Splenic autoinfarction: Absent or small calcified spleen
• Extramedullary hematopoiesis: Most commonly paravertebral soft tissue masses of homogeneous density
• Findings of iron deposition due to repetitive transfusions
 , indicating chronic and possibly acute infarction.
, indicating chronic and possibly acute infarction.
 that was heavily calcified on microscopy.
that was heavily calcified on microscopy.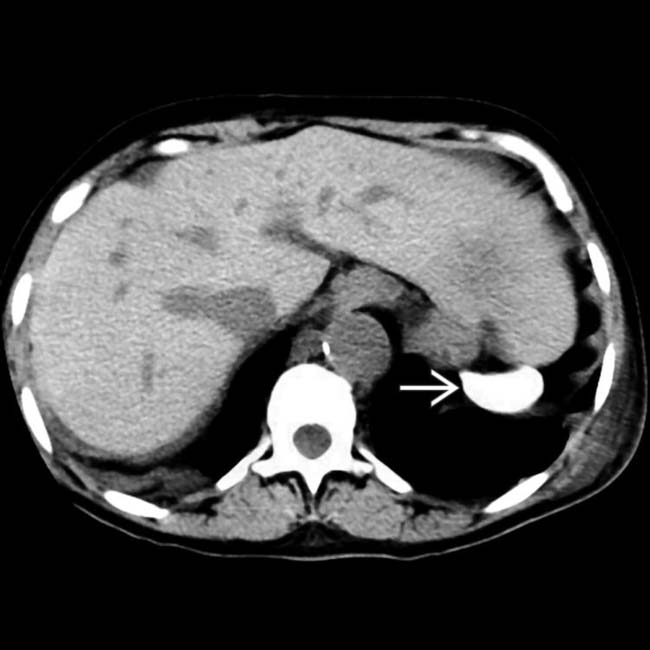
 , also known as autosplenectomy.
, also known as autosplenectomy.
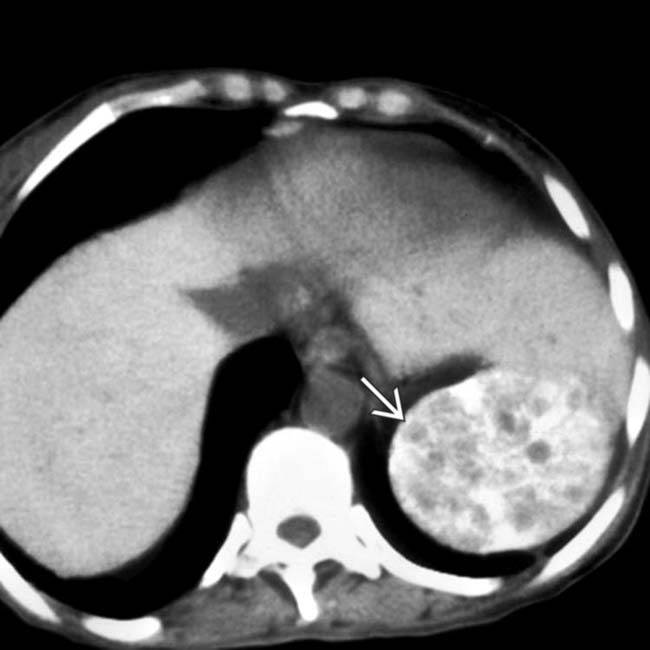
 in the spleen, representing massive splenic infarction, an uncommon complication that rarely results in the formation of a splenic abscess.
in the spleen, representing massive splenic infarction, an uncommon complication that rarely results in the formation of a splenic abscess.IMAGING
General Features
CT Findings
• Spleen
• Extramedullary hematopoiesis: May have many different manifestations, including paravertebral soft tissue masses (homogeneous soft tissue density), hepatosplenomegaly, or perinephric soft tissue “rind” encasing kidneys
MR Findings
• Persistence of red (cellular) marrow in bones with low-signal marrow on T1WI
 Demand for increased production of RBCs (due to RBC destruction and anemia) prevents normal conversion of red to yellow marrow
Demand for increased production of RBCs (due to RBC destruction and anemia) prevents normal conversion of red to yellow marrow
 Demand for increased production of RBCs (due to RBC destruction and anemia) prevents normal conversion of red to yellow marrow
Demand for increased production of RBCs (due to RBC destruction and anemia) prevents normal conversion of red to yellow marrowPATHOLOGY
General Features
• Genetics
 Sickle trait results when patient has only 1 abnormal sickle cell gene (30-40% of cases)
Sickle trait results when patient has only 1 abnormal sickle cell gene (30-40% of cases)
 Some patients may have 1 copy of sickle cell hemoglobin gene and 1 copy of another abnormal hemoglobin molecule (such as β-thalassemia)
Some patients may have 1 copy of sickle cell hemoglobin gene and 1 copy of another abnormal hemoglobin molecule (such as β-thalassemia)
 Sickle trait results when patient has only 1 abnormal sickle cell gene (30-40% of cases)
Sickle trait results when patient has only 1 abnormal sickle cell gene (30-40% of cases)
 Some patients may have 1 copy of sickle cell hemoglobin gene and 1 copy of another abnormal hemoglobin molecule (such as β-thalassemia)
Some patients may have 1 copy of sickle cell hemoglobin gene and 1 copy of another abnormal hemoglobin molecule (such as β-thalassemia)
CLINICAL ISSUES
Presentation
• Most common signs/symptoms
 Acute, painful vasoocclusive crisis (may occur several times each year)
Acute, painful vasoocclusive crisis (may occur several times each year)
 Acute, painful vasoocclusive crisis (may occur several times each year)
Acute, painful vasoocclusive crisis (may occur several times each year)

 of the right lower pole calyx with contrast extravasation
of the right lower pole calyx with contrast extravasation  (“golf ball-on-tee” appearance) within the papilla of the right lower pole calyx, consistent with papillary necrosis.
(“golf ball-on-tee” appearance) within the papilla of the right lower pole calyx, consistent with papillary necrosis.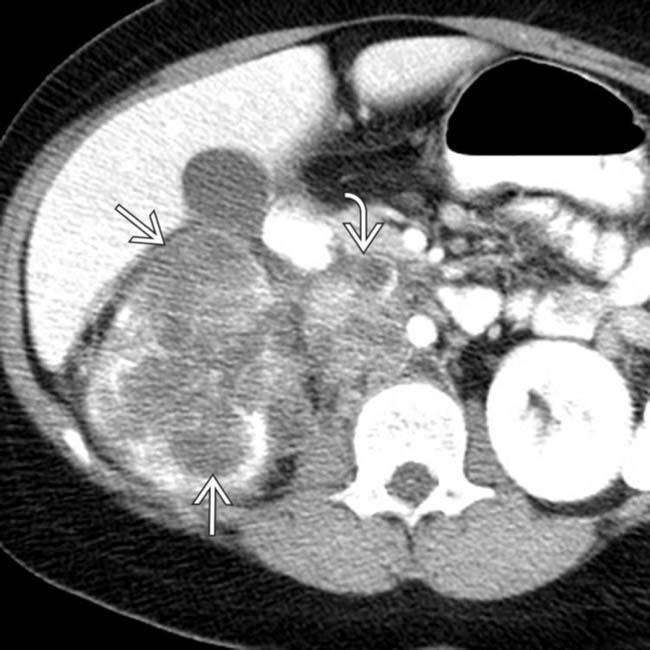
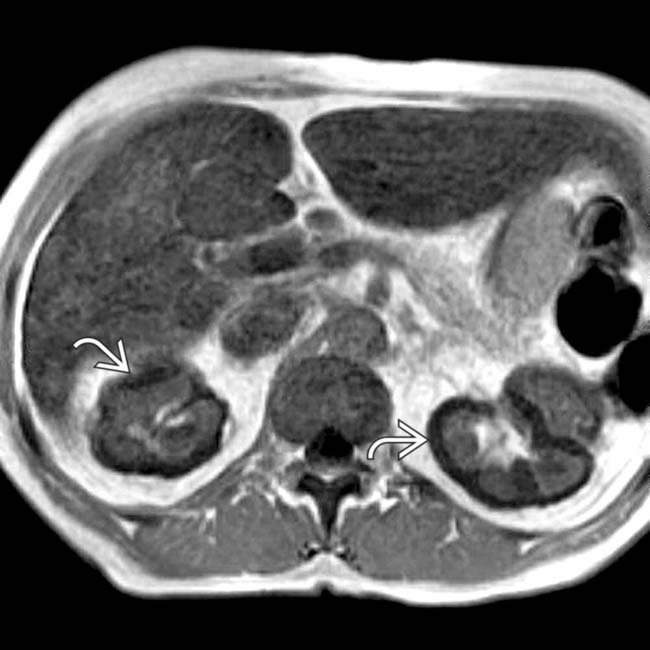
 in the right kidney with adjacent lymphadenopathy
in the right kidney with adjacent lymphadenopathy  . This was found to represent a renal medullary carcinoma.
. This was found to represent a renal medullary carcinoma.
 associated with sickle cell disease. Note the presence of sclerosis in the femoral head
associated with sickle cell disease. Note the presence of sclerosis in the femoral head  , compatible with avascular necrosis. This patient required a total left hip replacement 3 months later.
, compatible with avascular necrosis. This patient required a total left hip replacement 3 months later.

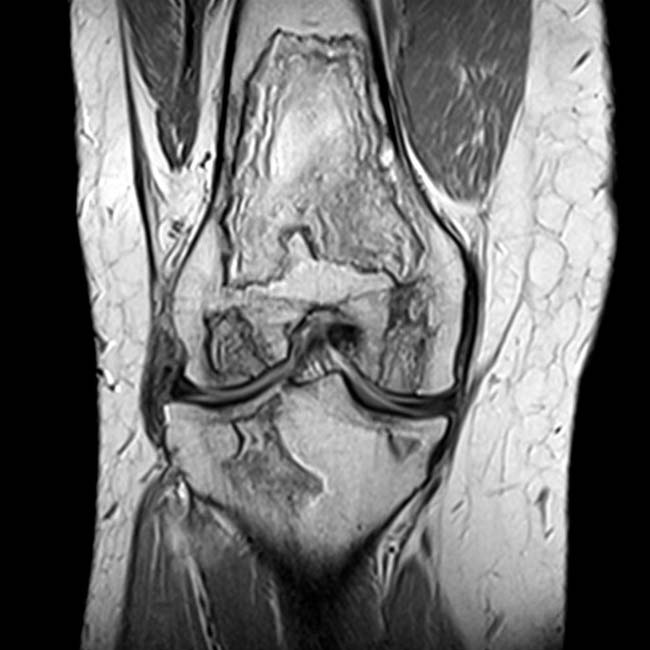
 in the distal femur and proximal tibia. Affected areas show a characteristic double-line sign with adjacent hyperintense and hypointense rims around their margins, characteristic of a bone infarct.
in the distal femur and proximal tibia. Affected areas show a characteristic double-line sign with adjacent hyperintense and hypointense rims around their margins, characteristic of a bone infarct.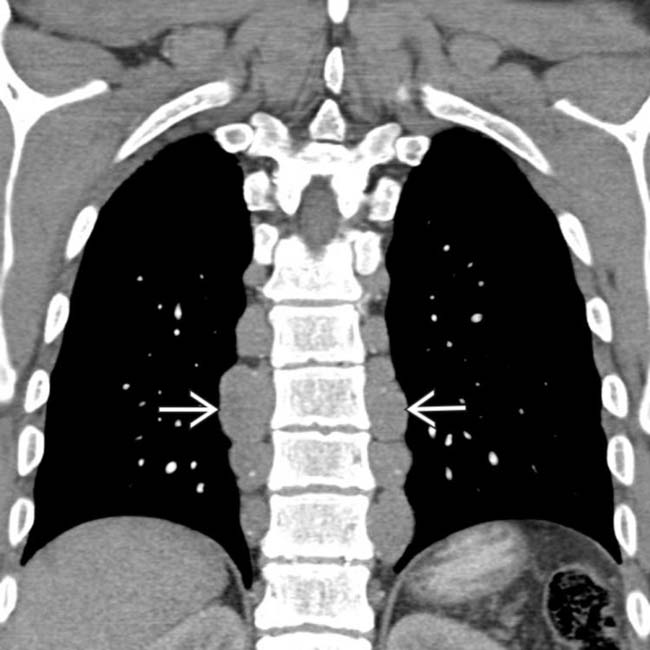
 , a characteristic appearance of extramedullary hematopoiesis.
, a characteristic appearance of extramedullary hematopoiesis.
 within the medial femoral condyle, consistent with a bone infarct.
within the medial femoral condyle, consistent with a bone infarct.
 and an area of high signal without bony sclerosis in the lateral femoral condyle
and an area of high signal without bony sclerosis in the lateral femoral condyle  , indicating a more acute infarct. Note the associated high-signal joint effusion
, indicating a more acute infarct. Note the associated high-signal joint effusion  .
.
 , and the lack of recognizable splenic tissue
, and the lack of recognizable splenic tissue  .
.
 , which is attributed to the deposition of hemosiderin within the proximal convoluted tubules.
, which is attributed to the deposition of hemosiderin within the proximal convoluted tubules.
 thought to be due to acute pulmonary hemorrhage from pulmonary infarcts related to sickle cell disease.
thought to be due to acute pulmonary hemorrhage from pulmonary infarcts related to sickle cell disease.





























































































