http://evolve.elsevier.com/McCuistion/pharmacology
Each day, over 1 million new cases of sexually transmitted infection (STI) occur worldwide. The incidence of STIs has been increasing since 2013. Young adults are at risk, particularly young women, but infections among men are also rising. Over 30 bacteria, viruses, and parasites can cause STIs. The most common bacterial pathogens are Chlamydia, Neisseria gonorrhoeae, and Treponema pallidum (syphilis); Trichomonas is a common parasite; and the most common viral pathogens are hepatitis B virus (HBV), herpes simplex virus (HSV), human immunodeficiency virus (HIV), and human papillomavirus (HPV). The majority of persons with STIs experience few or no symptoms, making it difficult to diagnose and treat to stop the spread of infections. STIs are spread through sexual contact, via blood or blood products, and through mother-to-child transmission during pregnancy and childbirth.
Sexually Transmitted Infections
Sexual transmission of pathogens can occur through breaks in the vaginal or cervical mucosa or in the skin covering the shaft or glans of the penis. Each act of coitus results in tiny, friction-induced fissures on these surfaces. Seminal fluid, spermatozoa, vaginal secretions, blood, and other body fluids can carry pathogens. Skin and mucosal lesions can be penetrated by microorganisms, and skin and mucosa can shed microorganisms.
Sexual contact can involve transmission of pathogens through the skin or mouth and via oral-genital, oral-anal, or hand-anal transmission of pathogens through breaks in the skin or mucosal surfaces or from inoculation by infectious body fluids. Anal penetration is particularly risky because of the likelihood of tissue trauma that results in the partner’s exposure to enteric microorganisms. The risk for contracting an STI increases with substance abuse, imprisonment, sexual activity with a partner who has been imprisoned, sexual activity with individuals being paid for sex acts, and rape or sexual assault.
Patients who engage in sexual activity with multiple partners are at high risk for transmission of STIs, particularly HIV. The Centers for Disease Control and Prevention (CDC) reports the risk for getting STIs is markedly increased among individuals who have more than one sexual partner per year versus those who have fewer partners. It should be noted that 5.2% of men between the ages of 15 and 44 report having 5 or more partners in a 12-month period, and 2% of women report the same. Additionally, 21.8% of men between the ages of 15 and 44 report having had 15 or more sexual partners, and 10.6% of women report the same.
Other high-risk practices are anal or vaginal intercourse without a condom, hand-anal contact, contact with menstrual blood during sexual activity, use of an enema before anal intercourse, and urination on broken skin or inside the body. Refer to Fig. 54.1 for guidelines provided by the CDC on the prevention of STIs.
STIs are often manifested as multiple infections. Individuals undergoing treatment for one STI should be assessed for others, including HIV. This is especially true if genital or perianal ulcerations are present.
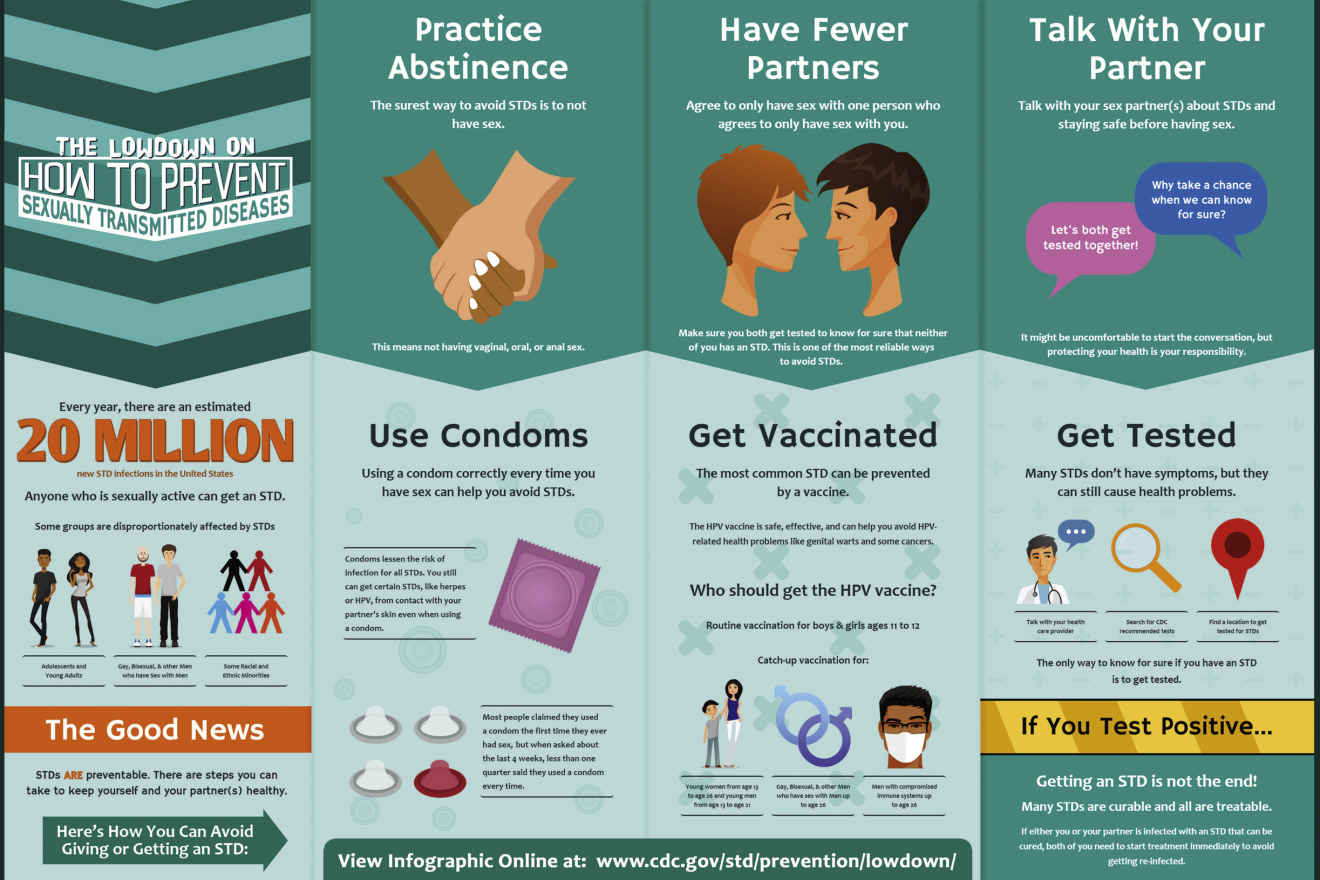
FIG. 54.1 How to Prevent Sexually Transmitted Infections.
From Centers for Disease Control and Prevention. (2016). How you can prevent sexually transmitted diseases. Retrieved from www.cdc.gov/std/prevention
Vertical transmission is the passage of infecting organisms from mother to neonate. Microbes can travel up the reproductive tract from the vagina or cervix and enter the intrauterine environment. Organisms that are of little consequence to healthy adults can be devastating to a fetus. Transmission can also occur through contact with the mother’s blood at birth or through breast milk, as in the case of HIV and HBV. Many STIs, such as syphilis, are transmitted through the placenta and membranes. Others, such as the herpes simplex virus type 2 (HSV-2), require actual contact by the infant with microorganisms in the birth canal. Because of the risk for blindness caused by Chlamydia trachomatis and N. gonorrhoeae, erythromycin ointment is routinely administered in the eyes of neonates as prophylaxis. This is usually done within the first hour after birth.
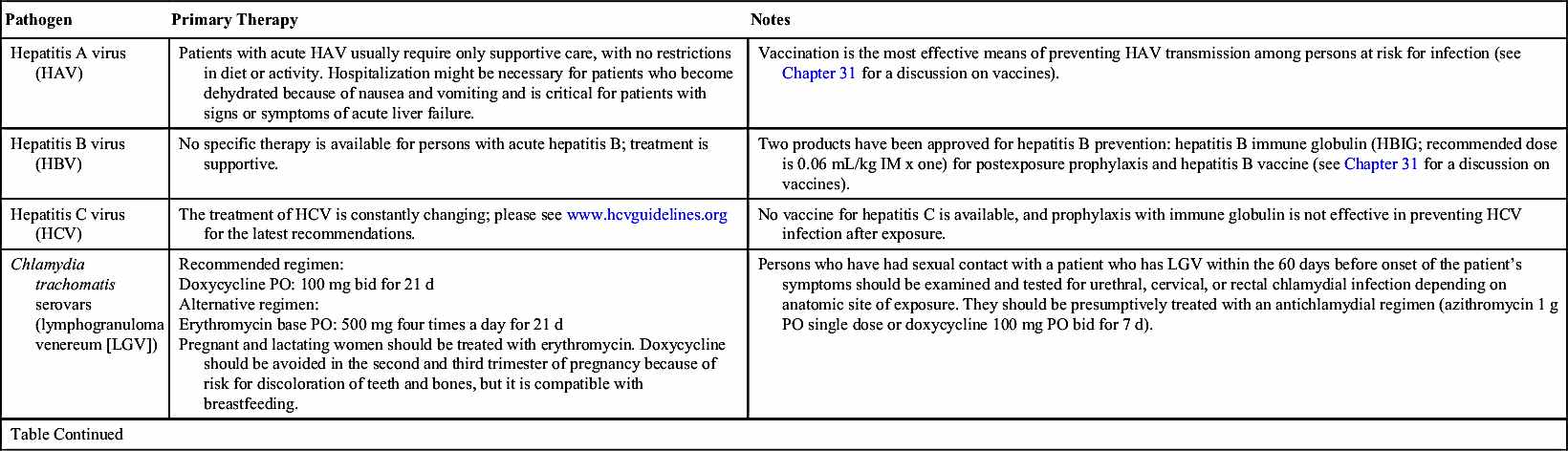
CDC guidelines for the primary treatment of some STI pathogens are listed in Table 54.1; the most common pathogens are discussed in the following section. All sexual contacts of an infected individual should be informed of the exposure so they can be treated. Partners should refrain from sexual activity until each is clear of infection on follow-up evaluation or, at the very least, condoms should be used until each is clear of infection.
Sexually Transmitted Pathogens
The information in this chapter comes directly from the 2015 treatment guidelines for sexually transmitted infections, available at www.cdc.gov/std/tg2015/default.htm.
Bacterial Pathogens
Sexually transmitted bacterial pathogens can be effectively treated with antibiotic therapy. When present, common symptoms include vaginal discharge, urethral discharge or burning (in men), genital ulcers, and abdominal pain.
Bacterial Vaginosis
Bacterial vaginosis (BV) causes a large amount of homogenous, thin, white vaginal discharge with a strong fishy odor. In BV, normal, healthy bacteria in the vagina—lactobacilli—are replaced with anaerobic bacteria, most commonly Gardnerella vaginalis, Mycoplasma hominis, Ureaplasma urealyticum, or Prevotella, Porphyromonas, Bacteroides, Peptostreptococcus, and Mobiluncus species. BV can be transmitted via sexual contact but is not considered an STI; however, having BV can increase a woman’s risk for getting an STI due to the imbalance in vaginal bacteria.
BV is treated with metronidazole 500 mg by mouth (PO) twice a day for 7 days. Because metronidazole can cause stomach upset, it should be taken with food or a full glass of water or milk. Alcohol causes severe nausea and vomiting when ingested with metronidazole, so patients should be instructed not to drink alcoholic beverages or use products that contain alcohol, such as mouthwash, for the duration of drug therapy and for 48 hours after treatment.
Vaginal preparations are also effective in treating BV, such as metronidazole gel 0.75%, one 5-g applicator intravaginally at bedtime for 5 nights; clindamycin cream 2%, one 5-g applicator intravaginally at bedtime for 5 days; or clindamycin ovules, 100 mg intravaginally at bedtime for 3 days.
Oral drugs that are alternatives to metronidazole include tinidazole, either 2 g orally once a day for 2 days or 1 g orally once a day for 5 days, or clindamycin 300 mg orally twice a day for 7 days. Tinidazole has the same precautions with alcohol as metronidazole and should be taken with food. Tinidazole causes slightly less gastrointestinal (GI) upset than metronidazole. Patients taking clindamycin should be instructed to notify their health care provider if diarrhea develops because it may be an indication of Clostridium difficile–associated diarrhea (CDAD). Treating BV is especially important for pregnant women because of the risk of spontaneous abortion, delivery of premature or low-birthweight babies, or pelvic infection developing after delivery. Metronidazole (oral or intravaginal) or clindamycin (oral) are the drugs of choice in pregnancy, and tinidazole should not be used during the first trimester of pregnancy. None of the drugs should be used by nursing mothers because these drugs are excreted in breast milk.
Chlamydia
Chlamydia trachomatis is the most common STI in the United States in young adults. This infection is most often asymptomatic. Women who contract the infection are at risk for developing pelvic inflammatory disease (PID), ectopic pregnancies, and infertility. Because of this, it is recommended that all sexually active women under the age of 25 be screened annually for C. trachomatis and that all women over 25 be screened based on risk factors.
The CDC recommends azithromycin 1 g orally in a single dose as treatment for C. trachomatis infections or doxycycline 100 mg orally twice a day for 7 days. Alternatively, erythromycin base 500 mg orally four times a day for 7 days, erythromycin ethylsuccinate 800 mg orally four times a day for 7 days, levofloxacin 500 mg orally once daily for 7 days, or ofloxacin 300 mg orally twice a day for 7 days may be given.
Doxycycline is contraindicated in the second and third trimesters of pregnancy. In the case of a chlamydial infection during pregnancy, azithromycin 1 g orally in a single dose is the treatment of choice. Alternatively, amoxicillin 500 mg orally three times a day for 7 days may be given. If neither azithromycin nor amoxicillin is an option, erythromycin may be used.
Neonates may contract C. trachomatis from exposure to the mother’s infected cervix during delivery. It most frequently presents as conjunctivitis that develops 5 to 12 days after delivery; however, C. trachomatis can also cause pneumonia in infants between 1 and 3 months old. Prenatal screening and treatment is the best means of prevention. Erythromycin ophthalmic ointment, administered to prevent gonococcal ophthalmia, may also prevent conjunctivitis caused by C. trachomatis.
Persons treated for Chlamydia infection should be instructed to abstain from sexual intercourse for 7 days after single-dose therapy or until a 7-day regimen is completed. Partners should be treated if they had sexual contact during the 60 days preceding the onset of symptoms or diagnosis.
Gonorrhea
In the United States, gonorrhea is the second most common communicable disease. In men, infection by N. gonorrhoeae causes a greenish yellow or whitish discharge from the penis, accompanied by burning with urination. These symptoms usually prompt them to seek evaluation and treatment but often not until they have spread the infection to others. In women, N. gonorrhoeae is frequently asymptomatic. Left untreated, women with N. gonorrhoeae infections develop PID, which can cause tubal scarring that leads to ectopic pregnancies and infertility. Oral infections caused by N. gonorrhoeae cause sore throat and trouble swallowing; on examination, the pharynx resembles strep throat.
Because of the development of resistant N. gonorrhoeae, dual drug therapy is recommended with ceftriaxone 250 mg given intramuscularly (IM) in a single dose plus azithromycin 1 g orally in a single dose for uncomplicated urogenital infections or oral infections. If ceftriaxone is not available, cefixime 400 mg orally in a single dose plus azithromycin 1 g orally in a single dose may be given. Use of two drugs improves treatment efficacy and slows the development of drug resistance.
For those who are allergic to cephalosporins, gemifloxacin 320 mg orally in a single dose plus azithromycin 2 g orally in a single dose may be used; or, alternatively, gentamicin 240 mg IM in a single dose plus azithromycin 2 g orally in a single dose may be used. Women who are diagnosed with N. gonorrhoeae while pregnant should be treated with ceftriaxone 250 mg in a single IM dose and azithromycin 1 g orally as a single dose. Children under 45 kg should receive 25 to 50 mg/kg intravenously (IV) or IM, not to exceed 125 mg IM in a single dose.
Neonates may contract N. gonorrhoeae from exposure to the mother’s infected cervix during delivery. The infection most frequently presents as an acute illness that develops 2 to 5 days after delivery. Prenatal screening and treatment is the best means of prevention, and most states require neonates to be administered erythromycin (0.5%) ophthalmic ointment in each eye in a single application at birth to prevent conjunctivitis caused by N. gonorrhoeae.
Persons receiving treatment for gonorrhea should be instructed to abstain from sexual activity for 7 days after treatment. Persons diagnosed with gonorrhea should also be tested for Chlamydia, syphilis, and HIV. Partners should be treated if they had sexual contact during the 60 days preceding the onset of symptoms or diagnosis.
Syphilis
Syphilis is caused by the bacteria Treponema pallidum; if not treated early in the infectious process, it produces systemic disease that can be fatal. The disease is divided into three stages: primary, secondary, and tertiary.
Primary syphilis infections present with a sore, or chancre, at the site where the infection entered the body—typically, the penis in men and outer genitals or inner vagina in women. It is usually painless. The chancre develops about 3 weeks after exposure and resolves in 3 to 6 weeks without treatment. During this stage, the person is very contagious, even after the chancre has resolved.
Secondary syphilis is characterized by a skin rash that appears 2 to 8 weeks after the chancre. It may occur anywhere on the body, commonly on the hands and soles of the feet; the rash usually does not itch. Mucocutaneous lesions, fever, fatigue, sore throat, and lymphadenopathy may occur as well. The rash usually resolves in about 2 months. During this stage, the person remains very contagious, even after the rash has resolved. After the rash has resolved, a period that lasts anywhere from 1 year to 20 years goes by without any symptoms. This is called the latent stage, and it occurs in persons who have gone untreated. A person may remain contagious during the latent period, and diagnosis can only be made through blood testing.
Tertiary syphilis may occur as early as 1 year after infection or at any time during an untreated person’s lifetime. Large sores inside the body or on the skin occur in the tertiary stage, along with cardiovascular and ocular syphilis and neurosyphilis. Examination of the cerebral spinal fluid (CSF) should be done in persons in the tertiary stage to determine neurologic involvement, even in the absence of clinical neurologic findings.
To diagnose syphilis, two types of serologic testing are necessary to avoid false positives. One test should be a nontreponemal antibody test (e.g., Rapid Plasma Reagin [RPR] or Venereal Disease Research Laboratory [VDRL]) that tests for antibodies produced when a person has syphilis, although it may be produced in other diseases as well (e.g., Lyme disease or malaria). The other test should be a treponemal antibody test (e.g., fluorescent treponemal antibody absorption [FTA-ABS] or T. pallidum particle agglutination assay [TP-PA]), a test for antibodies that specifically target T. pallidum.
Treatment for primary and secondary syphilis is benzathine penicillin G, 2.4 million units given IM in one dose. Infants and children should be treated with benzathine penicillin G 50,000 units/kg IM up to the adult dose of 2.4 million units in a single dose, and these patients should be followed by a pediatric infectious disease specialist.
Adults with early latent syphilis should be treated with benzathine penicillin G 2.4 million units IM in a single dose; those with late latent syphilis or latent syphilis of unknown duration should receive benzathine penicillin G 7.2 million units total, administered as three doses of 2.4 million units IM each at 1-week intervals. Infants and children with early latent syphilis should be treated with benzathine penicillin G 50,000 units/kg IM, up to the adult dose of 2.4 million units in a single dose; those with late latent syphilis should receive benzathine penicillin G 50,000 units/kg IM, up to the adult dose of 2.4 million units, administered as three doses at 1-week intervals (total 150,000 units/kg up to the adult total dose of 7.2 million units). Infants and children should be managed by a pediatric infectious disease specialist.
Persons with tertiary syphilis should receive CSF analysis before initiating treatment. Those with normal CSF should receive benzathine penicillin G 7.2 million units total, administered as three doses of 2.4 million units IM each at 1-week intervals. Those with neurosyphilis or ocular syphilis should receive aqueous crystalline penicillin G 18 to 24 million units per day, administered as 3 to 4 million units IV every 4 hours or as a continuous infusion for 10 to 14 days. Alternatively, persons with neurosyphilis or ocular syphilis may be treated with procaine penicillin G 2.4 million units IM once daily plus probenecid 500 mg orally four times a day, both for 10 to 14 days. This alternative treatment should only be given to persons whose adherence can be ensured.
Pregnant women can pass syphilis to their fetus, with potentially fatal consequences. Benzathine penicillin G is the only treatment for syphilis during pregnancy. Pregnant women with syphilis in any stage who report they are allergic to penicillin should undergo penicillin allergy skin testing and desensitization, and then should be treated with penicillin.
Partners should be treated if they had sexual contact during the 90 days preceding the diagnosis of primary, secondary, or early latent syphilis even if serologic testing is negative. If greater than 90 days, treatment should be initiated if serologic testing is positive or if testing is not available. All persons with syphilis at any stage should be tested for HIV.
Viral Pathogens
Infection caused by viral pathogens is not curable, although medication therapy is palliative. These include herpes simplex virus 1 (HSV-1; cross-contaminated from oral to genital) and HSV-2, HPV, and HIV.
Herpes Simplex Virus
Genital herpes is a life-long viral infection. Two types of HSV can cause genital herpes: HSV-1 and HSV-2. Most cases of recurrent genital herpes are caused by HSV-2. Approximately 50 million people in the United States are infected with genital herpes. However, an increasing number of herpes infections are caused by HSV-1. Both types of the virus cause lesions that look like blisters, which crust over and scab. They may last for 2 to 4 weeks. The lesions may be accompanied by fever, lymphadenopathy, headache, and painful urination. Most HSV-2 cases go undiagnosed and are transmitted by people unaware that they have the infection or who are asymptomatic when transmission occurs.
Antiviral drugs are beneficial to most symptomatic patients and are the mainstay of management. It is imperative that nurses counsel patients with herpes regarding sexual and perinatal transmission and methods to reduce transmission.
Systemic antiviral drugs can control some of the signs and symptoms of genital herpes during initial and recurrent episodes or when used for daily suppressive therapy. However, these do not cure herpes or reduce the frequency and severity of recurrent episodes following drug discontinuation. Three antiviral drugs are used in the management of genital herpes: (1) acyclovir, (2) valacyclovir, and (3) famciclovir.
Recommendations for drug therapy of initial genital herpes infections is recommended using acyclovir 400 mg orally three times a day for 7 to 10 days, acyclovir 200 mg orally five times a day for 7 to 10 days, valacyclovir 1 g orally twice a day for 7 to 10 days, or famciclovir 250 mg orally three times a day for 7 to 10 days. Treatment can be extended if healing is incomplete after 10 days of therapy.
Suppressive therapy reduces the frequency of genital herpes recurrences by 70% to 80% in patients who have frequent recurrences. Recommended regimens are acyclovir 400 mg orally twice a day, valacyclovir 500 mg orally once a day, valacyclovir 1 g orally once a day, or famciclovir 250 mg orally twice a day. Valacyclovir 500 mg once a day might be less effective than other valacyclovir or acyclovir dosing regimens in persons who have 10 episodes or more per year.
For episodic treatment to be effective, treatment should begin within 1 day of lesion onset or during the prodrome (e.g., burning, itching, or tingling) that occurs anywhere from 30 minutes to a couple of days before some outbreaks. Patients should be provided with a prescription for the drug with instructions to initiate treatment immediately when symptoms begin. The recommended regimens for episodic therapy are acyclovir 400 mg orally three times a day for 5 days, acyclovir 800 mg orally twice a day for 5 days, acyclovir 800 mg orally three times a day for 2 days, valacyclovir 500 mg orally twice a day for 3 days, valacyclovir 1 g orally once a day for 5 days, famciclovir 125 mg orally twice daily for 5 days, famciclovir 1 g orally twice daily for 1 day, or famciclovir 500 mg once, followed by 250 mg twice daily for 2 days.
Sexual partners should be evaluated, treated if symptomatic, and counseled. Asymptomatic sex partners should be questioned about a history of genital lesions and offered serologic testing for HSV infection.
The risk of vertical transmission is high (30% to 50%) among women who become infected near the time of delivery and low (<1%) among women with a prenatal history of herpes or those who become infected early in the pregnancy. Prevention of vertical transmission depends on both preventing infection during late pregnancy and avoiding exposure to viral shedding during delivery. The recommended drug regimen for suppressive therapy of pregnant women with recurrent genital herpes is acyclovir 400 mg orally three times a day or valacyclovir 500 mg orally twice a day with treatment recommended starting at 36 weeks of gestation.
Human Immunodeficiency Virus
Two to four weeks after exposure, HIV infection typically presents with an acute flulike syndrome that includes fever, fatigue, rash, pharyngitis, and lymphadenopathy. HIV is a chronic illness that progressively depletes CD4 T lymphocytes and ends with symptomatic acquired immunodeficiency syndrome (AIDS). Early diagnosis and treatment is essential to reduce the risk of transmitting HIV to others and to maintain quality of life.
Persons with acute HIV infection are at high risk for transmitting HIV to their partner because the concentration of virus in blood and genital secretions is extremely elevated. Antiretroviral therapy (ART) during acute HIV infection is recommended because it substantially reduces transmission to others. See Chapter 29 for drugs used to treat HIV.
Partners (sexual partners and those with whom needles and syringes are shared) should be notified concerning possible exposure to HIV. Early diagnosis and treatment reduces the risk for further HIV transmission. Partner notification for HIV infection should be confidential.
All pregnant women should be tested for HIV infection during the first prenatal visit. A second test during the third trimester, preferably at less than 36 weeks’ gestation, is recommended for those known to be at high risk for HIV.
Human Papillomavirus
Of the roughly 100 types of HPV infection that have been identified, nearly 40 infect the genital area. Most HPV infections are self-limited and asymptomatic, and most sexually active persons will become infected with HPV at some point in their lifetime. High-risk HPV infections (e.g., HPV types 16 and 18) cause most cervical, penile, vulvar, vaginal, anal, and oropharyngeal cancers. Low-risk HPV infection (e.g., HPV types 6 and 11) cause genital warts and recurrent respiratory papillomatosis. Screening with the Papanicolaou (“Pap”) test can detect cervical dysplasia, which can be a precursor to cervical cancer if left untreated. Whereas the Pap test can determine whether the cervical cells are abnormal, an HPV test specifically looks for high-risk HPV in cervical cells.
There are several HPV vaccines approved for use in the United States: a bivalent vaccine that prevents infection with HPV types 16 and 18, which cause 66% of all cervical cancers; a quadrivalent vaccine that prevents infection with HPV types 6, 11, 16, and 18, which cause 90% of all genital warts; and a 9-valent vaccine that prevents infection with HPV types 6, 11, 16, 18, 31, 33, 45, 52, and 58. See Chapter 31 for a discussion on vaccines.
Because most HPV infections do no harm, they do not require treatment and tend to resolve on their own. Because of this, antiviral therapy is not recommended. Treatment is aimed at removal of genital warts and precancerous lesions and treatment of cervical cancer and includes cryotherapy (freezing) or a loop electrosurgical excision procedure (LEEP) to cut away abnormal tissue.
Condom use can lower the risk of transmitting and developing HPV infections. Limiting the number of sex partners can also reduce the risk for HPV. However, abstaining from sexual activity is the most reliable method for preventing HPV infection.
Other Pathogens
Pediculosis Pubis
Persons with pediculosis pubis, a parasitic infection caused by Phthirus pubis, usually seek treatment because of extreme pruritus of the body part or area where the lice are moving and laying egg cases. Infected persons may also notice lice or nits on their pubic hair. Pediculosis pubis is usually transmitted by sexual contact.
Recommended treatment is with a permethrin 1% cream rinse applied to affected areas and washed off after 10 minutes, or pyrethrins with piperonyl butoxide are applied to the affected area and washed off after 10 minutes. Alternatively, malathion 0.5% lotion can be applied to affected areas and washed off after 8 to 12 hours, or ivermectin 250 mcg/kg can be given orally and repeated in 2 weeks.
Sexual partners within the previous month should be treated, and bedding and clothing must be decontaminated. Sexual contact should be avoided until treatment is complete. Pregnant and lactating women should be treated with either permethrin or pyrethrins with piperonyl butoxide.
Scabies
Infection with Sarcoptes scabiei causes pruritus, which takes up to several weeks to develop. Scabies in adults frequently is sexually acquired, although scabies in children usually is not.
Treatment consists of permethrin 5% cream applied to all areas of the body from the neck down and washed off after 8 to 14 hours or ivermectin 200 mcg/kg orally, repeated in 2 weeks. Permethrin is the treatment of choice for infants and young children. Alternatively, lindane 1%—either 1 oz of lotion or 30 g of cream—applied in a thin layer to all areas of the body from the neck down and thoroughly washed off after 8 hours may be used; however, pregnant women, infants, and children under the age of 10 years should not be treated with lindane.
Bedding and clothing should be decontaminated by either machine washing, machine drying using the hottest cycle, or dry cleaning; alternatively, bedding and clothing should be removed from body contact for at least 72 hours. Persons who have had sexual, close personal, or household contact with the patient within the month preceding scabies infestation should be examined and treated if infected.
Ivermectin likely poses a low risk to pregnant women and is likely compatible with breastfeeding; however, because of limited data regarding ivermectin use in pregnant and lactating women, permethrin is the preferred treatment
Trichomoniasis
The protozoan parasite Trichomonas vaginalis is the most common curable STI in the United States. Nearly 7.5 million cases occur annually. Most people with T. vaginalis (70% to 85%) have minimal or no symptoms. Men may develop urethritis, epididymitis, or prostatitis. Some infected women may develop a diffuse vaginal discharge that is malodorous and yellow green, with or without vulvar irritation.
The nitroimidazoles are the only class of antimicrobials effective against T. vaginalis. Metronidazole and tinidazole are approved for oral or parenteral treatment of trichomoniasis. The recommended regimen is metronidazole 2 g orally in a single dose or tinidazole 2 g orally in a single dose. Alternatively, metronidazole 500 mg orally twice a day for 7 days may be used.
Alcohol should be avoided during treatment with nitroimidazoles to prevent the likelihood of a disulfiram-like reaction. Abstinence from alcohol use should continue for 24 hours after completion of metronidazole or 72 hours after completion of tinidazole. Concurrent treatment of all sex partners is critical to prevent transmission and reinfection.
T. vaginalis is readily passed between sex partners. The best way to prevent infection is through consistent and correct use of condoms. Partners of men who have been circumcised might have a somewhat reduced risk of T. vaginalis infection.
T. vaginalis infection in pregnant women is associated with premature rupture of membranes, preterm delivery, and delivery of a low-birthweight infant. The recommended treatment regimen in pregnant women is metronidazole 2 g orally in a single dose.
Vulvovaginal Candidiasis
Vulvovaginal candidiasis (VVC) is usually caused by Candida albicans but may also be caused by other Candida species. Typical symptoms of VVC include pruritus, vaginal soreness, dyspareunia, external dysuria, and abnormal vaginal discharge. Signs include vulvar edema, fissures, excoriations, and a thick, curdy vaginal discharge.
Treatment with topically applied azole drugs results in symptomatic relief and negative cultures in 80% to 90% of patients who complete therapy. A variety of over-the-counter (OTC) and prescription drugs may be used to treat VVC. Treatment regimens include OTC and prescription intravaginal agents.
Over-the-Counter Intravaginal Agents
Clotrimazole 1% cream 5 g intravaginally daily for 7 to 14 days, clotrimazole 2% cream 5 g intravaginally daily for 3 days, miconazole 2% cream 5 g intravaginally daily for 7 days, miconazole 4% cream 5 g intravaginally daily for 3 days, one miconazole 100-mg vaginal suppository daily for 7 days, one miconazole 200-mg vaginal suppository daily for 3 days, one miconazole 1200 mg vaginal suppository, or tioconazole 6.5% ointment 5 g intravaginally in a single application.
Prescription Intravaginal Agents
Butoconazole 2% cream (single-dose bioadhesive product) 5 g intravaginally in a single application, terconazole 0.4% cream 5 g intravaginally daily for 7 days, terconazole 0.8% cream 5 g intravaginally daily for 3 days, or one terconazole 80 mg vaginal suppository daily for 3 days. Alternatively, an oral drug—fluconazole 150 mg orally in a single dose—may be used.
Topical agents usually cause no systemic side effects, although local burning or irritation might occur. Oral azoles occasionally cause nausea, abdominal pain, and headache.
VVC occurs frequently during pregnancy. Only topical azole therapies, applied for 7 days, are recommended for use among pregnant women. Uncomplicated VVC is not usually acquired through sexual intercourse, thus treatment of sexual partners is not necessary.
Prevention of Sexually Transmitted Infections
Because STIs can threaten reproductive health, neonatal health, fertility, and even life, early diagnosis and treatment are crucial but are less effective than prevention. Please review the information in Box 54.1 and in the Nursing Process box that discusses STI prevention.
Evaluation
• Intervention has been successful if patients and their partners remain free of infection.
• The patient is able to avoid sexual practices that carry risk for acquiring STIs, including intercourse without the use of a condom.
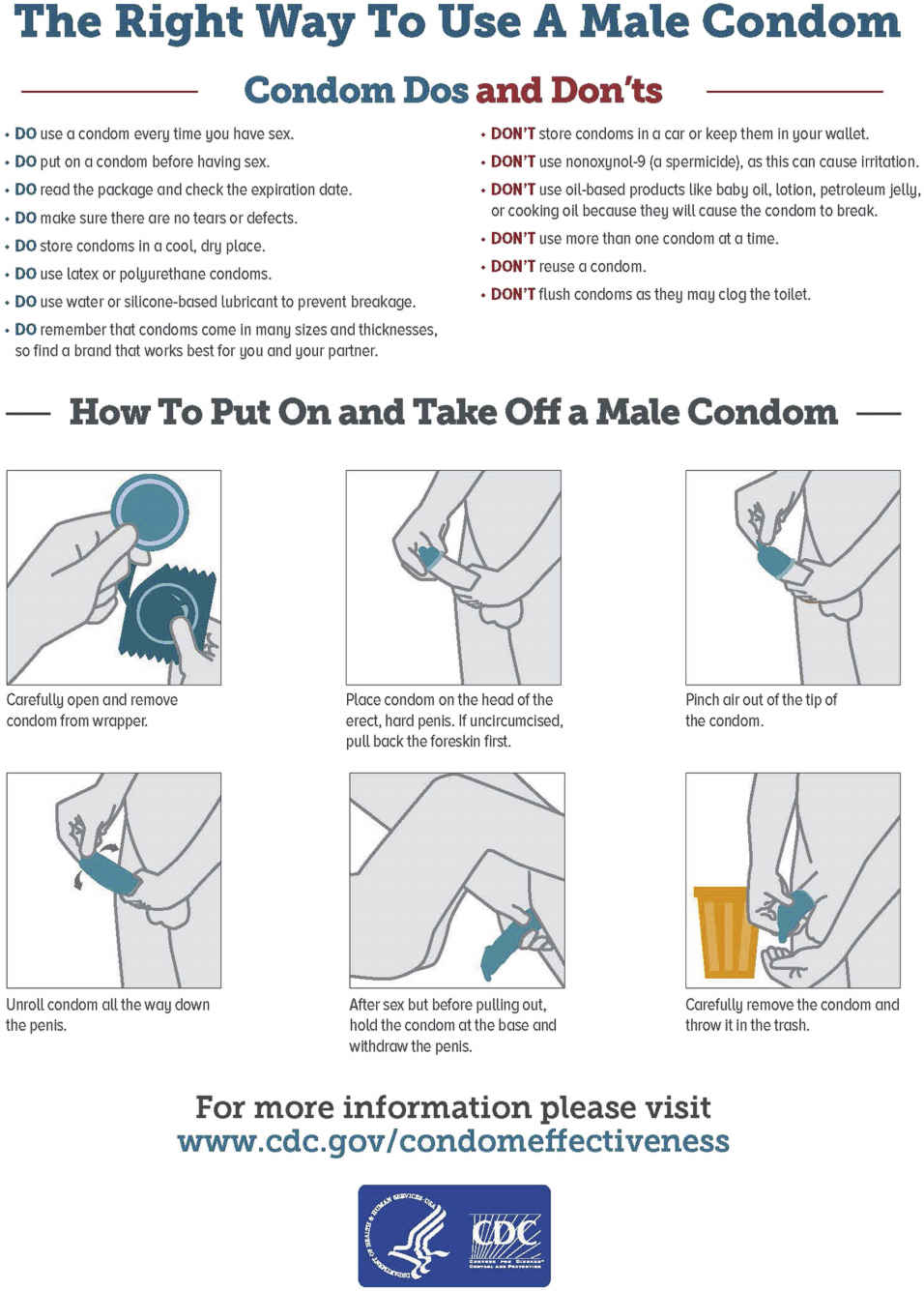
FIG. 54.2 How to Use a Male Condom.
From Centers for Disease Control and Prevention. (2016). The right way to use a male condom. Retrieved from www.cdc.gov/condomeffectiveness/male-condom-use.html
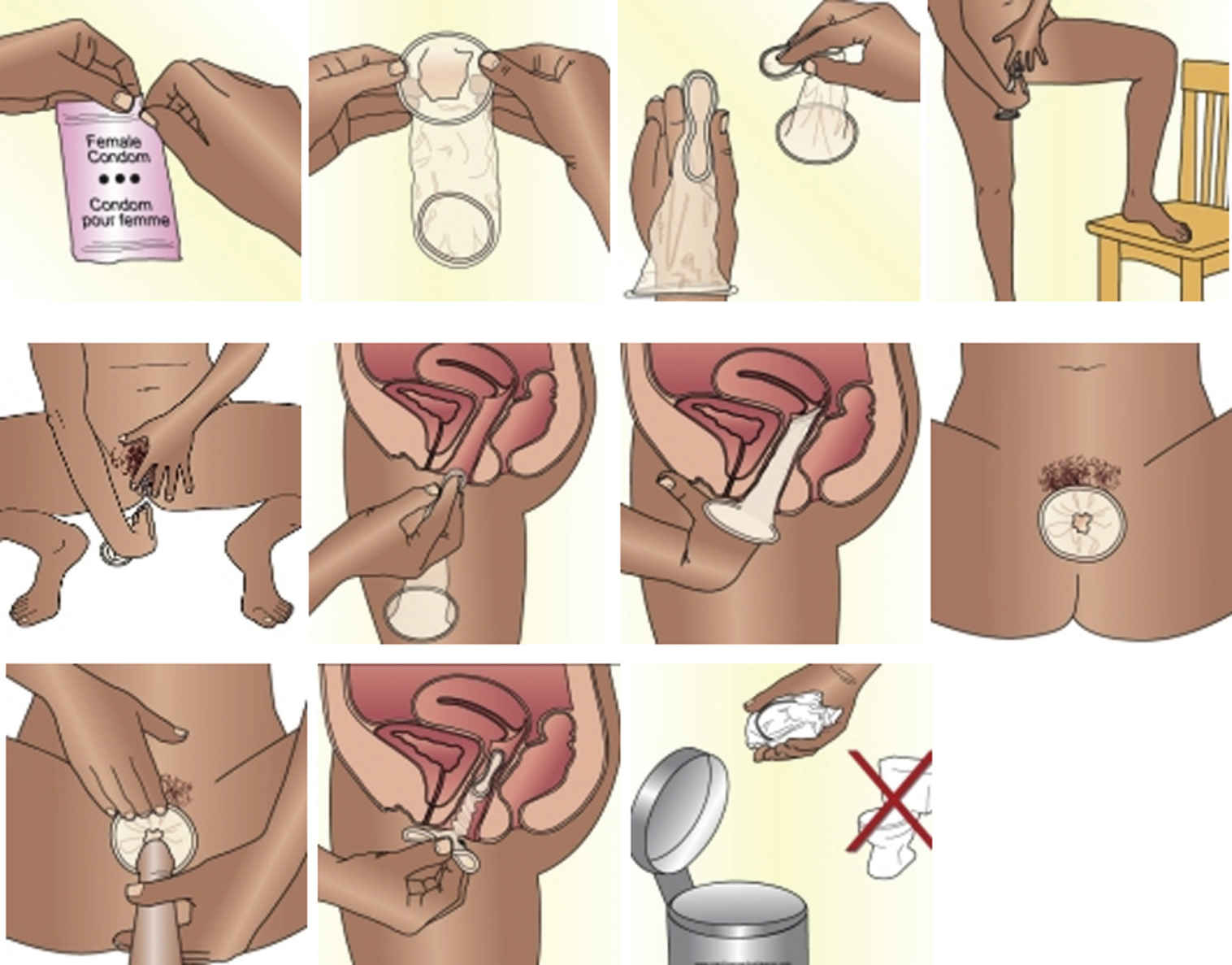
FIG. 54.3 How to Use a Female Condom.
1. Before using the female condom for the first time during sex, you should practice placing the condom in your vagina a couple of times. Inserting the condom becomes easier once you get the hang of it.
2. When you are ready to have intercourse, but before you become intimate, check the expiration date on the package to make sure that you can still use it. Then open the package and spread lubricant or spermicide on the outside of the closed end.
3. When you are ready to insert the female condom, you will need to find a comfortable position that works for you. Try squatting down, lying down, or placing one foot on a chair while standing.
4. Using your thumb and forefinger, squeeze the sides of the inner ring together. The condom may be a bit slippery, so make sure you have a firm grip before attempting to insert it into your vagina.
5. Using your forefinger as a guide, insert the inner ring much like you would a tampon, and push it up toward your cervix with your finger.
6. Once you have reached the cervix, the condom will expand naturally, and you will no longer be able to feel it. If you can still feel it, you have not placed it far enough inside.
7. Gently remove your finger and make sure that at least one inch of the condom is hanging outside of the vagina. Anything more than that indicates it has not been inserted far enough, and you’ll need to check that the inner ring is positioned correctly.
8. When you are ready to have intercourse, have your partner insert his penis in the outer ring and into the condom. You may want to help him, making sure that his penis is actually entering the condom and not just pushing it to one side.
From New Health Advisor. (2016). How to use a female condom: Pictures and instructions. Retrieved from www.newhealthadvisor.com/How-to-Use-Female-Condom-Picture.html
Critical Thinking Case Study
A 16-year-old Caucasian female is seen in your office for evaluation of a possible STI. She states that her partner has noted a whitish penile discharge and has burning with urination. When questioned, she states she’s been sexually active, both orally and vaginally, for 2 years and has had four partners. When questioned, she denies using any barrier methods to avoid infection, admits to having a sore throat, and denies vaginal symptoms.
1. What is the presumptive diagnosis?
2. Based on this diagnosis, what is the most appropriate treatment for your patient?
3. Why are two drugs recommended for treatment?
4. Should your patient’s partner be treated? What about past partners?
5. What is the best way to avoid reinfection?