repair because of the risk of non-union. Complications frequently include malunion, regardless of the support mechanism used. While malunion is of little functional or cosmetic consequence, a persistent sharp clavicular spike may cause discomfort against clothes and require excision (Kelly 2004). Patients should be advised that a residual palpable or visible deformity may be present after healing has occurred (Smith 2005).
Shoulder dislocation
The glenohumeral joint of the shoulder girdle is a shallow synovial ball and socket joint that comprises five joints and three bones. The wide range of movement carried out at the shoulder, and its lack of bony stability, predisposes the joint to dislocation. Two main patient groups can be identified: men between the ages of 20 and 30 years (Zacchilli & Owens 2010), and women over 60 years, and approximately 55–60 % of shoulder dislocations are recurrent (Proehl 2009). Glenohumeral joint dislocation can be categorized into four groups: anterior (>90 % of dislocations), posterior (<5 %), inferior (<1 %) and superior (<1 %).
Anterior dislocation
The patient presents in extreme pain, usually holding the injured arm in abduction and external rotation (Genge Jagmin 1995). On examination, the shoulder will be obviously deformed when compared with the uninjured side. It will have a square appearance over the lateral aspect and the acromial process will be prominent (Fig. 6.18). Assessment should include a detailed examination of neurovascular function (Box 6.5).
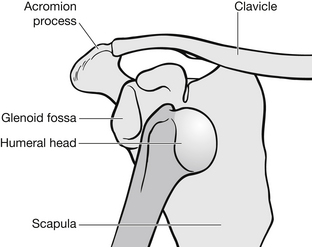
Figure 6.18 Anterior dislocation of the shoulder.
Before shoulder dislocation is treated, humeral fracture should be excluded on X-ray. Fractures of the humeral head or neck prohibit early reduction of dislocation in the ED and orthopaedic opinion should always be sought. If no fracture exists, reduction of shoulder dislocation should be carried out as soon as possible. Prompt reduction is always necessary as the procedure becomes more difficult as time passes and the dislocation may prove irreducible (Mills et al. 1995), partly because muscle spasm increases with the length of time the joint is dislocated. Early relocation is also vital in maintaining the integrity of the humeral head. Because the scapular neck is harder than the humeral head, a compression fracture occurs, causing long-term deformity to the humeral head (Hill-Sachs deformity), which leads to recurrent dislocation. This is thought to occur in between 11 and 50 % of patients with anterior dislocation.
Traction methods include laying the patient prone with the injured arm over the side of the trolley and hanging a 5–7 kg weight, depending on the patient’s muscularity, on the affected arm. Over 20–30 minutes this reduces muscle spasm by gently elongating muscles, pulling the humeral head off the scapular and allowing the rotator cuff muscles to relocate it in the glenoid fossa. This method is thought to be less painful than some more aggressive relocations and the risk of complication is low (Quaday 1995). There are several approaches to reduction available: two-person traction/counter-traction using a sheet, two-person traction/counter-traction using foot in the patient’s armpit, external rotation leverage, Kocher’s leverage technique and Spaso Miljesic leverage method.
The most commonly used and safest traction method of reduction is a two-person traction/counter-traction approach. One person applies longitudinal traction to the injured arm, reducing muscle spasm, while the other person applies counter-traction by wrapping a sheet around the patient’s chest and under the axilla of the injured side and then pulling towards the patient’s ear on the unaffected side. This helps to disengage the humeral head from the scapula. Traditional traction/counter-traction methods of putting a foot in the patient’s armpit and then pulling on the arm are not recommended because of their high association with neurovascular injury and lower success rate than other methods (Quaday 1995).
Leverage techniques involve some traction to lift the humeral head off the scapula, but then lever it back into place. These methods are fast, but increase the risk of injury to the glenoid rim or humeral shaft. The external rotation method of reduction is the least traumatic. It works by slowly adducting the injured arm and then flexing the elbow to 90°. The elbow is then held in place while the forearm is externally rotated by its own weight and gravity, not by force. This allows the smallest profile of the humeral head to be relocated into the glenoid fossa. The traditional method of leverage is Kocher’s technique. This involves a three-step external/internal rotation manoeuvre which is both painful for the patient and dangerous because of the high risk of vascular tearing, rotator cuff injury and humeral fracture. A third technique is the Spaso Miljesic method: with the patient supine grasp the arm around the wrist or distal forearm. Gradually lift the arm vertically, applying gentle traction. Slightly externally rotate while maintaining vertical traction. Pauses may be required when muscular spasm occurs in which case the traction is maintained while movement is halted until the spasm passes (Yuen et al. 2001). If reduction cannot be achieved, orthopaedic referral should be made for manipulation under general anaesthetic.
Whatever method of reduction is used, it is important that neurovascular integrity is rechecked, and an X-ray taken to check position. The affected arm is often immobilized to prevent re-dislocation, however Hovelius et al. (2008) found that there were no long-term differences between patients who were immobilized compared with those who were allowed immediate mobilization. Where immobilization is chosen, the arm should be adducted and internally rotated. To prevent shoulder stiffness, the patient should be advised to extend the elbow and rotate the arm to a neutral position several times a day. In older patients, the risk of joint stiffness is greater, and therefore it is usual to remobilize the arm sooner than in younger people. Patients over 40 years should not be immobilized for longer than three weeks. The rate of re-dislocation is higher in younger people but settles over time (Hovelius et al. 2008).
Posterior dislocation
The anatomy of the shoulder girdle makes posterior dislocation difficult because the glenoid fossa is positioned posteriorly to the humeral head. The angle of the scapula helps to buttress this structure. When dislocation occurs, the humeral head sits behind the glenoid and usually below the acromion (Fig. 6.19).
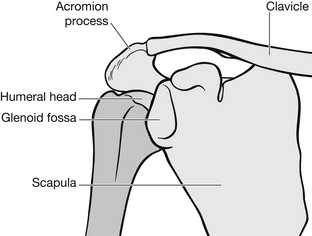
Figure 6.19 Posterior dislocation of the shoulder.
Posterior dislocation is caused by a fall onto an outstretched hand where the arm is flexed and internally rotated. Posterior dislocation also occurs following significant electric shock, epileptic seizures and, occasionally, from direct force to the anterior aspect of the shoulder. The patient will have severe pain and will present holding the arm in internal rotation, supported in a sling-type position. There is usually a loss of definition of the anterior shoulder and a prominent acromial and coracoid process, with the humeral head sometimes palpable posteriorly. The patient is unable to lift the arm above 90° and cannot externally rotate.
Diagnosis should be made from the mechanism of injury and patient presentation as anteroposterior X-rays are inconclusive and up to 50 % of posterior dislocations are missed initially (Quadray 1995). Lateral and axillary X-ray views will confirm diagnosis. Neurovascular injury is less common with posterior dislocation because the major structures lie anterior to the joint and are thus protected. Although closed reduction with muscle relaxant and analgesia may be attempted, orthopaedic consultation should determine this.
Upper arm injury
Humeral fractures are common in two main patient groups:
• women aged between 56 and 65 years, usually with osteoporosis – fractures occur as a result of a fall and occasionally direct force; injury is usually to the proximal humerus, neck or shaft
• young men aged between 16 and 24 years – mechanisms of injury include RTAs (transverse humeral fractures), falls from a significant height (oblique or spiral fractures) and stress fractures from throwing actions.
The patient will present holding their arm close to their chest, with localized pain, extensive bruising or shoulder pain in fractures of the humeral neck. The upper arm is usually swollen and may have obvious shortening with normal movement at the point of fracture. Very careful neurovascular assessment is necessary, especially with distal third fractures as both the brachial plexus and axillary nerve may be damaged. Circulation should be assessed at the brachial pulse, radial pulse and along the ulnar and brachial arteries. The axillary artery is the most common to sustain vessel injury and may be present with any combination of limb pain, paraesthesia, pallor, no pulse, a cool limb and paralysis. Capillary refill of the fingertips and hand should also be assessed. Sensory and motor function should be checked in line with radial, ulnar and median nerve activity.
• traction to restore length and align fragment
• any angulation should be reduced
• initial immobilization for pain control and healing
• encourage mobilization of shoulder and elbow to prevent loss of function.
A number of immobilization methods exist. Hanging casts and U-slabs have been used for many years as a method of immobilizing the upper arm. As well as being extremely uncomfortable and restrictive for patients, these casts can cause posterior angulation of the fracture (Ciernick et al. 1991); and since they are not adjustable they cannot ensure that the soft tissues are compressed as swelling decreases and atrophy ensues or enable the patient to move the arm several times a day to passively flex and extend the elbow, emphasizing extension of the joint. Slings are commonly used, but these offer little immobilization or pain control. The treatment of choice appears to be an interlocking upper arm functional brace with forearm support. These have 95 % excellent functional rotation and 85 % minimal shortening of the limb (Zagorski et al. 1988). Functional bracing is contraindicated in: fractures with axial distraction between the fragments due to higher risk of delayed or nonunion; open fractures with major soft-tissue damage or with vascular injuries that require surgical repair; bilateral humeral fractures; and polytrauma who are unable to walk are best treated by surgical stabilization. Open reduction with internal fixation is usually performed for open or severely comminuted fractures and in patients with multiple fractures where conservative management would delay overall recovery and mobility.
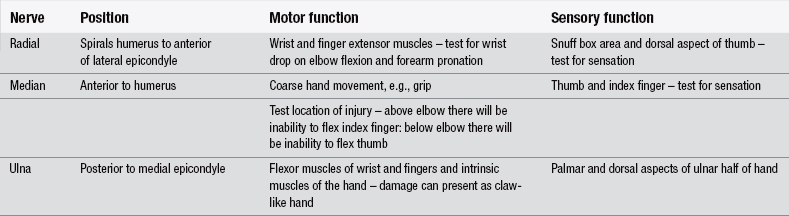
Elbow injury
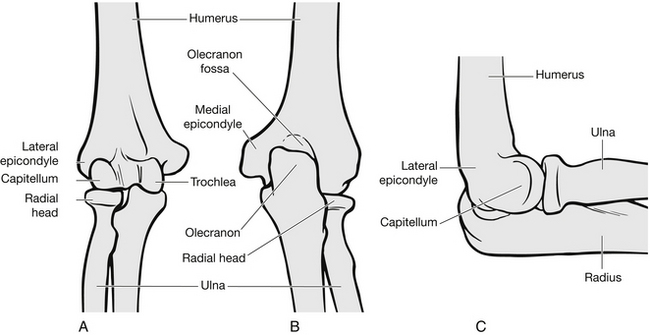
The elbow joint is a hinge-like articulation and consists of the distal humerus, radius, ulna and olecranon (Fig. 6.20). The distal humerus forms two columns; the lateral and medial epicondyles form the proximal part of these columns and are significant for their muscle attachment facilitating wrist movement. The wrist extensors originate from the lateral epicondyle, and flexors from the medial epicondyle. The trochlea articulates with the olecranon to allow flexion/extension at the elbow, and the capitellum allows pronation and supination of the forearm by articulation with the radial head. The radial nerve travels around the humerus to the anterior of the lateral epicondyle, and supplies the wrist and finger extensors. Because of its proximity to the distal humerus, it is very susceptible to injury. The medial nerve travels anterior to the humerus with the brachial artery. It provides sensation to the thumb and index finger and coarse hand movement, such as grip. If the nerve is damaged above the elbow, the index finger cannot be flexed (Ochsner’s test). If damaged in the forearm, the interphalangeal thumb joint cannot be flexed if the base of the thumb is held to immobilize it.
Supracondylar fractures
These are distal humerus fractures, proximal to the epicondyles. They are the most common fracture in children and adolescents, accounting for 50–70 % of elbow fractures (El-Adl et al. 2008) and 30 % of all limb fractures in under-7-year-olds (Babal et al. 2010). Supracondylar fractures are categorized into two groups depending on the mechanism of injury: extension and flexion fractures.
Extension fractures
This type of fracture is caused by a fall onto an outstretched hand with the elbow locked in extension (Fig. 6.21). This results in posterior displacement of the distal fragment of the humerus, and puts neurovascular structures at risk because of the jagged proximal humerus which becomes anteriorly angulated. This injury is most common in those under 15 years of age, because the tensile strength of the ligaments and joint capsule is greater than that of bone, and therefore fracture occurs. In adults, the reverse is true and dislocation of the elbow joint is more common (Magnusson 2009).
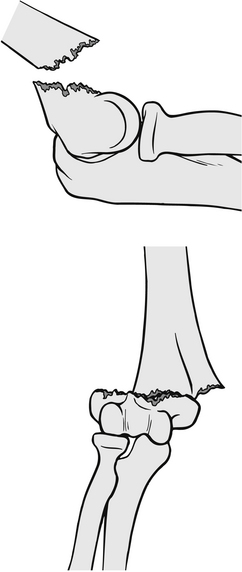
Figure 6.21 Supracondylar extension fracture.
The patient will present holding the arm partially flexed. There is usually severe pain and swelling above the elbow. A thorough assessment should be made of neurovascular and motor function, as injury to the radial nerve occurs in about 8 % of patients (Tsai & Ruiz 1995) (Table 6.3).
Management depends on clinical findings. If circulatory compromise exists then immediate reduction should be considered in the ED. This carries significant risk of neurovascular damage and should only be carried out in limb-threatening situations. In most cases prompt reduction of the fracture should be carried out in theatre. In undisplaced fractures, a plaster backslab can be applied, and provided neurovascular integrity is maintained the patient can be discharged with limb care advice and fracture clinic follow-up.
Flexion fractures
These are less common than extension fractures and comprise approximately 2–4 % of the total number of supracondylar fractures (Babal et al. 2010). They are caused by direct force to a flexed elbow, from a fall or a blow (Fig. 6.22). The patient will have significant pain around the site and will be supporting the injured arm in a flexed position, but the olecranon prominence will be decreased. There may be a prominent proximal fragment of the humerus anteriorly, and these injuries are commonly seen in open fractures. Although nerve damage is less likely with flexion fractures, the ulnar nerve is at risk because of fracture displacement. Vascular injury is uncommon. If only minimal displacement exists, the fracture can be treated by closed reduction and an above-elbow back-slab in flexion. Fractures with significant displacement or open injuries should have open reduction and internal fixation of the fracture.

Figure 6.22 Supracondylar flexion fracture.
Elbow dislocation
The patient will have pain, the arm will be supported in mid-flexion and the limb will appear shortened. The olecranon is prominent. Careful neurovascular examination is essential, especially of the nerve and brachial artery. The median nerve may be assessed by feeling the muscle while the patient attempts to resist the thumb being pressed from a vertical position against the plane of the hand (Smith 2005). The brachial artery can be assessed by checking the radial pulse.
Radial head fractures
In this type of fracture the radial head becomes compressed upwards against the capitellum following a fall onto an outstretched hand. It is an important feature in elbow flexion/extension and forearm rotation. The patient will present with localized pain, which is worse with passive rotation of the forearm and an inability to fully extend the forearm. The presence of a fat pad elevation on X-ray is recognized as associated with an underlying radial head fracture in recent trauma (O’Dwyer et al. 2004). For management purposes, fractures are classified into three types (Table 6.4).
Table 6.4
Classification and management of radial head fractures
| Type | Description | Management |
| I | Undisplaced | Sling with early mobilization |
| II | Marginal fracture with displacement | Joint aspiration if necessary Sling and early mobilization |
| III | Comminuted fracture | Treatment options vary from internal fixation to partial or total extension of the radial head |
Forearm injury
Ulnar fractures
Ulnar shaft fractures sometimes known as nightstick fractures are caused by direct force to the arm, commonly when it is raised to protect the face from injury. The patient presents with pain over the area, and swelling and deformity if the fracture is displaced. Management depends on the degree of displacement. Fractures with more than 50 % displacement or 10 % of angulation should be internally fixed as they carry a significant risk of non-union. Fractures with less displacement/angulation can be treated in a long arm POP cast with the elbow in 90° flexion and the forearm in a neutral position. Non-displaced fractures initially treated by immobilization respond well to early remobilization at about ten days post-injury.
Proximal ulnar fractures rarely occur independently and are associated with radial head dislocation. This is called a Monteggia fracture and four major classifications of these exist (Wilkins 2002), these are defined by the position of the radial head. Monteggia fractures have a better outcome in children compared with adults (Wilkins 2002). In adults, these fractures are associated with increased morbidity including the complications of reduced function, non-union, infection and the need for revisionary surgery (Fayaz & Jupiter 2010). Radial nerve paralysis can also occur as a result of compression from the displaced radial head. This causes weak wrist and hand extensors. It has been argued that the implications of distal ulnar fractures are often insufficiently appreciated and may result in ineffective treatment, especially compared to distal radius fractures (Logan & Lindau 2008). Greenstick fractures of the ulna are often difficult to detect, which in part accounts for the reason that Monteggia fractures are frequently overlooked in children.
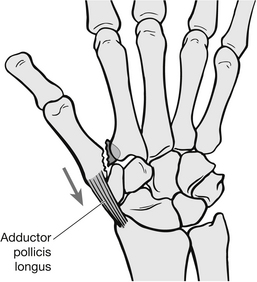
Fractures of the radius
Distal third shaft fractures also occur because of direct force, but are more common because of the lack of soft tissue protection. Isolated fractures are less common than more complicated injury (Goldberg et al. 1992). Dislocation of the radio-ulnar joint is usually concomitant with fractures around the mid-shaft and distal shaft junction. This is called a Galeazzi fracture. These fractures have a high incidence of long-term functional disability and chronic pain when untreated (Perron et al. 2001). Pain is the primary diagnostic feature. Tissue swelling may obscure deformity, but shortening is sometimes apparent. The deforming forces, shown in Table 6.5, make closed reduction less successful than open reduction with internal fixation.
Table 6.5
Deforming forces in Galeazzi fractures
| Mechanism | Deformity |
| Gravity | Subluxation or dislocation of radio-ulnar joint Angulation of radial fracture |
| Pronator quadratus | Rotation of distal fragment in a proximal and volar direction |
| Brachioradialis | Shortening because of distal fragment rotation |
| Thumb abductors and extensors | Compounds shortening |
Wrist injury
Anatomically, the wrist is an area that contains multiple joints connected by ligaments. It extends from the distal radius and ulna to the distal carpal bones (Fig. 6.23). Injury to the wrist usually results from a fall onto an outstretched hand, which causes hyperextension of the hand and force to be exerted on the volar aspect of the radius causing fracture. Injury pattern varies with age, gender and the amount of force involved. The distal radius is a common site of injury in adults. Fractures of this area are broadly grouped into three categories depending on the displacement of the distal radius and ulna. They are known as Colles’, Smith’s and Barton’s fractures.
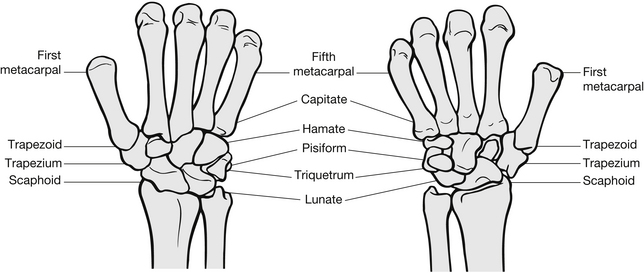
Figure 6.23 The wrist injury.
Colles’ fracture
The most common of these fractures is the Colles’ fracture (Fig. 6.24). This describes a distal radius fracture with dorsal displacement of the distal fragment. This causes a loss of the usual volar tilt and pronation of the distal fragment over the proximal fragment. An associated ulnar styloid fracture is present in 60 % of cases (Cooney et al. 1991). The injury is most prevalent in women over 50 years, particularly those with signs of osteoporosis. Colles’ fractures are easy to identify at initial assessment as the patient presents with classic dinner-fork deformity of the wrist because of dorsal displacement and loss of volar angulation (Harness et al. 2004).
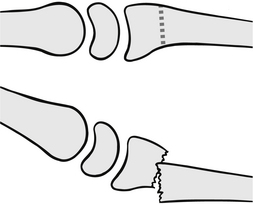
Figure 6.24 Colles’ fracture.
The patient usually has significant swelling around the fracture site and localized pain. Nerve involvement is not uncommon and paraesthesia may be present in areas served by the median or ulnar nerve. Severe swelling can cause vascular compromise and compartment syndrome. Neurovascular function should therefore be carefully checked on assessment. All the digits should be touched to ensure there is feeling and therefore neurological deficit is present, and capillary refill should also be checked. Patients need adequate analgesia and a full explanation of what is going to happen before any examination of the wrist is undertaken (Summers 2005). Management priorities involve restoration of anatomical alignment, in particular the degree of volar tilt, and the exact restoration of a neutral radio-ulnar joint if good function of the wrist is to be restored. Fractures with minimal displacement with no shortening and maintenance of volar tilt are managed in a forearm POP back-slab or split cast with the hand pronated and ulnar deviation, and flexion at the wrist (Brown 1996).
Most displaced fractures can be managed by closed reduction in the ED. To facilitate this, adequate analgesia is required. Debate persists as to which method of anaesthesia is most appropriate, and various methods are discussed in Chapter 26. Bier’s block is often favoured by orthopaedic staff, but demands skilled operators. Haematoma block requires less skill but carries the risk of subsequent tissue toxicity from the lidocaine used, and has been criticized for providing inadequate anaesthesia to complete the reduction (Cooney et al. 1991). Despite this, haematoma block is commonly used and is successful in the treatment of elderly women. As a general rule, haematoma block is not suitable for Colles’ fracture reduction in younger patients, particularly men with greater muscle spasm creating resistance to reduction. An accurate reduction is vital for restoration of full function in younger patients, and therefore multiple attempts at manipulation are sometimes needed. This is more easily facilitated under Bier’s block.
The reduction involves a traction/counter-traction approach, with the first person applying longitudinal traction through the hand to lengthen the radius, while the second applies counter-traction through the forearm until disimpaction of the distal fragment can be felt. Then the first person applies pressure to the top of the distal fragment to reduce it. Again, volar movement will be felt and visible deformity should be resolved. The wrist should be immediately immobilized in a POP slab with ulnar deviation and wrist flexion. Post-reduction X-rays should be obtained to establish the degree of volar tilt, length and neutral radio-ulnar joint position (Greaves & Jones 2002). If this cannot be achieved by closed manipulation, open reduction and internal fixation should be considered. In complicated or severely comminuted injuries, open reduction and internal fixation should be considered and closed manipulation not attempted in ED.
Compartment syndrome, which is the compression of nerves and blood vessels in an enclosed space, can lead to permanent damage of these structures. Summers (2005) recommends the following symptoms of compartment syndrome – the ‘five Ps’ – should be discussed with patients, stressing that, if any of these symptoms manifest themselves, patients should contact their ED for advice.
• pallor, when fingers lose their healthy colour
• pulselessness: instruction needs to have been given on how to perform capillary refill testing and interpret results
As patients with Colles’ type fracture are often older, their social circumstances should be established before discharge to make sure they can cope at home.
Smith’s fractures
In both anatomical presentation and mechanism of injury, a Smith’s fracture represents the opposite of a Colles’ fracture. The distal radius is displaced proximally and the distal fragment is volar to the radial shaft. There are three classifications depending on the direction of the fracture (Fig. 6.25).
Barton’s fractures
These are distal radius fractures with volar or dorsal dislocation of radiocarpal joint. Volar fractures are more common than dorsal (Harness et al. 2004). It differs from Colles’ or Smith’s fracture in that there is always intra-articular dislocation present. Barton’s fractures are often associated with high-velocity trauma (Aggarwal & Nagi 2004) although they can result from a fall upon an outstretched, pronated arm.
Treatment is usually by surgery as conservative care has an elevated risk of complications, including ‘early osteoarthrosis, deformity, subluxation, and instability’ (Aggarwal & Nagi 2004).
Carpal fractures
The carpal bones form two rows (see Fig. 6.23). The proximal row consists of the scaphoid, lunate, triquetrum and pisiform bones. The scaphoid has a bridging position with the distal row which consists of the trapezium, capitate and hamate bones. These bones are supported by three strands of ligaments stemming from the radial styloid. The radial and ulnar arteries provide vascular supply, and the radial, ulnar and median nerves provide neurological function.
Fractures of the carpal bones are less common than other wrist injuries averaging at 8 % compared to phalanges (59 %) and metacarpals (33 %) (Van Onselen et al. 2003, Dennis et al. 2011). These fractures are often associated with ligament injury, creating an unstable wrist joint. Long-term disability is not uncommon in missed fractures. Assessment of wrist injury should focus on the mechanism of injury, force involved, and exact site of impact as well as the age of the patient, wrist anatomy and relative strengths change with age.
Scaphoid fracture
Because of its unique position in relation to the radius and both rows of carpal bones, the scaphoid is the most commonly fractured carpal bone and accounts for between 2 and 7 % of all orthopaedic fractures (McNally & Gillespie 2004). It occurs in both adults and children, most often between early teens and mid-life. The oblong-shaped scaphoid bone derives its name from the Greek word ‘skaphos’ meaning ‘boat’ and is divided into four anatomical areas (Fig. 6.26).
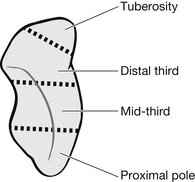
Figure 6.26 The scaphoid bone.
The scaphoid has a good vascular supply to the middle and distal areas, but the proximal pole has no dedicated blood supply. This results in a high incidence of vascular necrosis if fracture union is not rapidly achieved. Scaphoid fractures are usually classified as stable or unstable and time taken to union differs with the fracture location (Box 6.6). Stable fractures that are incomplete or completely undisplaced, heal rapidly and are treated with immobilization. An unstable fracture has been defined as displacement of the fracture by 1 mm or more on X-ray.
The most common mechanism of injury is a fall onto an outstretched hand. Externally, there is little visible evidence of a fracture, although swelling can sometimes be present. The patient will have generalized pain, which is worse on wrist movement, particularly gripping actions. On examination, patients will have specific tenderness in the anatomical snuffbox. The anatomical snuffbox is on the radial aspect of the dorsum of the wrist. They may also have pain when longitudinal pressure is applied to the thumb and index finger, and pain on dorsiflexion of the wrist. To assess the snuffbox, ask the patient to hyperextend the thumb with the wrist slightly deviated in the radial aspect. In this position the snuffbox becomes visible. The scaphoid can be palpated proximally in the floor of the snuffbox. The trapezium can be palpated distally. This test is sensitive but not specific (Phillips et al. 2004). Tenderness of the scaphoid tubercle is also a sensitive test but is more specific. To examine this with one hand extend the patient’s wrist while applying pressure on the scaphoid tuberosity at the proximal wrist crease with the other. If there is no tenderness with these two tests, a scaphoid fracture is unlikely.
X-ray findings can be misleading as up to 20 % of patients with scaphoid fracture have normal initial X-rays (McNally & Gillespie 2004). Fractures not initially visible on X-ray will be apparent between 10–14 days post-injury (Hunter 2005). For this reason diagnosis should be based on clinical findings, specifically, mechanism of injury and localized tenderness in the anatomical snuffbox. Management of scaphoid fractures can be controversial (Hunter 2005). At present most non-complex fractures are treated conservatively with an excellent healing rate, however where the facilities and skill exist surgical treatment is increasing in popularity with a 100 % union rate and reduced immobilization time required (Vinnars et al. 2008). A general consensus exists that all fractures, whether clinical or radiological, should be immobilized as failure to do this can result in delayed or non-union healing or avascular necrosis. A POP cast or splint that incorporates the forearm and thumb, with the wrist in slight volar flexion, should be used. Complicated fractures should be referred to the orthopaedic team because of the risk of avascular necrosis. Some fractures are internally fixed at an early stage to prevent non-union and to ensure good functional recovery (Chin et al. 2009).
Triquetrum fractures
The triquetrum is the second most commonly fractured carpal bone. Such fractures often occur with other carpal fractures or perilunate dislocation. Isolated injury is less common and usually minor. Triquetrum fractures are usually caused by hyperextension injury of significant force. The patient usually complains of pain over the dorso-ulnar area of the wrist. Management involves a short arm POP cast or splint for 3–6 weeks in the case of isolated injury or referral to the orthopaedic team where the fracture is associated with other wrist injuries. Other carpal fractures generally occur as part of a more complicated hand or wrist injury, and demand specialist orthopaedic input after initial diagnosis in the ED.
Perilunate and lunate dislocation
These dislocations occur as a result of disruption to the lesser arc of ligaments. They can be graded into four groups depending on the degree of disruption (Box 6.7). They are caused by extreme hyperextension, which might occur due to a motorcycle accident or fall from a height. Because of the force needed to cause perilunate and/or lunate dislocation, concurrent injury is common. The patient presents with extreme pain and a fork-type deformity, and is usually unable to hold the fingers in a flexed position. Nerve disruption is not uncommon, so paraesthesia may also be present. Fractures and severe ligament disruption are usual with these injuries, which should always be managed by the orthopaedic team and often require open reduction when associated with fractures.
Hand injury
The hand is a complex structure whose skeletal outline is shown in Fig. 6.27. The back of the hand is referred to as the dorsal aspect and the palm of the hand the volar aspect. The intricate mechanisms of hand movement are particularly vulnerable to injury because of its environmental exposure and functional purpose. Hand function relies on intact muscle and tendon structures and sensory motor connection to the central nervous system, as well as adequate circulation. The treatment of any hand injury revolves firstly around restoring function and secondly around appearance. Anatomy will be considered in greater detail where relevant to specific injuries.
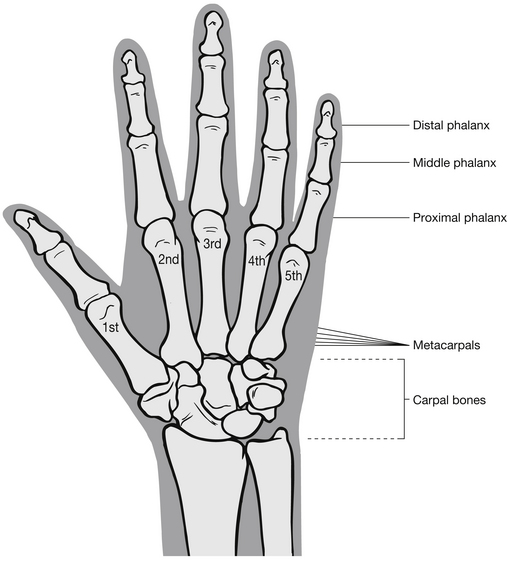
Figure 6.27 Anatomy of the hand.
Base of first metacarpal fractures
Extra-articular fractures occur within the joint capsule, but do not involve the articular surface of the joint (Fig. 6.28) and are the most common fracture type. These injuries are usually managed by closed reduction and POP cast incorporating the thumb. In order to retain good function, it is important not to hyperextend the thumb at the metacarpophalangeal joint. Some oblique fractures may remain unstable with closed reduction and plaster immobilization alone, and therefore orthopaedic referral for percutaneous pinning is necessary.
Intra-articular fractures can be divided into two groups: the more common Bennett’s fracture and Rolando’s fracture. The Bennett’s fracture is categorized by the displacement of the metacarpal shaft while the palmar articular fragment retains its correct anatomical location as shown in Fig. 6.29. The mechanism of injury is similar to that of an extra-articular fracture, with interpersonal fracas being a common cause of injury. The patient has limited movement of the base of the thumb with pain and swelling around the area. Effective emergency management is essential to prevent degenerative post-traumatic arthritis and to restore adequate range of movement. This injury is considered unstable because of the adductor pollicis longus tendon, which is attached to the base of the first metacarpal. Its tensile strength prevents union of fracture without the aid of percutaneous pins or orthopaedic reduction and internal fixation.
Rolando’s fracture is similar to a Bennett’s fracture, but in addition to the palmar articular fragment remaining in place, the dorsal fragment displaces from the base, creating a Y-shaped or more severely comminuted base of metacarpal fracture. Mechanism of injury and patient presentation are similar to those of a Bennett’s fracture, but the prognosis is poor as functional integrity is difficult to restore with orthopaedic reduction and internal fixation or closed reduction and immobilization. Persistent pain and degenerative arthritis are common.
Phalangeal fractures of the thumb are generally managed in the same manner as fingers.
Shaft of metacarpal fracture
These are caused by a number of mechanisms of injury (Table 6.6). Principles of management revolve around correction of any rotation, angulation and shortening of the finger to ensure functional recovery. Even a small degree of rotation can cause problems with flexion of the metacarpo-phalangeal joint. Effective closed reduction and immobilization are usually achievable in ED unless severe swelling or open fractures exist. If rotation cannot be corrected with manipulation, the patient should be referred for percutaneous pinning or orthopaedic reduction and internal fixation.
Table 6.6
| Type | Cause |
| Transverse | Direct blow |
| Oblique | Torque force |
| Comminuted | Crush injury/gunshot wound |
Metacarpal neck fractures
Fifth metacarpal neck fracture, known as Boxer’s fracture, is one of the most common hand injuries treated in the ED and usually results from a punch injury. Management of these fractures is controversial (Winter et al. 2007), but there is a consensus that any rotational injury needs manipulation and either splinting or wiring. Volar angulation can, however, be treated in a number of ways, ranging from orthopaedic reduction and internal fixation to no treatment and early mobilization (Winter et al. 2007).
Clinical trials (Rusnak 1995) have found that no treatment at all or supportive splinting which facilitates mobilization has quicker functional repair, with minimal cosmetic deformity in the majority of cases. Where closed reduction is carried out, maintaining that reduction is difficult without causing further damage to the function of the hand. This is because 70° of flexion at the metacarpo-phalangeal joint is necessary to prevent contractures, but this position will not provide the three-point fixation needed to stabilize the metacarpal neck.
Soft tissue injury
Soft tissue injuries are commonly treated in ED and are usually considered ‘minor’ in nature by emergency staff. The impact on the patient, however, is far from minor; loss of normal function in the short term is common, usually because of pain. If soft tissue injuries are not detected and treated properly, long-term or recurrent problems can occur. Soft tissue injury (STI) is the all-encompassing term given to injury to muscles, ligaments, tendons and skin. As a result, the diagnosis of a STI has a number of possible causative factors. The common ones are described below.
A treatment common to all STIs is that of non-steroidal anti-inflammatory drugs (NSAIDs). This treatment is becoming increasingly questioned. NSAIDs can reduce pain and swelling enabling earlier mobilization and therefore recovery. However, the argument is that swelling is a recognized part of the healing process and this treatment should not routinely be used on acute injuries (Stovitz & Johnson 2003).
Sprains
These are injuries to the fibres of ligaments supporting a joint. This results from abnormal movement of the joint causing stretching and tearing of the ligament. The degree of this varies from partial tearing to total disruption of the ligament complex supporting a joint (Table 6.7).
Table 6.7
| Physiology | Clinical signs | |
| First degree | Minor tearing of ligament fibres with mild haemorrhage | Minimal swelling Tenderness over ligaments – worse with motion, stressing the ligaments |
| Second degree | Partial tear with moderate haemorrhage and reduced active motion | Significant pain – worse with passive movement and swelling Injuries prone to recurrence and can cause joint instability |
| Third degree | Complete rupture of ligament Moderate haemorrhage with significant loss of function |
Less painful with significant swelling and abnormal motion of joint on active/passive movement Usually need surgical repair if joint instability exists |
The patient will present with mechanisms of injury and symptoms similar to those with fractures. The joint has often been subjected to forces in opposite or abnormal directions, creating joint stress. The patient will usually describe a sudden onset of acute pain, and often describe hearing a ‘snap’ at the time of injury. Many patients are convinced this means they have broken their limb and the nurse must therefore be careful to assess the injury thoroughly and provide the appropriate reassurance (Loveridge 2002, Smith 2003) without offending by implying the injury should not be seen in ED. Although specific injury management can vary, common RICE principles of sprain management apply:
• Rest – most acute sprains benefit from a 48-hour period of rest, with minimal use.
• Ice – used as a first aid measure either as an ice pack, or wrapped crushed ice. The intention is to help decrease both pain and swelling although there is little evidence to confirm improved clinical outcomes result in its use (Collins 2008). The patient should be advised to apply the ice for 10–15 minutes every 2–3 hours for the first 12 hours post-injury.
• Compression – elastic tubular bandages or strapping are utilized to provide support for the injury and help to reduce swelling although there is debate about the efficacy of elasticated tubular bandages (Beynnon et al. 2006). Where a tubular bandage is applied, the patient should remove it at night to prevent oedema distal to the injury. In severe sprains, POP casts or braces may be more appropriate for specific injuries.
• Elevation – together with ice packs and rest, elevation of the injured part helps to reduce the accumulation of blood and lymph in tissues surrounding the injury, which in turn reduces both pain and healing time (Safran et al. 1999). This is particularly important for distal limb injuries, such as those of the hand, foot or ankle.
Strains
These are injuries to muscles and tendons. They occur after forced stretching or sudden violent contraction. As with sprains, the severity of strain injury is classified by the extent of damage (Table 6.8).
Table 6.8
| Physiology | Clinical signs | |
| First degree | Minor tearing of muscle/tendon unit | Spasm, swelling and localized pain |
| Second degree | More severe pain but incomplete tearing of fibres | Muscle spasm, swelling, localized pain and loss of strength |
| Third degree | The muscle or tendon is completely disrupted with separation of muscle from tendon, tendon from muscle or tendon from bone | Palpable defect is often present Muscle spasm, pain, swelling and loss of function |
Treatment of strains is similar to that of sprains. Management of first-degree strains involves rest, ice, compression and elevation as described under ‘sprains’ above. Second-degree injuries may require immobilization, depending on the site affected, and usually take longer to heal. Third-degree injuries should be immobilized and the patient referred for early orthopaedic consultation at the fracture/STI clinic. Some injuries benefit from surgical repair, but many require simple immobilization. Many factors influence this decision: the site of injury, as well as the age, activity level and occupation of the patient (Loveridge 2002).
Tendinitis
This is an inflammatory condition usually caused by overuse. Less commonly it is caused by direct trauma. The patient complains of pain at the point where the tendon attaches to bone. Pain is worse on movement and function is sometimes restricted. Occasionally, palpable crepitus exists. Common sites include the rotator cuff of the shoulder (supraspinatus tendonitis), the insertion of hand extensors to the humeral lateral epicondyle (tennis elbow), the medial epicondyle (golfer’s elbow), the radial aspect of the wrist (De Quervain’s tenosynovitis) and the Achilles tendon. Management principally involves rest. NSAIDs are often used but their efficacy is currently debated particularly where overuse and degeneration are present (Khan et al. 2000).
Bursitis
This condition is most common in middle age (Genge Jagmin 1995). The patient usually presents to the ED with a swelling at 2–3 days post-injury or strain. Pain can increase gradually over this time or may be of sudden onset. It is usually worse on movement and radiates distally from the site of bursitis. The area will appear classically inflamed with erythema and swelling and will be hot to the touch. Areas commonly affected include the knee (Adams 2004), elbow and big toe (gout bursitis).
Specific soft tissue injuries
Knee injury
The knee gives support and flexibility to body movement. Ligaments and musculotendinous structures maintain its stability. The knee joint is the most complicated joint in the body (Snell 2000, Adams 2004) and because of its load-bearing task it is very susceptible to injury, particularly during sporting activities such as rugby and football. Medial injuries tend to be the most common; lateral injuries, however, are often more disabling. A history of an audible snap at time of injury is suggestive of anterior cruciate rupture. The mechanism of injury gives a strong indication of the likely structural damage, so accurate history-taking is vital (Table 6.9).
Table 6.9
| Force | Cause | Injury |
| Hyperextension Forced flexion | Running/sudden deceleration, e.g., from rugby tackles | Tearing of anterior cruciate ligament |
| Twisting or flexed knee injury | Direct or blunt trauma | Meniscal injury |
| Valgus stress with external rotation | Skiing | Medial collateral ligament injury |
| Varus stress internal rotation | Skiing in snow plough position | Lateral collateral ligament |
| Direct force | Fall, hitting dashboard in RTA | Posterior cruciate ligament |
Patients may also present to the ED with knee pain but no history of trauma. In such presentations other diagnoses such as Baker’s cyst, osteoarthritis or in rare cases septic arthritis should be considered.
Achilles tendon rupture
The Achilles tendon is the largest, thickest and strongest tendon in the body and after the quadriceps is the second most ruptured supporting tissue (Kerr 2005). Achilles tendon rupture is a common tennis and badminton injury, associated with sudden jumping movements with a heavy landing. The patient complains of a sudden sharp pain at the back of the ankle, not dissimilar to a direct blow. Swelling is present in some cases, as is bruising, but often it is simply pain and the mechanism of injury which initially indicate Achilles tendon rupture. The calf squeeze test (Simmonds’ test) is useful in confirming diagnosis. The patient kneels backwards over a chair or lies face down on a trolley with the ankles over the end. When the calf is squeezed, plantar flexion of the ankle should occur unless the Achilles tendon is ruptured (Bickley & Szilagyi 2008). All of these patients should be referred for orthopaedic follow-up.
Most are initially managed in long leg equinous plaster, with the ankle in plantar flexion. Some patients benefit from surgical repair, particularly young athletic people. Patient outcomes appear similar whether or not open repair is performed (Mayeda 2009). Achilles tendinitis should not be confused with partial rupture. Tendinitis is caused by overuse or sudden change in activity such as dancing or running. The patient will have localized pain, swelling and crepitus over the tendon. The range of movement will be normal but painful. The patient should be treated with rest and analgesia with or without NSAIDs.
Ankle sprain
Large numbers of patients with ankle injuries are treated in ED, and one of the priorities for ED nurses lies with identifying serious or potentially limb-threatening injury (Loveridge 2002). Assessment for all ankle injuries should be systematic and thorough, although the majority will turn out to be straightforward sprains. Assessment should include mechanism of injury, the most common being an inversion injury causing damage to the anterior talofibular ligaments. This results from slipping off kerbs or twisting the ankle in a manner where the sole of the foot turns inwards.
Eversion injury is less common, but is more likely to be associated with an avulsion fracture and causes damage to the deltoid ligament; it is characterized by an injury where the sole of the foot turns outwards. Patients will often have heard a ‘snap’ or ‘crack’ at the time of injury which they will probably associate with a broken bone. The nurse needs to provide reassurance as well as a thorough assessment, particularly when an X-ray is not clinically indicated (see Ottawa ankle rules, Fig 6.13). The patient with an ankle sprain usually has pain at the site of injury, swelling over that area, and reduced mobility because of pain. Examination usually identifies the area immediately below the respective malleolus to be the most severe point of pain, as opposed to a fracture where pain is worse over the bony prominence.
Rotator cuff injury
The varied mobility of the shoulder joint makes it susceptible to injury (Ryan 2004). Shoulder stability is maintained by the rotator cuff. It comprises a sheath of muscles listed in Table 6.10. Degenerative conditions such as rheumatoid arthritis are not uncommon and increase the likelihood of injury. Acute injury includes tearing or tendinitis. The supraspinatus is the most commonly injured area; this results from falls with hyperextension or hyperabduction of the shoulder. Rest and analgesia comprise the management of choice, and most patients benefit from orthopaedic follow-up, as recurrent injury is not uncommon.
Table 6.10
| Muscle | Action |
| Infraspinatus | External rotation |
| Teres minor | External rotation |
| Subscapularis | Internal rotation |
| Supraspinatus | Internal rotation |
Mallet finger
This occurs as a result of forced flexion of the distal interphalangeal (DIP) joint or by a direct blow to the end of the finger, and is an injury commonly sustained by netball players. It is caused by rupture or avulsion of the extensor tendon. If an avulsion fracture of the distal phalanx is present, healing is usually more rapid than a tendon rupture. The patient presents in the ED with pain and a deformed finger and is unable to actively extend the fingertip distal to the DIP joint, causing drooping of the distal phalanges which may be slight or severe (Wang & Johnston 2001). Management involves splinting the finger to below the DIP joint in slight hyperextension. Patient education and cooperation are vital to the success of this treatment. The splint is usually plastic and needs to be removed frequently to clean the finger and prevent skin damage. It is important, however, that hyperextension of the DIP joint is maintained during this time. The patient should therefore be taught to apply and remove the splint while supporting the fingertip on a firm surface.
Compartment syndrome
Compartment syndrome is a common but potentially life-threatening condition that requires prompt treatment and recognition. Caused by high pressure in a closed fascial space so that capillary perfusion is too low for tissue viability, it is well recognized as a potentially devastating complication of fractures (Edwards 2004, Kashuk et al. 2009). If this pressure is allowed to rise and stay high, it causes permanent damage to the soft tissue structures and nerves within that compartment. The limbs contain compartments, so injuries where swelling occurs have the potential to cause compartment syndrome. The forearm contains dorsal and volar compartments, and the lower leg is divided into four compartments: lateral, anterior, superficial posterior and deep posterior. In addition to internal tissue swelling, constricting dressings or POP which is too tight can cause compartment syndrome. This is one reason why casts on new injuries tend to be either split or bivalved or back-slabs are applied.
• bleeding into the compartment, perhaps following a fracture or rupture of small vessels, will result in clot formation and increased compartmental pressure
• muscle swelling – this usually occurs after a period of ischaemia, e.g., following vascular damage.
If any restrictive splints or dressings are in place these should be removed and the limb elevated in an attempt to reduce swelling. Initial treatment with mannitol can decompress compartment syndrome and avoid the need for surgery (Porter & Greaves 2003); however, if conservative treatment fails to restore sensation and relieve pain, fasciotomy will be necessary to prevent long-term damage. Fasciotomy has a high complication rate, however, as it transforms a closed lesion into an open wound (Fitzgerald et al. 2000). In all patients susceptible to compartment syndrome, early involvement of the orthopaedic and/or vascular team is essential. Specialist tissue-pressure monitoring gives an accurate portrait of how the patient is responding to conservative management and an indication of how quickly to intervene with fasciotomies. If left unchecked, the cycle of oedema and ischaemia results in muscle infarction, nerve injury and permanent loss of function in the extremity (Edwards 2004).
Conclusion
Musculoskeletal injury is one of the most common types of presentation to EDs. As this chapter has highlighted, it is imperative for emergency nurses to be able to assess musculoskeletal injury and identify life- or limb-threatening trauma, some of which may not seem devastating at first glance. An understanding of the underpinning anatomy and physiology of the musculoskeletal system has been provided in order to inform clinical decision-making and meet the needs of the individual patient and avoid long-term, preventable disability. As most of these patients will be discharged from the ED, the nurse has a crucial role as health educator in ensuring the patient looks after their injury, and prevents or minimizes long-term sequelae. In doing so, the emergency nurse may be assured of delivering quality care to this vulnerable group of patients.
References
Adams, N. Knee injuries. Emergency Nurse. 2004;11(10):19–27.
Aggarwal, A.K., Nagi, O.N. Open reduction and internal fixation of volar Barton’s fractures: A prospective study. Journal of Orthopaedic Surgery. 2004;12(2):230–234.
American College of Surgeons. Advanced Trauma Life Support, eighth ed. Chicago: American College of Surgeons; 2008.
Audit Commission. United they Stand: Coordinating Care for Elderly People with Hip Fractures. London: The Stationary Office; 2000.
Babal, J.C., Mehlman, C.T., Klein, G. Nerve injuries associated with pediatric supracondylar humeral fractures: A meta-analysis. Journal of Pediatric Orthopedics. 2010;30(3):253–263.
Bachmann, L.M., Kolb, E., Koller, M.T., et al. Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot: a systemic review. British Medical Journal. 2003;326(7386):405–406.
Beynnon, B.D., Renström, P.A., Haugh, L., et al. A prospective, randomized clinical investigation of the treatment of first-time ankle sprains. American Journal of Sports Medicine. 2006;34(9):1401–1412.
Bickley, L.S., Szilagyi, P.G. Bates’ Guide to Physical Examination and History Taking, tenth ed. Philadelphia: Lippincott, Williams & Wilkins; 2008.
Bickley, L.S., Szilagyi, P.G. Bates’ Pocket Guide To Physical Examination And History Taking, sixth ed. Philadelphia: Lippincott, Williams & Wilkins; 2009.
Bowie, D. Choosing the right pain relief for patients with soft-tissue injuries. Emergency Nurse. 2011;19(2):28–30.
Brown, A.F.T. Accident & Emergency Diagnosis and Management. Oxford: Butterworth-Heinemann; 1996.
Cadogan, M. Femur injuries. In Cameron P., Jelinek G., Kelly A.M., Murray L., Brown A.F.T., Heyworth J., eds.: Textbook of Emergency Medicine, second ed, Edinburgh: Churchill Livingstone, 2004.
Chin, H.W., Propp, P.A., Orban, D.J. Forearm and wrist. In Marx J., Hockberger R., Walls R., eds.: Rosen’s Emergency Medicine: Concepts and Clinical Practice, seventh ed, St Louis: Mosby Year Book, 2009.
Ciernick, I.F., Meier, L., Hollinger, A. Humeral mobility after treatment with a hanging cast. Journal of Trauma. 1991;31(2):230–233.
Clasper, J., Ramasamy, A. Open fractures. In: Smith J., Greaves I., Porter K., eds. Oxford Desk Reference: Major Trauma. Oxford: Oxford Medical Publications, 2011.
Cole, P.A. Scapula fractures. Orthopedic Clinics of North America. 2002;33(1):1–18.
Collins, N.C. Is ice right? Does cryotherapy improve outcome for acute soft tissue injury? Emergency Medicine Journal. 2008;25(2):65–68.
Cooney, W.P., Linscheid, R.L., Dobyns, J.H., Fractures and dislocations of the wrist. Rockward, C.A., et al, eds. Fractures in Adults, vol. 1. Philadelphia: JB Lippincott, 1991.
Dennis, H.H., Sze, A.C., Murphy, D. Prevalence of carpal fracture in Singapore. Journal of Hand Surgery. 2011;36(2):278–283.
Dickinson, K., Roberts, I. Medical antishock trousers (pneumatic antishock garments) for circulatory support in patients with trauma [Cochrane review]. Cochrane Database Systematic Review. 2004;4:2–CD001856.
Edwards, S. Acute compartment syndrome. Emergency Nurse. 2004;12(3):32–38.
Eisenhart, A.W., Gaeta, T.J., Yens, D.P. Osteopathic Manipulative Treatment in the Emergency Department for Patients With Acute Ankle Injuries. Journal of the American Osteopathic Association. 2003;103(9):417.
El-Adl, W.A., El-Said, M.A., Boghdady, G.W., et al. Results of treatment of displaced supracondylar humeral fractures in children by percutaneous lateral cross-wiring technique. Strategies in Trauma and Limb Reconstruction. 2008;3(1):1–7.
Fayaz, H.C., Jupiter, J.B. Monteggia fractures in adults. Acta Chirurgiae Orthopaedicae et Traumatologiae Cechoslovaca. 2010;77(6):457–462.
Fitzgerald, A.M., Wilson, Y., Quaba, A., et al. Long-term sequelae of fasciotomy wounds. British Journal of Plastic Surgery. 2000;53(8):690–693.
Garden, R.S. Stability and union in subcapital fractures of the femur. Journal of Bone and Joint Surgery. 1964. [46-B, 630].
Genge Jagmin, M. Musculoskeletal injuries. In Kitt S., Selfridge-Thomas J., Proehl J.A., Kaiser J., eds.: Emergency Nursing: A Physiologic and Clinical Perspective, second ed, Philadelphia: Saunders, 1995.
Georgilas, I., Mouzopoulos, G. Anterior ankle dislocation without associated fracture: a case with an 11 year follow-up. Acta Orthopaedica Belgica. 2008;74(2):266–269.
Goldberg, H.D., Young, J.W.R., Reiner, B.I. Double injuries of the forearm: a common occurrence. Radiology. 1992;185(1):223–227.
Gordon, W.T., Grijalva, S., Potter, B.K. Damage control and austere environment external fixation: Techniques for the civilian provider. Journal of Orthopaedic Advances. 2012;21(1):22–31.
Greaves, L., Jones, J. Practical Emergency Medicine. London: Arnold; 2002.
Harness, N., Ring, D., Jupiter, J.B. Volar Barton’s fractures with concomitant dorsal fracture in older patients. The Journal of Hand Surgery. 2004;29A(3):439–445.
Harris, C.R. Ankle injuries. In: Ruiz E., Cicero J.J., eds. Emergency Management of Skeletal Fractures. St Louis: Mosby, 1995.
Harris, C.R., Haller, P.R. The tibia and tibula. In: Ruiz E., Cicero J.J., eds. Emergency Management of Skeletal Fractures. St Louis: Mosby, 1995.
Hauschild, O., Strohm, P.C., Culemann, U., et al. Mortality in patients with pelvic fractures: results from the German pelvic injury register. The Journal of Trauma Injury, Infection and Critical Care. 2008;64(2):449–455.
Herrera-Soto, J.A., Scherb, M., Duffy, M.F., et al. Fractures of the fifth metatarsal in children and adolescents. Journal of Pediatric Orthopedics. 2007;27(4):427–431.
Hopkins, M. A comparative analysis of the application of the Ottawa ankle rule. International Emergency Nursing. 2010;18(4):188–195.
Hovelius, L., Olofsson, A., Sandström, B., et al. Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger: A prospective twenty-five year follow-up. The Journal of Bone & Joint Surgery. 2008;90(5):945–952.
Hunter, D. Diagnosis and management of scaphoid fractures: a literature review. Emergency Nurse. 2005;13(7):22–26.
Ingram, M.D., Watson, S.G., Skippage, P.L., et al. Urethral injuries after pelvic trauma: Evaluation with urethrography. RadioGraphics. 2008;28(6):1631–1643.
Kashuk, J.L., Moore, E.E., Pinski, S., et al. Lower extremity compartment syndrome in acute care surgery paradigm: safety lessons learned. Patient Safety in Surgery. 2009;3(11):11–16.
Khan, K.M., Cook, J.L., Taunton, J.E., et al. Overuse tendinosis, not tendonitis part 1: a new paradigm for a difficult clinical problem. The Physician and Sports Medicine. 2000;28(5):38–48.
Kelly, A.M. Injuries of the shoulder girdle. In Cameron P., Jelinek G., Kelly A.M., Murray L., Brown A.F.T., Heyworth J., eds.: Textbook of Emergency Medicine, second ed, Edinburgh: Churchill Livingstone, 2004.
Kerr, J. Achilles tendon injury: assessment and management in the ED. Emergency Nurse. 2005;13(2):32–38.
Knapton, P. Shoulder injury: A case study. Emergency Nurse. 1999;6(10):25–28.
Kyle, R.F., Gustilo, R.B., Premer, R.F. Analysis of 622 intertrochanteric hip fractures: a retrospective and prospective study. Journal of Bone and Joint Surgery. 1979;61(2):216.
Larsen, D. Assessment and management of foot and ankle fractures. Nursing Standard. 2002;17(6):37–46.
Lisk, R., Raison, N., Lawton, K., et al. Improving the management of pressure ulcer care in fracture neck of femur patients Communications to the Spring Meeting of the British Geriatrics Society. BT Convention Centre Liverpool; 2011. [p32. 4–6_May_2011].
Logan, A.J., Lindau, T.R. The management of distal ulnar fractures in adults: a review of the literature and recommendations. Strategies in Trauma and Limb Reconstruction. 2008;3(2):49–56.
Loveridge, N. Lateral ankle sprains. Emergency Nurse. 2002;10(2):29–33.
Lynch, T.H., Martínez-Piñeiro, L., Plas, E., et al. EAU guidelines on urological trauma. European Urology. 2005;47(1):1–15.
Magnusson, A.R. Humerus and Elbow. In Marx J., Hockberger R., Walls R., eds.: Rosen’s Emergency Medicine: Concepts and Clinical Practice, seventh ed, St Louis: Mosby Year Book, 2009.
Mattox, K.L., Bickell, W., Pepe, P.E., et al. Prospective MAST study in 911 patients. Journal of Trauma. 1989;29(8):1104–1111.
Mayeda, D.V. Ankle and foot. In Marx J., Hockberger R., Walls R., eds.: Rosen’s Emergency Medicine: Concepts and Clinical Practice, seventh ed, St Louis: Mosby Year Book, 2009.
Mayfield, J.K., Johnson, R.P., Kilcoyne, R.F. Carpal dislocations: pathomechanics and progressive perilunar instability. Journal of Hand Surgery. 1980;5(3):226–241.
McNally, C., Gillespie, M. Scaphoid fractures. Emergency Nurse. 2004;12(1):21–25.
McRae, R. Pocketbook of Orthopaedics and Fractures. Edinburgh: Churchill Livingstone; 2006.
Middleton, P. Trauma retrieval. In: Smith J., Greaves I., Porter K.M., eds. Oxford Desk Reference: Major Trauma. Oxford: Oxford University Press, 2011.
Mills, K., Morton, R., Page, G. Color Atlas and Text of Emergencies, second ed. London: Mosby-Wolfe; 1995.
National Clinical Guideline Centre. The management of hip fracture in adults. London: Royal College of Physicians; 2011.
Nowotarski, P.J., Turen, C.H., Brumback, R.J., et al. The Journal of Bone and Joint Surgery America. 2000;82(6):781.
O’Dwyer, H., O’Sullivan, P., Fitzgerald, D., et al. The fat pad sign following elbow trauma in adults: its usefulness and reliability in suspecting occult fracture. Journal of Computer Assisted Tomography. 2004;28(4):562–565.
O’Steen, D. Orthopaedic and neurovascular trauma. In Newbery L., ed.: Sheehy’s Emergency Nursing: Principles and Practice, fifth ed, St Louis: Mosby, 2003.
Perron, A.D., Hersh, R.E., Brady, W.J., et al. Orthopedic pitfalls in the ED: Galeazzi and Monteggia fracture-dislocation. American Journal of Emergency Medicine. 2001;19(3):225–228.
Phillips, T.G., Reibach, A.M., Slomiany, W.P. Diagnosis and management of scaphoid fractures. American Family Physician. 2004;70(5):879–884.
Porter, K., Greaves, I. Crush injury and crush syndrome: a consensus statement. Emergency Nurse. 2003;11(6):26–30.
Proehl, J. Emergency Nursing Procedures, fourth ed. Philadelphia: WB Saunders; 2009.
Quday, K. Shoulder injuries. In: Ruiz E., Cicero J.J., eds. Emergency Management of Skeletal Fractures. St Louis: Mosby, 1995.
Rana, M., Banerjee, R. Scapular Fracture After Electric Shock. Annals of the Royal College of Surgeons England. 2006;88(2):143.
Rourke, K. An orthopaedic nurse practitioner’s practical guide to evaluating knee injuries. Journal of Emergency Nursing. 2003;29(4):366–372.
Routt, M.L., Jr., Nork, S.E., Mills, W.J. High energy pelvic ring disruptions. Orthopedic Clinics of North America. 2002;33:59–72.
Rowley, D.I., Dent, J.A. The Musculoskeletal System: Core Topics in the New Curriculum. London: Arnold; 1997.
Ruiz, E. Pelvic, sacral and acetabular fractures. In: Ruiz E., Cicero J.J., eds. Emergency Management of Skeletal Fractures. St Louis: Mosby, 1995.
Rusnak, R.A. Examination of the hand and management of finger-tip injuries. In: Ruiz E., Cicero J.J., eds. Emergency Management of Skeletal Fractures. St Louis: Mosby, 1995.
Ryan, A. Rotator cuff tears. Emergency Nurse. 2004;12(4):27–37.
Safran, M.R., Achazewski, J.E., Benedetti, R.S., et al. Lateral ankle sprains: a comprehensive review. Part 2: treatment and rehabilitation with an emphasis on the athlete. Medicine and Science in Sports and Exercise. 1999;31(7):S438–S447.
Scalea, T.M., Burgess, A.R. Pelvic fractures. In Moore E.E., Feliciano D.V., Mattox K.L., eds.: Trauma, fifth ed, New York: McGraw-Hill, 2004.
Schatzker, J., McBroom, R., Bruce, D. The tibial plateau fracture: the Toronto experience, 1968–1975. Clinical Orthopeadics and Related Research. 1979;138:94–104.
Schmidt, M., Armbrect, A., Havermann, D. Results of surgical management of scapula fractures. 78th annual meeting of the Swiss Society of Accident Surgery and Occupational Diseases. Z-Unfallchir Versicherungsmed. 1992;85:186–188.
Smith, M. Ankle sprain: A literature search. Emergency Nurse. 2003;11(3):12–16.
Smith, M. Orthopaedic trauma. In: O’Shea R.A., ed. Principles and Practice of Trauma Nursing. Edinburgh: Elsevier Churchill Livingstone, 2005.
Snell, R.S. Clinical Anatomy for Medical Students, sixth ed. Philadelphia: Lippincott Williams, Wilkins; 2000.
Snyder, P.E. Fractures. In Maher A.B., Salmond S.W., Pellino T.A., eds.: Orthopaedic Nursing, second ed, Philadelphia: WB Saunders, 2002.
Starr, A.J., Griffin, D.R., Reinert, C.M., et al. Pelvic ring disruptions: Prediction of associated injuries, transfusion requirement, pelvic arteriography, complications, and mortality. Journal of Orthopaedic Trauma. 2002;16(8):553–561.
Stiell, I.G., Greenberg, G.H., McKnight, R.D., et al. A study to develop clinical decision rules for the use of radiography in acute ankle injuries. Annals of Emergency Medicine. 1992;21(4):384–390.
Stovitz, S., Johnson, R. NSAIDs and musculoskeletal treatment. What is the evidence? The Physician and Sports Medicine. 2003;31(1):35–41.
Summers, A. Recognising and treating Colles’ type fractures in emergency care settings. Emergency Nurse. 2005;13(6):26–33.
Tsai, A.K., Ruiz, E. The elbow joint. In: Ruiz E., Cicero J.J., eds. Emergency Management of Skeletal Fractures. St Louis: Mosby, 1995.
Van Onselen, E.B.H., Karim, R.B., Joris Hage, J., et al. Journal of Hand Surgery (British and European Volume. 2003;28B(5):491–495.
Vinnars, B., Pietreanu, M., Bodestedt, A., et al. Nonoperative compared with operative treatment of acute scaphoid fractures – A randomized clinical trial. The Journal of Bone and Joint Surgery, American volume. 2008;90(6):1176–1185.
Wang, Q.C., Johnson, B.A. Fingertip injuries. American Family Physician. 2001;63:1961–1966.
Ward, W. Key issues in nurse requested X-rays. Emergency Nurse. 1999;6(9):19–23.
Wickham, N. Pressure area care in A&E: Part Two. Emergency Nurse. 1997;5(4):25–29.
Wilkins, K.E. Changes in the Management of Monteggia Fractures. Journal of Pediatric Orthopaedics. 2002;22(4):548–554.
Winter, M., Balaguer, T., Bessière, C., et al. Surgical treatment of the boxer’s fracture: transverse pinning versus intramedullary pinning. Journal of Hand Surgery European Volume. 2007;32(6):709–713.
Wyatt, J.P., Illingworth, R.N., Clancy, M.J., Munro, P., Robertson, C.E. Oxford Handbook of Accident and Emergency Medicine. Oxford: Oxford University Press; 1999.
Yuen, M.C., Yap, P.G., Chan, Y.T., et al. An easy method to reduce anterior shoulder dislocation: the Spaso technique. Emergency Medicine Journal. 2001;18(5):370–372.
Zacchilli, M.A., Owens, B.D. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. The Journal of Bone and Joint Surgery (American). 2010;92(3):542–549.
Zagorski, J.B., Latta, L.I., Zych, G.A., et al. Diaphyseal fractures of the humerus treatment with prefabricated braces. Journal of Bone and Joint Surgery. 1988;70A:607–610.