Sexually Transmitted Infections/Diseases
After reading this chapter, the student will be able to:
• Explain the difference in the terminology between sexually transmitted infections (STIs) and sexually transmitted diseases (STDs)
• Describe gonorrhea, syphilis, and chlamydia, and their incidence, symptoms, and treatment
• Describe the less common bacterial STIs including NGU, chancroid, and donovanosis
• Discuss the cause, prevention, and treatment of HIV and AIDS
• Discuss the cause, prevention, and treatment of hepatitis B, C, and D
• Describe the cause, prevention, and treatment of genital herpes and human papillomavirus infections
• Describe fungal STIs, their causative agents, and possible treatment
• Discuss the epidemiology of trichomoniasis
• Describe the complications that can occur with STIs and STDs
Introduction
Sexually transmitted infections/diseases (STIs/STDs) affect the same organs as the organs and structures covered in Chapter 16 (Infections of the Reproductive System). While affecting the same anatomical structures, the primary difference between infections of the reproductive system and sexually transmitted infections is the method of transmission. Sexual intercourse or any other sexual activity can lead to STIs, and eventually to STDs. Although the terms sexually transmitted infection and sexually transmitted disease are often used interchangeably, there is a distinction between the two. The term infection refers to just that, the presence of pathogenic organisms in a host, and symptoms of infection may be completely absent. The term disease refers to the appearance of symptoms and damaging effects as a result of an infection (see Chapter 9, Infection and Disease).
For the purpose of simplicity, STIs and STDs are referred to as STIs throughout this chapter. The organs that are affected by STIs in females are the ovaries, fallopian tubes, uterus, vagina, and external genitalia. In males the affected organs include the testes, prostate gland, urethra, and penis. Although reproductive organs are the primary targets, STIs may affect other organ systems and cause systemic problems. One of the likely reasons that sexual activity can lead to a high probability of STI transmission is the fact that most areas of the reproductive system are lined with mucous membranes, which are more susceptible to the penetration of pathogens than the skin (see Chapter 20, The Immune System). STIs can be caused by a variety of organisms including bacteria, fungi, viruses, and protozoa.
Bacterial Infections
Gonorrhea
Gonorrhea is the most reported STI in the United States.* The infection is caused by the bacterium Neisseria gonorrhoeae, a gram-negative diplococcus, and humans are the only known natural host. Once thought to be rather fragile and fastidious, not surviving for long periods of time outside of the host, research has recently discovered strains that are capable of surviving in dried pus on a bed sheet for 6 weeks. The organism can be transmitted through vaginal, anal, and oral sexual activity. The typical incubation time for the infection is between 2 and 7 days. Gonorrhea can be transmitted by individuals who are asymptomatic. Up to 40% of males and between 60% and 80% of females may be infected without any symptoms, but they can act as carriers for up to 5 to 15 years. A small number of organisms, in some cases only about 1000, is required to cause an infection. The symptoms of gonorrhea vary between males and females (Box 17.1). Besides infections of the genitals, oral and anal sexual activity can also lead to gonorrheal infections in the pharynx and the rectum, leading to general systemic bacteremia. Symptoms of systemic gonorrheal infections include the following:
• Skin lesions (Figure 17.1) that can move to the joints, causing arthritis

The lesions start as erythematous papules and often develop into necrotic, grayish central lesions surrounded by an erythematous base. (From Morse S, Ballard RC, Holmes KK, et al: Atlas of sexually transmitted diseases and AIDS, ed 3, St. Louis, 2003, Mosby.)
Gonorrhea increases the risks of other infections, including HIV and chlamydia. Men with prolonged infections may also develop an inflammation of the testicles called epididymitis, a condition often leading to infertility. Prolonged infections in women can result in pelvic inflammatory disease (see Chapter 16, Infections of the Reproductive System), which may include the uterus and fallopian tubes. Scar tissue in the fallopian tubes can prevent fertilization, and damage to the uterine wall can stop implantation of a fertilized ovum (zygote). Pelvic inflammatory disease also increases the risk of ectopic pregnancy.
During delivery gonorrhea can be passed from the infected mother to the baby as it moves through the birth canal (see Chapter 23, Human Age and Microorganisms). Infection of the newborn often leads to infection of the joints, blood infection (bacteremia), and/or blindness.
Syphilis
Syphilis has been in the human population for many years and is documented in many historical writings. Because it causes symptoms that can be associated with numerous other diseases, syphilis is sometimes referred to as the “great imitator.” It is caused by Treponema pallidum, a gram-negative spirochete. Humans are the organism’s only natural reservoir and transmission occurs through direct contact with sores of an infected person. Although the bacterium can be passed on through body fluids such as saliva, the primary means of transmission is through any sexual activity—vaginal, anal, or oral. A pregnant woman can also pass the infection on to her child during pregnancy. This infection is known as congenital syphilis (see Chapter 23, Human Age and Microorganisms).
Syphilis takes place in three stages, with an incubation time between 10 and 90 days after the initial infection. The initial symptoms may be mild and are sometimes difficult to diagnose because they resemble symptoms of other diseases such as gonorrhea. Many infected persons in the early stages do not realize that they are infected. If treated early, syphilis can be cured without any resulting serious or long-term health problems. Untreated, syphilis manifests itself in three stages: primary, secondary, and tertiary syphilis (Table 17.1).
TABLE 17.1
| Stage | Time Frame | Symptoms |
| Primary | Ten to 90 d after initial infection | Small, red skin sores |
| Secondary | Two to 10 wk after primary stage | Red-brown rash on palms of hands and soles of feet; fever, swollen lymph nodes, sore throat, muscle and joint pain, loss of patches of hair, malaise, rash on skin and mucous membranes of mouth, throat, and cervix |
| Latent | After secondary stage | None |
| Tertiary | Many years from onset of the latent phase | Gummas—rubbery masses of tissue in various organs; memory loss, ataxia, paralysis, insanity, and finally death |
• Primary syphilis represents itself as small, red sores (chancres) that appear on the body at the site of infection within 10 to 90 days after initial contact. These sores will eventually disappear, leaving a scar on the skin. if untreated, the symptoms will move to the secondary stage.
• Secondary syphilis occurs within 2 to 10 weeks of the primary stage (Figure 17.2). During this stage the organism enters the bloodstream and travels to other organ systems, causing a wide variety of symptoms including the following:
Without treatment at this point the disease will move into the tertiary stage:
• Tertiary syphilis is the final stage of the disease, characterized by gummas (lesions) that begin to affect vital organs including the eyes, liver, heart, kidneys, and the brain. This stage results in conditions such as:
Patients with syphilis in the later stages are also at increased risk for HIV infection.
Pregnant women run the risk of passing the infection on to their unborn child and they have an increased risk for miscarriage, premature delivery, and stillbirth (see Chapter 23, Human Age and Microorganisms). Diagnosis of syphilis can be done by a number of different methods. Observing a sample from a lesion for the organism itself, using a dark-field microscope, is typically one of the first methods used for early detection. Along with microscopic examination, a number of blood-screening tests are available to confirm an infection. These include the following:
Chlamydia
Although usually referred to simply as chlamydia, the organism Chlamydia trachomatis, a gram-negative coccus and an intracellular obligate parasite, is responsible for a number of different infections of the reproductive system. These include nongonococcal urethritis (NGU), pelvic inflammatory disease (PID), and lymphogranuloma venereum (LGV). Chlamydial infections are now the most prevalent STIs in the United States (Box 17.2). Female carriers of the infection are often asymptomatic, thus increasing the transmission of chlamydial infections. Transmission occurs through exchange of semen or vaginal fluid during vaginal, oral, or anal sexual activity. Pregnant women can also pass the infection on to their child during labor and delivery. The incubation period is between 1 and 3 weeks before symptoms appear. The symptoms of a chlamydial infection tend to be very mild or virtually nonexistent. According to research data, up to 75% to 80% of infected women and up to 50% of infected men show no symptoms at all.
Left untreated, chlamydial infections can cause serious health problems in both men and women. In males the infection can lead to epididymitis, possibly resulting in sterility and other complications. Furthermore, in males an NGU chlamydial infection may manifest itself as urethritis (see Urinary Tract Infections in Chapter 15, Infections of the Urinary System) and in women as vulvovaginitis or cervicitis (inflammation of the cervix). Women are more likely to experience serious problems associated with a chlamydial infection in the form of PID (see Chapter 16, Infections of the Reproductive System). LGV chlamydial infections are 20 times more common in men than in women. The lesions characteristic of this type of infection usually heal on their own; however, 1 week to 2 months after the lesions heal the organism invades the lymph nodes, causing large, painful buboes. If the buboes are not drained, inflammation can create obstructions in the lymph vessels, causing massive enlargement of the external genitalia in both males and females.
Mycoplasmal and Ureaplasmal Nongonococcal Urethritis (NGU)
Treatment for these infections is typically tetracycline; however, erythromycin, spectinomycin, and clindamycin have also proven to be effective. Because of the lack of a cell wall, penicillin is not effective against these microbes (see Chapter 22, Antimicrobial Drugs). Preventive measures against these NGU infections include simply abstinence from sexual activity or use of a condom.
Chancroid
Chancroid infection is relatively rare in the United States but its incidence worldwide may be greater than that of either gonorrhea or syphilis. The soft chancres (Figure 17.3) of this infection distinguish it from the hard lesions that are characteristic of syphilis. The causative agent is Haemophilus ducreyi, a short gram-negative bacillus. Humans are the host for this organism, and the method of transmission is vaginal sex. Incubation time between initial infection and the appearance of symptoms is about 3 to 7 days. This infection affects both men and women, with a much higher incidence of infection noted among men. The primary symptom is the appearance of soft, painful lesions or chancres. These chancres bleed easily and usually appear on the genitals or in the genital area 3 to 5 days after exposure. On occasion an infection will be present without the lesions, but a burning sensation after urination occurs. Chancres can also appear in the mouth or on the lips, but regardless of their location, they are highly infective. Simply touching a chancre with bare skin can result in transmission of the infection. In about 30% of cases the infection will move to the groin area, where it will form enlarged masses of lymphatic tissue, called buboes. Each bubo will then enlarge greatly and can break through the skin, discharging pus. Untreated lesions can persist for months, but the infection will often resolve without treatment.
Donovanosis (Granuloma Inguinale)
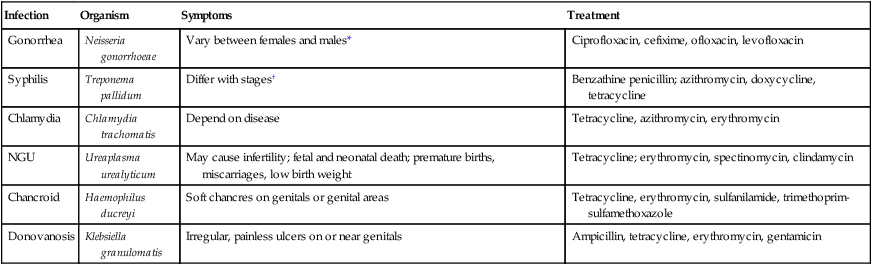
HEALTHCARE APPLICATION
Common Bacterial STIs
| Infection | Organism | Symptoms | Treatment |
| Gonorrhea | Neisseria gonorrhoeae | Vary between females and males* | Ciprofloxacin, cefixime, ofloxacin, levofloxacin |
| Syphilis | Treponema pallidum | Differ with stages† | Benzathine penicillin; azithromycin, doxycycline, tetracycline |
| Chlamydia | Chlamydia trachomatis | Depend on disease | Tetracycline, azithromycin, erythromycin |
| NGU | Ureaplasma urealyticum | May cause infertility; fetal and neonatal death; premature births, miscarriages, low birth weight | Tetracycline; erythromycin, spectinomycin, clindamycin |
| Chancroid | Haemophilus ducreyi | Soft chancres on genitals or genital areas | Tetracycline, erythromycin, sulfanilamide, trimethoprim-sulfamethoxazole |
| Donovanosis | Klebsiella granulomatis | Irregular, painless ulcers on or near genitals | Ampicillin, tetracycline, erythromycin, gentamicin |
Viral Infections
HIV and AIDS
The human immunodeficiency virus (HIV) is the causative agent of acquired immune deficiency syndrome (AIDS), a secondary immune deficiency (see Chapter 20, The Immune System). AIDS is not a disease but a syndrome because it has complex signs and symptoms, and a variety of diseases are associated with a common cause. AIDS results in many opportunistic infections due to a severely compromised immune system.
HIV infection in humans is now a pandemic, that is, an infection that occurs worldwide. There are at least two types of the virus, HIV-1 and HIV-2, that are responsible for causing AIDS (discussed in Chapter 20). The HIV virus basically destroys the immune system, thus leaving the body open to various infections that ultimately prove fatal. The virus targets cells of the immune system including helper T cells, macrophages, dendritic cells, and Langerhans cells. As these components of the immune system battle the virus in the early stages of infection the virus survives but may be kept in check, and the result can be almost a draw between the body and the virus. However, over time the body’s ability to replace the cells of the immune system will be diminished and unable to keep up with the rapidly replicating, and usually mutating virus. Without the helper T cells and macrophages the B cells will not be stimulated to form plasma cells, which are responsible for producing the antibodies to fight the infection (see Chapter 20). A count of the helper T cells is a good indicator in predicting the progression of the infection and the onset of AIDS-related symptoms. The progression of HIV infections depends primarily on two factors: the actual amount of virus a person was exposed to, and how often repeated exposure occurred. According to the Centers for Disease Control and Prevention (CDC, Atlanta, GA) the stages of HIV infections are classified into four groups or stages (Table 17.2).
TABLE 17.2
Stages of HIV Infections and AIDS
| Stage | Time Frame | Symptoms |
| 1 | 1–12 mo | HIV antibodies appear; flulike symptoms |
| 2 | 1–8 yr | Mild anemia, low white blood cell count, some decrease in T cell count, seborrheic dermatitis, shingles, hairy leukoplakia |
| 3 | 9–15 yr | Moderate anemia, low albumin, low cholesterol, decrease in helper T cell count, severe dermatitis, thrush, weight loss, diarrhea, recurring fever, tuberculosis, various bacterial infections, recurrent shingles |
| 4 | Months to years | Death—usually 2 yr after diagnosis in men, 12–18 mo in women. Causes of death vary, but usually involve opportunistic infections, lymphoma, and wasting syndrome |
• Sexual contact—all forms of sexual activity: Heterosexual and homosexual intercourse whether vaginal, anal, or oral
• Sharing contaminated needles between intravenous drug users
• Receiving any contaminated blood products
• Transfer from infected mother to infant either during the pregnancy, during delivery, or through breastfeeding
Diagnosis of HIV infections can include the following methods:
• Enzyme-linked immunosorbent assay (ELISA): This is typically the first step in HIV testing, which detects the presence of HIV antibodies in a sample of blood. If positive, the second step will be a confirmation test. If negative, testing stops here. This is the U.S. Food and Drug Administration (FDA)-approved method for detecting HIV infections.
• Western blot is used to confirm the positive ELISA results. This test involves detection of specific proteins present in the blood of an HIV-positive patient. Combined with the ELISA, a positive result with the Western blot is 99.9% accurate. This test is FDA approved for detecting an HIV infection.
• HIV polymerase chain reaction (HIV PCR) is used to detect the presence of specific DNA and RNA sequences that indicate the presence of HIV as the viral DNA/RNA circulate in the blood after infection has occurred. This test is FDA approved for detecting an HIV infection.
• OraSure is a home-type test using secretions from between the cheek and the gums to detect the presence of HIV antibodies; this is in contrast to the blood used in the three previous tests. The principle is essentially the same as with the ELISA, but involves a different sample type. This test is not currently approved by the FDA for a definitive diagnosis of HIV infection.
• Urinanalysis is also used to detect an HIV infection but tends to be inaccurate in the present form. This test is not FDA approved for detecting an HIV infection.
The ELISA, Western blot, and PCR methods are discussed in detail in Chapter 25 (Biotechnology). There are a number of testing methods and protocols being developed to improve the speed and accuracy of the tests.
Hepatitis B, C, and D
Hepatitis is an infection of the liver, capable of causing significant destruction of liver cells (see Chapter 9 [Infection and Disease] and Chapter 12 [Infections of the Gastrointestinal System]). Hepatitis B, C, and D viruses can be transmitted during sexual activity and are therefore considered STIs although they do not specifically target or affect organs of the reproductive system.
• Hepatitis B (HBV) transmission occurs when blood from an infected person enters the body of another. It can be transmitted through sexual activities with an infected person, by sharing needles, and from infected mother during birth or by breastfeeding. Transmission has also been documented through artificial insemination with contaminated semen. Furthermore, transmission can occur through needlesticks or exposure to sharps. The incubation time is between 45 and 180 days, with an average of about 90 days. The virus itself replicates in liver cells, lymph tissue, and hematopoietic tissue. The virus may stay in the blood for years and be passed on by the carrier at any time. The symptoms of a HBV infection are not immediately obvious but once they do appear they include the following:
• Hepatitis C (HCV) in most cases is transmitted by blood-to-blood contact but may be sexually transmitted, especially among individuals already infected with another STI. Signs and symptoms of the infection are similar to those of hepatitis B infections. Hepatitis C can be either acute, that is, a short-term illness occurring within the first 6 months after exposure to the virus, or chronic. Seventy to eighty percent of acute infections will develop into a chronic infection, a serious disease that can result in long-term health problems, or even death. HCV RNA can be detected in the blood within 1 to 3 weeks of exposure, and antibodies to HCV can be detected in more than 97% of persons by 6 months after exposure. At present there is no vaccine available for hepatitis C and the CDC recommendations for prevention and control of HCV infections include screening and testing of blood donors, viral inactivation of plasma-derived products, risk reduction counseling, screening of persons at risk for HCV infection, and routine practice of infection control in healthcare settings.
• Hepatitis D (HDV) is caused by the hepatitis D virus, a defective virus that needs the hepatitis B virus to exist and therefore is found in the blood of persons infected with the HBV virus. HDV may worsen hepatitis B infection or existing hepatitis B liver disease. Symptoms of the infection are similar to those of HBV infections but may also include the following:
Genital Herpes
Genital herpes, a highly contagious and common STI in the United States, is caused by the herpes simplex virus HSV-2 or HSV-1. Although most genital herpes is caused by HSV-2, it can also be caused by HSV-1, the organism that most commonly causes “fever blisters” of the mouth and lips (see Chapter 10, Infections of the Integumentary System, Soft Tissue, and Muscle). Genital herpes infections typically result in one or more blisters on or around the genitals or rectum. After the blisters break they leave tender sores that take 2 to 4 weeks to heal. Other outbreaks may occur weeks or months thereafter, with the number of outbreaks generally decreasing over the years. The signs and symptoms of the infection vary greatly and some individuals infected with HSV-2 may not be aware of their infection. Even without clear signs and symptoms of the infection HSV can be detected by the use of blood tests, because of the presence of antibodies.
Neonatal herpes (see Chapter 23, Human Age and Microorganisms) is a condition of concern for women of childbearing age because the virus can cross the placenta and infect the fetus. Serious damage to the fetus may occur, including mental retardation and defective hearing and vision. Spontaneous abortions have also been reported. If the infection is acquired during the late stages of pregnancy a cesarean delivery is usually performed to protect the child.
Summary
• Sexually transmitted infections (STIs) and diseases (STDs) are the result of some type of sexual activity and affect both men and women, but can also affect the unborn child.
• STIs affect mostly the organs of the reproductive system, but depending on the infection can affect all systems of the human body.
• STIs can be caused by bacteria, viruses, fungi, and protozoans.
• The most common bacterial STIs are chlamydia, gonorrhea, and syphilis. Others include chancroid, mycoplasmal and ureaplasmal nongonococcal urethritis, and donovanosis.
• Most bacterial STIs can be treated with antibiotics. Damage to tissues and organs that occurs before treatment generally cannot be reversed.
• Viral STIs are as common as bacterial STIs but at the present time are incurable. Vaccination is available for some.
• The most common viral STIs include HIV, hepatitis B, C, and D, genital herpes, and human papillomavirus infections.
• Fungal STIs include candidal vaginitis, balanitis, and jock itch. These infections are not always sexually transmitted.
• Trichomoniasis is the only known STI transmitted by a protozoan.
• STIs are preventable but remain a major public health challenge worldwide and in the United States.
Review Questions
1. Which of the following organisms is the causative agent for gonorrhea?
2. Which of the following STIs is also referred to as the “great imitator”?
3. Gummas are characteristic lesions of:
4. The secondary stage of syphilis includes which of the following time periods after the primary stage:
5. Lymphogranuloma venereum is an infection caused by:
6. The causative agent for chancroid is:
7. The STI caused by Klebsiella granulomatis is:
8. A red-brown rash on the palms of the hands and soles of the feet is typical for:
9. Which of the following agents can be used in the treatment of balanitis?
10. Which of the following organisms can cause sexually transmitted toxic shock syndrome?
11. NGU is the abbreviation for __________.
12. Granuloma inguinale is also called __________.
13. HIV is the abbreviation for __________.
14. Vaccination is available for the sexually transmitted hepatitis __________ virus.
15. The only STI transmitted by a protozoan is __________.
16. Discuss and differentiate between the prevalence and incidence of STIs in the United States.
17. Describe the different symptoms of gonorrhea in males and females.
18. Explain the different stages of syphilis.
19. Describe the different stages of HIV infections and AIDS.



