Selective (Supraomohyoid) Neck Dissection, Levels I-III
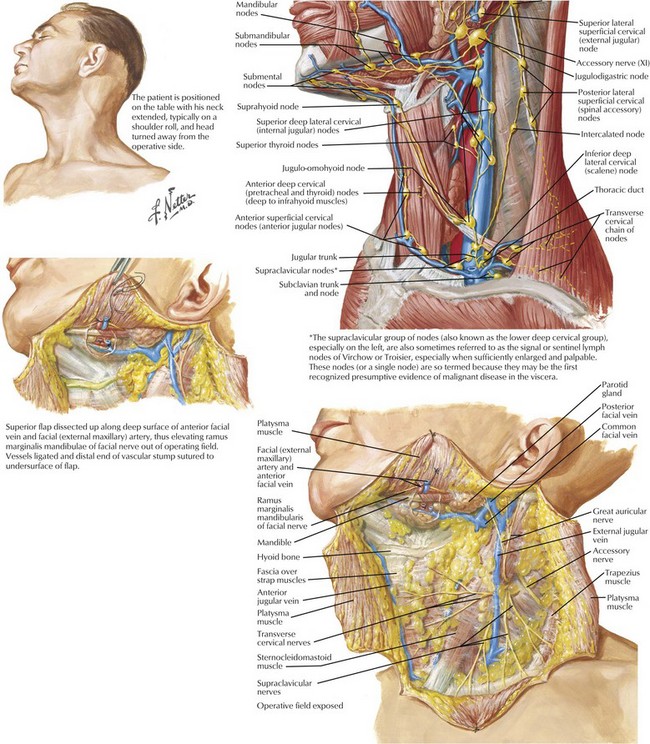
Neck Anatomy for Surgical Planning
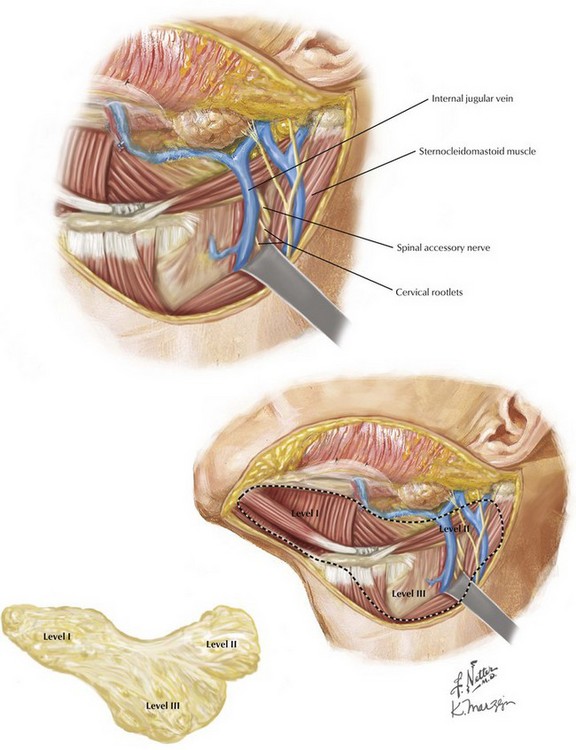
Understanding the regional lymphatic drainage pathways is critical when planning which type of neck dissection will be employed (Fig. 1-1). A supraomohyoid neck dissection is performed when treating patients who are at risk for micrometastasis in levels I, II, and III. The boundaries of levels I (submental and submandibular), II (upper jugular nodal chain), and III (midjugular nodal chain) are defined as follows:
Level Ia: Bounded laterally by the medial aspects of the anterior belly of the digastric muscles, and ending medially at a line drawn from the mandible to the hyoid bone at the anatomic midline.
Level Ib: Bounded by the lateral aspect of the anterior belly of the digastric muscle, the medial aspect of the posterior belly of the digastric and stylohyoid muscles, and the inferior border of the mandibular body superiorly.
Level IIa: Bounded anteriorly and superiorly by the posterior belly of the digastric and stylohyoid muscles, posteriorly by the vertical plane defined by the spinal accessory nerve and sternocleidomastoid muscle (SCM), and inferiorly by the horizontal plane defined by the inferior border of the hyoid bone.
Level IIb: Bounded anteriorly by the jugular vein and inferiorly by the vertical plane defined by the spinal accessory nerve, posteriorly by the posterior border of the SCM, and superiorly by the skull base.
Level III: Bounded superiorly by the horizontal plane defined by the inferior border of the hyoid bone, inferiorly by the horizontal plane defined by the inferior border of the cricoid cartilage and/or the omohyoid muscle as it crosses the internal jugular vein, anteriorly by the lateral border of the sternohyoid muscle, and posteriorly by the posterior border of the SCM.
Incision Planning and Patient Positioning for Neck Dissection
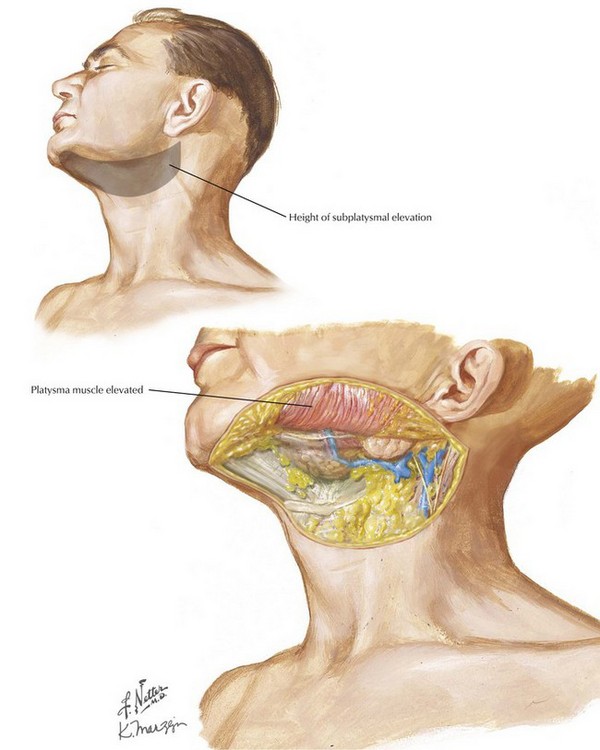
Raising the Subplatysmal Flap
Skin and subcutaneous incisions are continued down through the subcutaneous fat and platysma muscle, but not through the superficial layer of the deep cervical fascia. A superior subplatysmal flap is then elevated up to the inferior border of the mandible. Care is taken to keep the plane of elevation immediately subplatysmal, to aid in identification and preservation of the marginal mandibular branch of the facial nerve. Laterally, the platysma muscle is not developed, and elevation must proceed over the external jugular vein and great auricular nerve. This allows for complete elevation of the flap (Fig. 1-2).
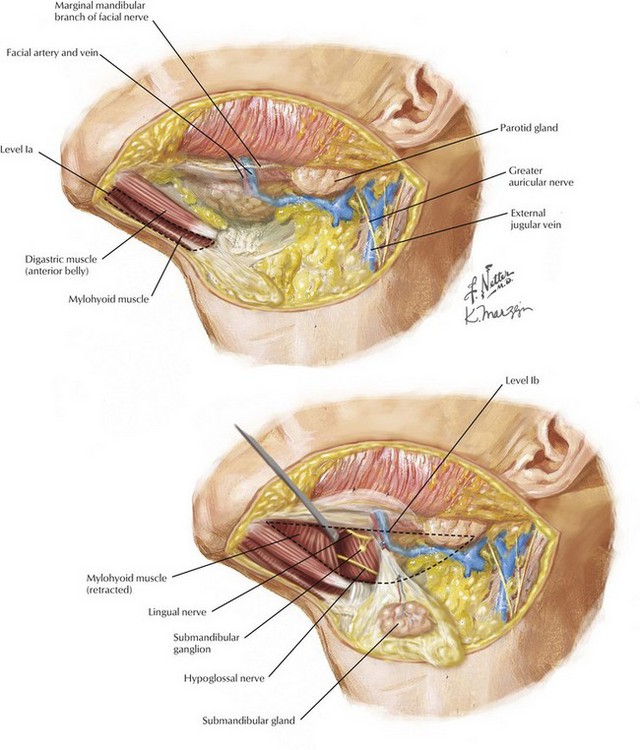
Level Ia-Ib Neck Dissection
After flap elevation, expose the anterior belly of the digastric muscle by making a midline incision from below the mentum to the hyoid bone. It is important to include all the fibrofatty contents from the contralateral medial edge of the digastric muscle. The elevation continues to the medial aspect of the submandibular gland to complete the level Ia dissection (Fig. 1-3).
Retract the mylohyoid muscle; identify and preserve the lingual and hypoglossal nerves; then identify, ligate, and divide the submandibular duct, submandibular ganglion, and corresponding vasculature. Level I is released and left pedicled by the inferior fibrofatty attachments to levels II and III (Fig. 1-3).
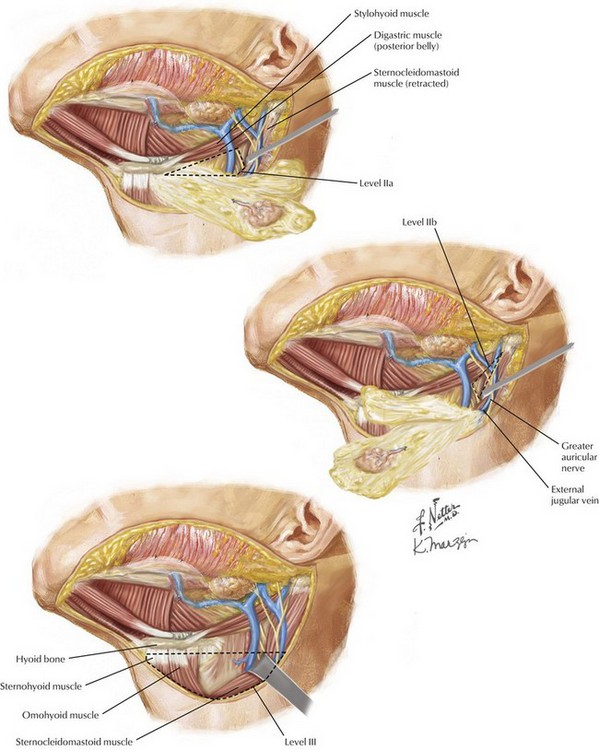
Level II-III Neck Dissection
Identify the posterior belly of the digastric muscle, creating the digastric tunnel back to the mastoid tip under the SCM (Fig. 1-4).
Once the investing fascial layer is elevated off the SCM down to the level of the deep cervical rootlets, the dissection is taken medially across the rootlets from the omohyoid muscle to the spinal accessory nerve superiorly. Care must be taken to avoid injuring the spinal accessory nerve in this area as it exits the SCM posteriorly (Fig. 1-5).
The specimen is then dissected away from the hypoglossal nerve and posterior belly of the digastric muscle until it can be easily removed. The anterior dissection will meet with the posterior dissection as the specimen is brought across the strap muscles, carotid artery, and jugular vein (Fig. 1-5).