W6 Capsular Shrinkage in the Treatment of Wrist Instability
Basic Science
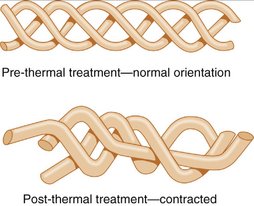
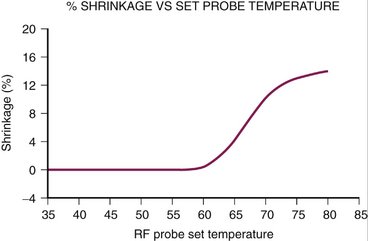
Capsular shrinkage was used by Hippocrates 2400 years ago to stabilize dislocated shoulders. More recently (comparatively speaking), the biology of capsular shrinkage has been extensively studied in animal models. These studies have shown that the triple helix of collagen “unwinds” and “shrinks” when heated to 60°C, maximum shrinkage being achieved between 65°C and 75°C (Figs. W6-1 and W6-2). The hydrogen bonds maintaining the three-dimensional configuration of the type I collagen triple helix rupture as the collagen is heated to greater than 60°C. The denatured collagen can potentially shorten to 50% of the resting length of the untreated collagen. The shortened denatured collagen acts as scaffolding onto which new collagen is deposited.1 The new collagen fibers maintain this shortened conformation, ensuring the long-term maintenance of the shortening.
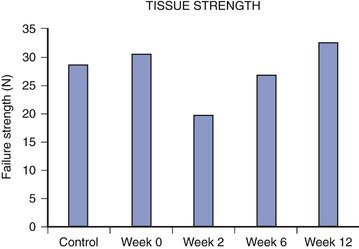
Biomechanical studies have shown that the tensile strength of heated collagen decreases rapidly and does not return to normal values for 12 weeks.2 The tensile strength returns to nearly 80% normal by 6 weeks after heating (Fig. W6-3). This transient loss of tensile strength would suggest that the application of stress to recently heated collagen is contraindicated. Premature loading of the shrunken collagen would lead to a lengthening of the collagen; this has been verified in an animal model.3,4 Based on these data, it would seem reasonable to recommend at least 6 to 8 weeks of joint immobilization after capsular shrinkage. Heavy loading of the joint should be avoided for 12 weeks.
Technique
General Information
Shrinkage requires very low energy settings. The radiofrequency (RF) devices must be adjusted to heat the tissue to a temperature of 65°C to 75°C. It is wise to start at low energy and slowly increase the energy output until the desired shrinkage is observed. If a laser is used, it should be set to very low energy (i.e., 0.2 to 0.5 J at 15 pulses per second [3 to 7.5 W]). The laser is held away from the target ligament and slowly advanced until the ligament is seen to shrink. When the shrinkage has stopped, continued heating further weakens the ligament only without increasing the shrinkage. The color of the ligament changes from white to light yellow during the shrinkage. Lu and associates5 suggested that a cross-hatching shrinkage pattern optimizes the ingrowth of healthy tissue and hastens the recovery of the ligament. During the shrinkage, the traction on the wrist should be reduced as much as possible to permit optimal shrinkage.
Scapholunate Instability
The question is what should or can be shrunk to stabilize the scapholunate axis? The scapholunate interosseous ligament is a heterogeneous structure. Its central portion is composed of fibrocartilage, which is not shrinkable (Fig. W6-4). The dorsal and palmar portions of the scapholunate ligament are composed of type I collagen and are shrinkable (Fig. W6-5). The arthroscope and thermal wand can be placed in either the 3,4 or 4,5 portals. The 70-degree side-firing laser probe and 90-degree RF probe can be placed in the 4,5 portal, while the scope is placed in the 3,4 portal. If the 0-degree probes are used, the scope should be placed in the 4,5 portal, while the wand is passed through the 3,4 portal. Extreme caution is exercised to avoid injury to normal hyaline cartilage. Good fluid inflow and outflow are crucial because the arthroscopy fluid removes the excess thermal energy generated by the probes.
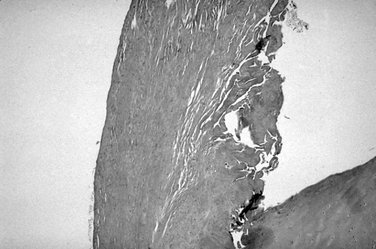
FIGURE W6-4 Histology of central fibrocartilaginous portion of the scapholunate ligament.
(From Berger RA: Ligament anatomy. In Cooney WP, Lilnscheid RL, Dobyns JH, eds: The Wrist: Diagnosis and Operative Treatment. St. Louis: Mosby, 1998.)
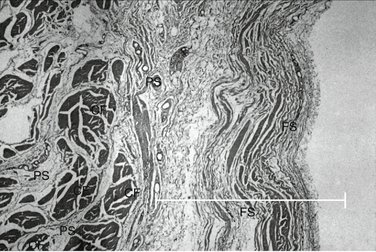
FIGURE W6-5 Histology of capsule showing loose collagen (CF) in a fibrous stratum (FS).
(From Berger RA: Ligament anatomy. In Cooney WP, Lilnscheid RL, Dobyns JH, eds: The Wrist: Diagnosis and Operative Treatment. St. Louis: Mosby, 1998.)
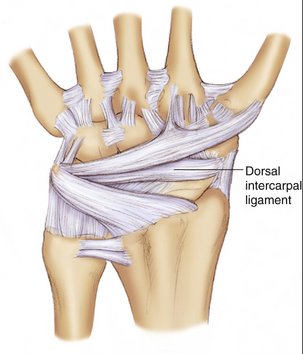
Capsular shrinkage of the dorsal intercarpal ligament could potentially reinforce the stabilizing effect of scapholunate ligament shrinkage. The dorsal intercarpal ligament is attached to the distal dorsal aspect of the scaphoid and the dorsal triquetrum (Fig. W6-6).6,7 Shrinkage of this ligament could simulate the tensioning of this ligament noted during open capsulodesis.8 To accomplish this, the scope and laser/RF angled probes would be placed in the radial and ulnar midcarpal portals. Alternatively, the scope can be placed in the midcarpal joint via the radial midcarpal volar portal described by Slutsky,9 while the thermal probes are passed through the ulnar midcarpal portal.
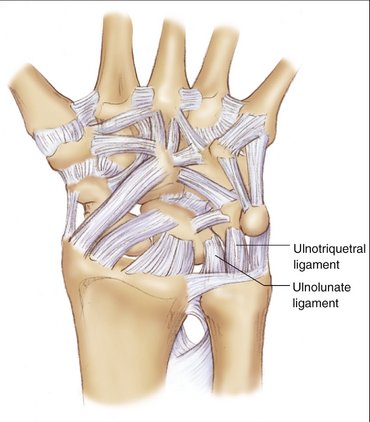
Lunotriquetral and Ulnocarpal Instability
Mild forms of lunotriquetral instability can be treated with ulnocarpal ligament shrinkage. I have applied this technique in a few cases with satisfying results. This procedure takes advantage of the anatomy of the ulnotriquetral and ulnolunate ligaments. These ligaments form a “V” as they diverge from their origin on the palmar distal radioulnar ligament and insert on the palmar aspect of the lunate or triquetrum (Fig. W6-7). As the ligaments are shrunk, the arms of the “V” shorten and approximate the lunate to the triquetrum, stabilizing the lunotriquetral joint. This stabilization can be reinforced further with the shrinkage of the lunotriquetral interosseous ligament. The lunotriquetral ligament histology is similar to that of the scapholunate ligament and can undergo dorsal and palmar, but not central, shrinkage. Isolated ulnocarpal ligament instability also can be treated with ulnocarpal ligament shrinkage. Ulnocarpal shrinkage is accomplished with the arthroscope in the 3,4 portal and the laser in the 4,5 or 6U portals.
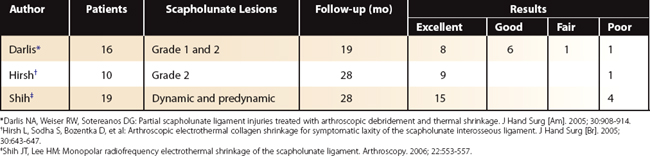
Results
Only a few capsular shrinkage clinical trials have been reported. Table W6-1 lists three such trials. They all deal with the treatment of mild scapholunate instability. They all suggest that capsular shrinkage has been very helpful for most patients treated.
There are no clinical studies reporting the outcome of capsular shrinkage for lunotriquetral or ulnocarpal instability. I have found ulnocarpal ligament shrinkage for ulnocarpal ligament laxity, mild triangular fibrocartilage complex laxity, and mild lunotriquetral instability to be rewarding in the 12 patients so treated. Mason and Hargreaves have reported good results in 14 of 15 patients they treated for midcarpal instability using RF shrinkage.10 I have used shrinkage to treat mild midcarpal instability in four cases. All patients are better, although one still has symptoms when she applies heavy stress to the wrist.
1. Lopez MJ, Hayashi K, Vanderby R Jr, et al. Effects of monopolar radiofrequency energy on ovine joint capsular mechanical properties. Clin Orthop. 2000;374:286-297.
2. Hecht P, Hayashi K, Lu Y, et al. Monopolar radiofrequency energy effects on joint capsular tissue: potential treatment for joint instability: an in vivo mechanical, morphological, and biochemical study using an ovine model. Am J Sports Med. 1999;27:761-771.
3. Naseef GS3rd, Foster TE, Trauner K, et al. The thermal properties of bovine joint capsule: the basic science of laser- and radiofrequency-induced capsular shrinkage. Am J Sports Med. 1997;25:670-674.
4. Hayashi K, Markel MD. Thermal capsulorrhaphy treatment of shoulder instability: basic science. Clin Orthop. 2001;390:59-72.
5. Lu Y, Hayashi K, Edwards RB3rd, et al. The effect of monopolar radiofrequency treatment pattern on joint capsular healing: in vitro and in vivo studies using an ovine model. Am J Sports Med. 2000;28:711-719.
6. Mitsuyasu H, Patterson RM, Shah MA, et al. The role of the dorsal intercarpal ligament in dynamic and static scapholunate instability. J Hand Surg [Am]. 2004;29:279-288.
7. Viegas SF, Yamaguchi S, Boyd NL, et al. The dorsal ligaments of the wrist: anatomy, mechanical properties, and function. J Hand Surg [Am]. 1999;24:456-468.
8. Szabo RM, Slater RR Jr, Palumbo CF, et al. Dorsal intercarpal ligament capsulodesis for chronic, static scapholunate dissociation: clinical results. J Hand Surg [Am]. 2002;27:978-984.
9. Slutsky DJ. Clinical applications of volar portals in wrist arthroscopy. Tech Hand Upper Extrem Surg. 2004;8:229-238.
10. Mason WTM, Hargreaves DG. Arthroscopic thermal capsulorrhaphy for palmar instability. J Hand Surg [Br]. 2007;32:411-416.