SHOULDER
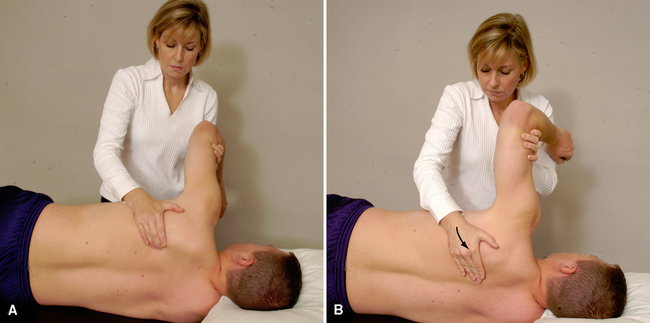
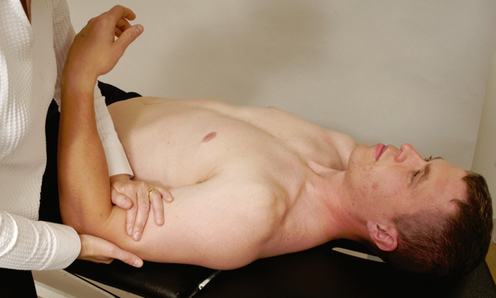
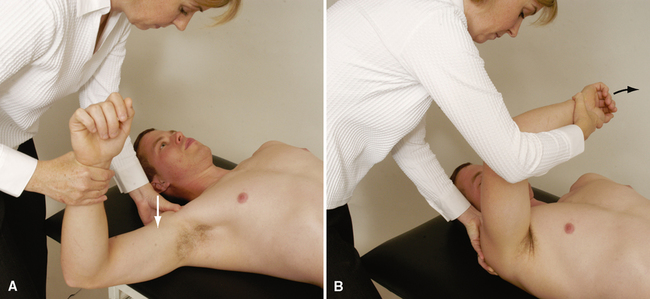
SPECIAL TESTS FOR ANTERIOR GLENOHUMERAL INSTABILITY27–37
General Information
Suspected Injury
• Unidirectional anterior instability.
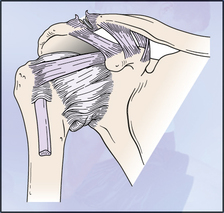
• If the instability is the result of anterior dislocation or subluxation, injuries that may be present include a Hill-Sachs lesion, fracture of the anterior glenoid rim, or a Bankart lesion.
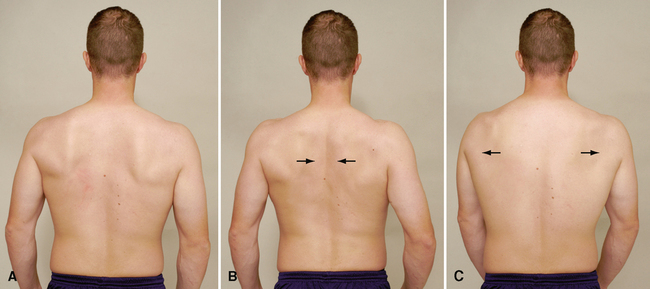
• Incorrect forward head posture, with rounded shoulders and protracted scapulae.
• Any of the peripheral nerves arising from the brachial plexus could be compromised. Damage can range from minor numbness or tingling to complete palsy of the nerve. The axillary nerve is especially susceptible.
• Anterior laxity often is accompanied by damage to the labrum, glenoid, anterior capsule, and/or brachial plexus.
• Vascular damage can occur with a shoulder dislocation. The brachial artery may be injured as it runs through the anterior shoulder complex.
Epidemiology and Demographics
Athletes who play overhead sports (e.g., tennis, volleyball, baseball) and patients with a history of dislocations or subluxations are more likely to have anterior shoulder instability. Several factors make the younger athlete more susceptible to anterior shoulder instability, such as poor technique and inadequate strength. Some researchers speculate that, in addition, adolescents’ immature collagen makeup makes them more susceptible to anterior shoulder instability and laxity.37
A wide array of incidences has been proposed in studies on anterior shoulder instability. Most patients initially dislocate the shoulder in their 20s or 30s, and 85% to 95% of dislocations in the shoulder are anterior. One fourth of all patients with dislocations have a family history of the same problem. The patient’s age at the time of dislocation has a significant impact on the recurrence rate. Reported recurrence rates in patients younger than age 20 vary from 70% to 100%.37
Relevant Signs and Symptoms
Translational Instability
• The patient may complain of generalized or anterior shoulder pain that can radiate down into the deltoid region of the shoulder, especially when the arm is above shoulder height.
• The patient may also complain of weakness in the shoulder that may be accompanied by clicking or grinding with shoulder motion.
• The patient often has a subjective feeling of instability, dislocation, or apprehension.
• The patient may complain that the shoulder does not “feel right,” especially when it is loaded above shoulder height.
• The results of unloaded active and passive movement and/or resisted isometric testing in neutral may be normal.
• Sensory loss, numbness or tingling, weakness, or complete palsy within a peripheral nerve distribution may be present in some cases.
• Coldness or weakness may be present if the vascular structures are compromised through the brachial region.
End-Range Instability
• Severe pain and restricted ROM are noted with dislocation.
• Severe muscle spasm may be present.
• The arm is held in 20º of abduction.
• Loss of shoulder roundness is seen.
• The humeral head may be palpated in the axilla.
• Once the dislocation has been reduced or if it has previously subluxed, apprehension predominates over pain.
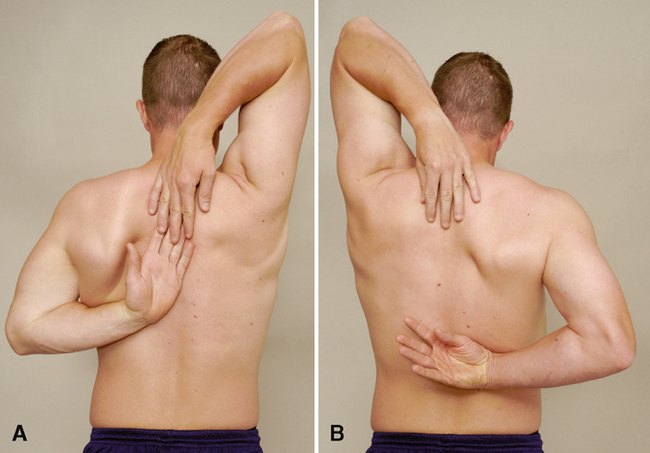
• In individuals under age 35, anterior shoulder instability is commonly associated with scapular instability and a tight posterior capsule, both of which must be addressed for successful treatment.
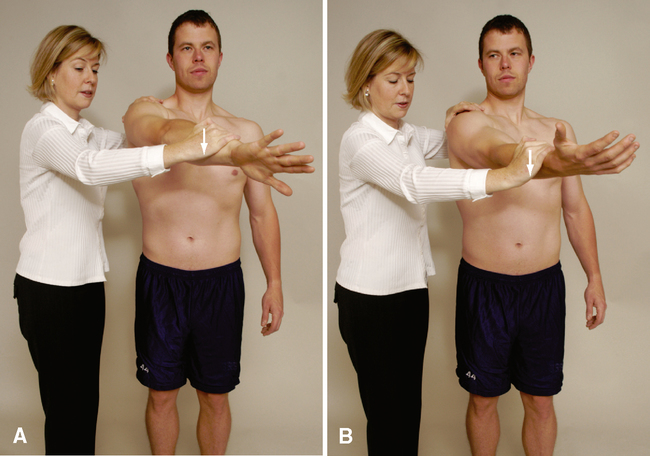
SPECIAL TESTS FOR POSTERIOR GLENOHUMERAL INSTABILITY
Relevant Special Tests
Epidemiology and Demographics
Recurrent posterior instability of the glenohumeral joint is less common than anterior instability. The frequency of occurrence is less than 5% of shoulder dislocations in most series.63 Other studies report that the rate of incidence is 2% to 12% of all cases of shoulder instability.64
Relevant Signs and Symptoms
• The patient may complain of generalized or posterior shoulder pain that may radiate down into the deltoid region of the shoulder.
• The patient may complain of weakness in the shoulder that may be accompanied by clicking or grinding with shoulder motion.
• Neural irritation is not common with posterior shoulder instability.
• The patient often has subjective feelings of instability, dislocation, or apprehension.
• The patient may complain that the shoulder “doesn’t feel right,” especially when it is loaded above shoulder height.
• The results of unloaded active and passive movement and resisted isometric testing may be normal.
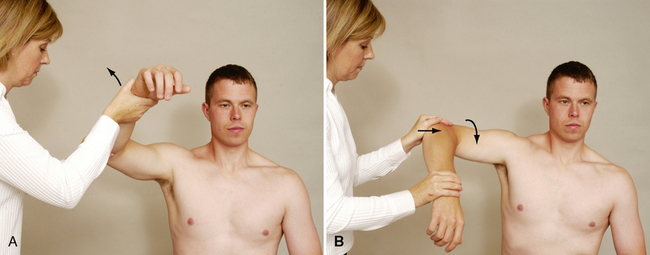
SPECIAL TESTS FOR INFERIOR GLENOHUMERAL INSTABILITY
Relevant Special Tests
Epidemiology and Demographics
Athletes who play overhead sports (e.g., tennis, volleyball, baseball) and patients with a history of dislocations or subluxations are more likely to have multidirectional instability of the shoulder. Several factors make the younger athlete more susceptible to multidirectional shoulder instability. Younger athletes have a tendency to have poor shoulder mechanics (incorrect techniques) and inadequate strength. In addition, some researchers speculate that adolescents’ immature collagen makeup leaves them more susceptible to shoulder instability and laxity.37,70–77
Relevant Signs and Symptoms
• The patient may have subjective feelings of instability, dislocation, or apprehension.
• The patient may complain that the shoulder “doesn’t feel right,” especially when it is loaded above shoulder height.
• Test results with unloaded active and passive movement and resisted isometric testing may be normal.
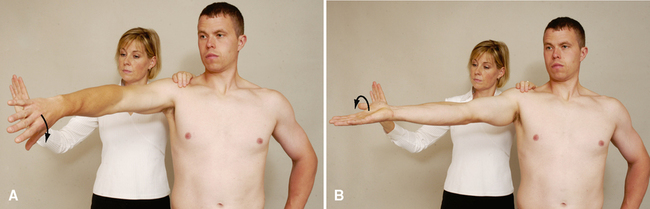
SPECIAL TESTS FOR IMPINGEMENT
Relevant Special Tests
Epidemiology and Demographics83
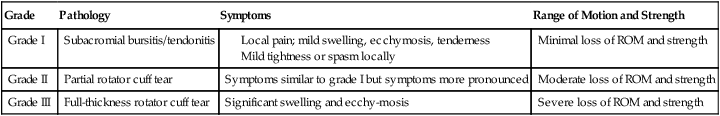
Neer has described three stages of impingement (Table 4-2).
Table 4-2
Neer’s Grades of Shoulder Impingement83
| Grade | Pathology | Symptoms | Range of Motion and Strength |
| Grade I | Subacromial bursitis/tendonitis |
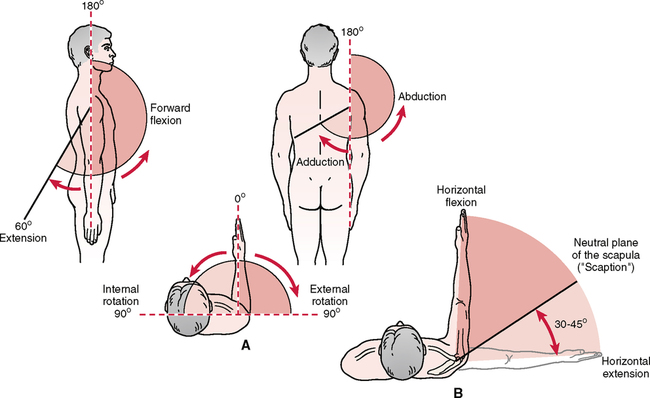
Mechanism of Injury84–88
Anterior shoulder impingement. Regardless of its cause (e.g., pathological condition of the rotator cuff, bicipital paratenonitis/tendinosis, scapular or humeral instability, labral pathology), anterior shoulder impingement most commonly results when structures are compressed in the anterior aspect of the humerus between the head of the humerus and the coracoid process, under the acromion process and under the coracoacromial ligament. These injuries may be acute or degenerative. An acute injury produces a sudden onset of shoulder pain after a specific activity. The aggravating activity commonly is an overhead maneuver, such as throwing or painting. Trauma, such as a fall onto an outstretched hand (FOOSH injury), also can result in shoulder impingement. Because of the progressive nature of subacromial impingement, patients with degenerative-type impingement often complain of several bouts of shoulder pain over a number of years. Each subsequent episode generally is worse than the previous one. The patient often reports that the latest episode did not resolve and has increasing loss of ROM.
Posterior shoulder impingement. Posterior impingement occurs when the rotator cuff impinges against the posterosuperior edge of the glenoid when the arm is abducted, extended, and laterally rotated. The result is a “kissing” labral lesion posteriorly. The resulting impingement occurs between the rotator cuff and greater tuberosity on one side and the posterior glenoid and labrum on the other side. This type of impingement often accompanies anterior instability or pseudolaxity, and deltoid activity increases to compensate for weakened rotator cuff muscles.
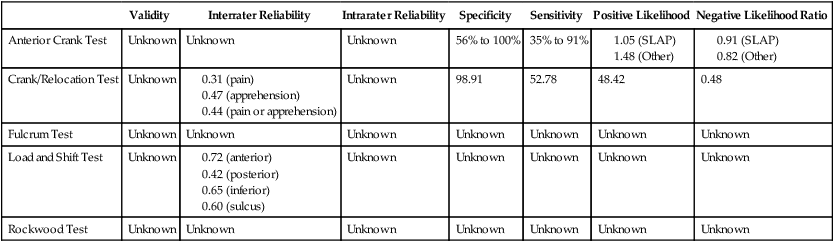
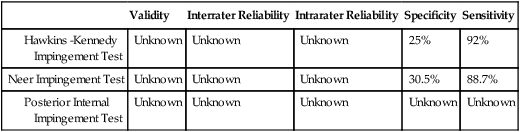
RELIABILITY/SPECIFICITY/SENSITIVITY/COMPARISON89
| Validity | Interrater Reliability | Intrarater Reliability | Specificity | Sensitivity | |
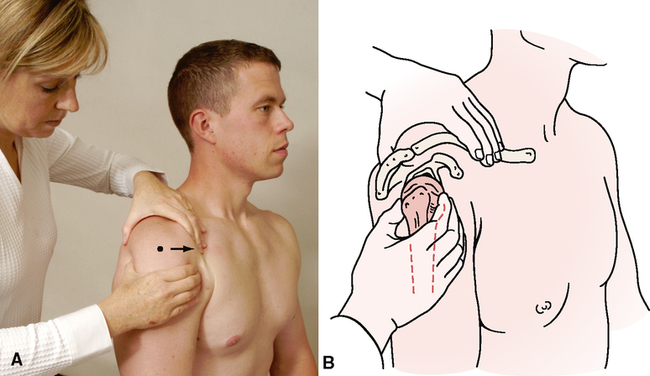
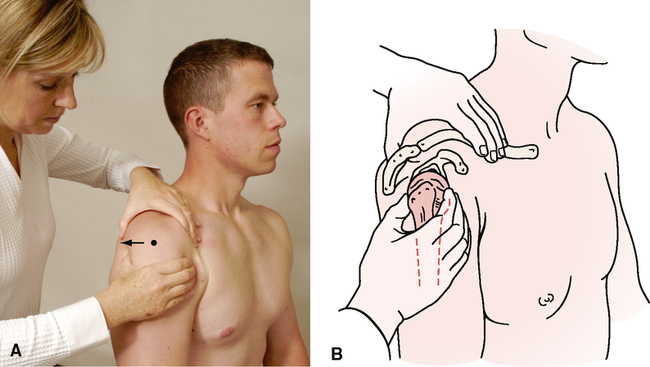
SPECIAL TESTS FOR LABRAL TEARS OF THE GLENOHUMERAL JOINT
Relevant Special Tests
Note: Parentis et al.107 concluded that no one test can provide a definitive diagnosis of a labral lesion.
Epidemiology and Demographics
The most common cause of a labral tear is trauma from a dislocation. In addition, younger individuals are prone to labral injury with repetitive overhead motions, such as swimming, tennis, or throwing. Older people are more prone to degenerative lesions, which often are associated with poor vascular supply to the labral tissue.54,74,108,109
Relevant Signs and Symptoms
• Aching of the shoulder region
• A feeling of instability may be noted by the patient
• Clicking or popping with motion
• Catching in the shoulder with movement
• Weakness or pain (or both) with overhead motions
• Diffuse upper trapezius or thoracic pain (or both)
Clinical Note/Caution
• Diagnosis of a SLAP lesion is based primarily on the history. The special tests are used to verify the suspected involvement of the labrum. The tests themselves should not be the sole source of diagnosis; they must correlate with the patient’s subjective complaints.
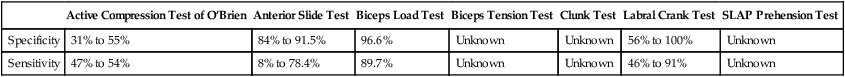
RELIABILITY/SPECIFICITY/SENSITIVITY COMPARISON27–29,110–112
| Active Compression Test of O’Brien | Anterior Slide Test | Biceps Load Test | Biceps Tension Test | Clunk Test | Labral Crank Test | SLAP Prehension Test | |
| Specificity | 31% to 55% | 84% to 91.5% | 96.6% | Unknown | Unknown | 56% to 100% | Unknown |
| Sensitivity | 47% to 54% | 8% to 78.4% | 89.7% | Unknown | Unknown | 46% to 91% | Unknown |