49 Selective Nerve Root Block
Cervical Transforaminal Injection
Placement
Position
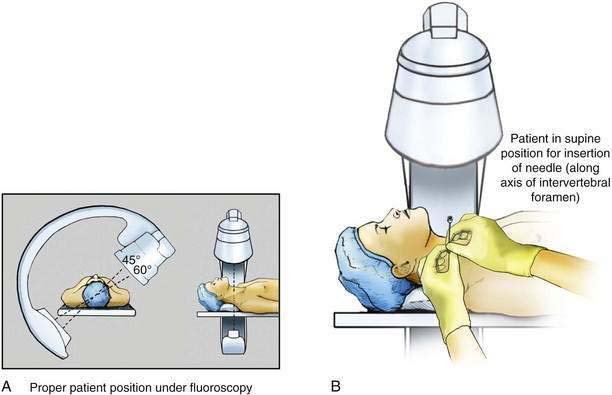
The procedure can be performed with the patient lying in a supine, oblique, or lateral decubitus position, depending on the operator’s preference and the patient’s comfort. The position must allow adequate visualization of the cervical intervertebral foramina in the anteroposterior (AP), lateral, and oblique planes (Fig. 49-1A). The important first step is to obtain a correct oblique view of the target foramen (Fig. 49-1B). In this view the foramen is maximally wide transversely, and the anterior wall of the superior articular process projects onto the silhouette of the lamina. If these criteria are not satisfied, the inclination of the fluoroscope must be adjusted until they are. The correct oblique view is essential because in less oblique views, which may nevertheless show a foramen, the vertebral artery lies along the course of the needle. Older C-arm fluoroscopy units often restrict the degree of rotation of the side opposite the unit to less than 45 degrees, which can prevent adequate visualization of the cervical intervertebral foramina on the patient’s right side when the C-arm is positioned from the patient’s left. The 60 degrees of anterior oblique angulation often needed for good visualization can be achieved simply by placing a foam cushion under the patient’s right side, thereby tilting him or her to the left, or by tilting the surface of the table to the patient’s left.
Needle Puncture
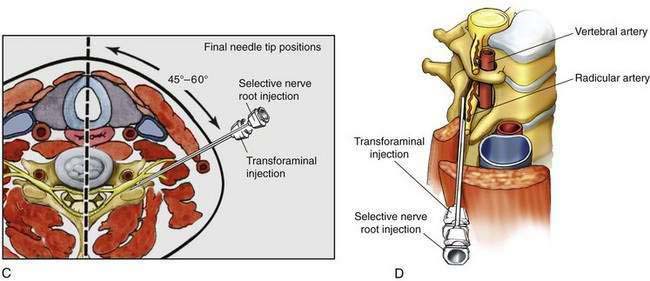
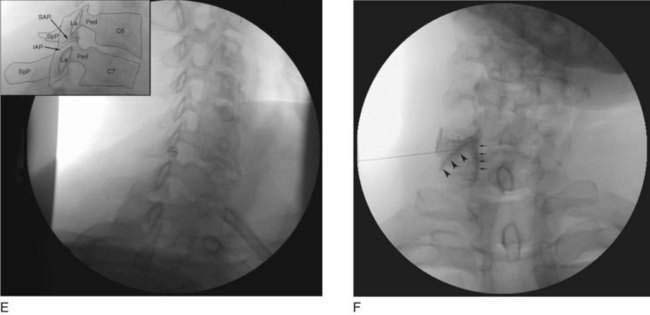
A 25-gauge, 2.5- to 3.5-inch needle is passed into the neck through a skin puncture at a point overlying the posterior half of the target foramen. Some experts advocate the use of a blunt-tipped needle to reduce the likelihood of penetration into an arterial structure. The needle tip should always lie over the anterior half of the superior articular process lest it be inserted prematurely and too far into the foramen. Once the needle has reached the superior articular process, its depth is noted. Subsequent insertion should not be more than a few millimeters beyond this depth. The needle is then repositioned to enter the foramen tangential to its posterior wall, opposite the equator of the foramen (Fig. 49-1C through E). Cephalad to this level, the needle may encounter veins; caudad to this level, the needle may encounter the spinal nerve and its arteries. The needle must stay in contact with the posterior wall lest it encounter the vertebral artery.
Under an AP fluoroscopic view, the tip of the needle is finally adjusted so that it lies opposite the midline of the articular pillars in the sagittal plane. Insertion beyond this depth increases the likelihood of puncturing the dural sleeve or thecal sac. The final needle position is checked and radiographically recorded on an oblique view, which documents needle placement against the posterior wall of the foramen, and on an AP view (Fig. 49-1F), which documents the depth of needle insertion.
To ensure that the final needle position does not change with attempts to connect and disconnect syringes directly to the needle, a short length of sterile connecting tubing is attached to the needle and further injections carried out through the distal end of this tubing. Under direct, real-time fluoroscopy, a small volume of nonionic contrast medium (≤1.0 mL) is injected. The solution should outline the proximal end of the spinal nerve and spread centrally toward the epidural space (see Fig. 49-1F).
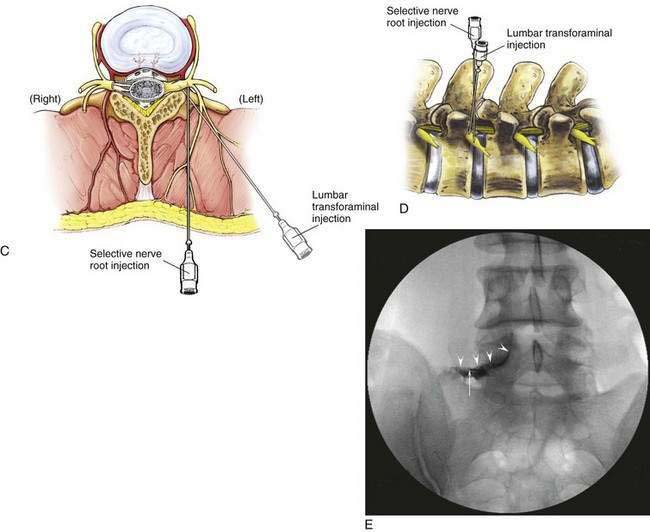
Lumbar Transforaminal Injection
Placement
Position
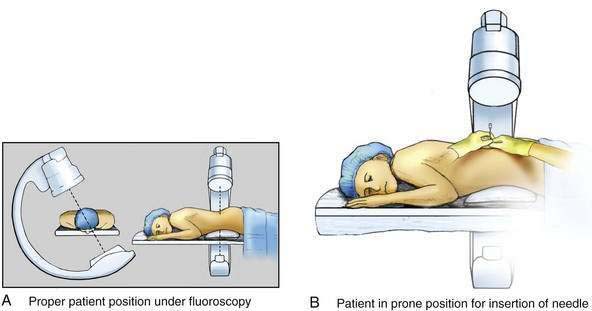
The procedure is typically performed with the patient in the prone position, with a pillow under the abdomen above the iliac crests and the pelvis tilted anteriorly (Fig. 49-2A). The first step is to obtain a 10- to 20-degree oblique view of the target foramen that allows the needle to pass into the lateral aspect of the intervertebral foramen. This is most difficult for the LS-Sl level, where the iliac crest blocks entry to the foramen when the oblique angle is too extreme.
Needle Puncture
Through a skin puncture point overlying the superior portion of the target foramen, just caudad to the pars interarticularis (the junction of the transverse process with the lamina or just caudad to the most proximal portion of the transverse process), a 25-gauge, 2.5- to 3.5-inch needle is passed into the back (Fig. 49-2B). Some experts advocate the use of blunt-tipped needles to reduce the likelihood of penetration into an arterial structure. The needle tip should always lie over the posterior aspect of the intervertebral foramen (Fig. 49-2C). Once the needle has reached the pars interarticularis, its depth should be noted; the radiographic image orientation is then switched to the lateral projection (Fig. 49-2D). Subsequent insertion is carried out using the lateral projection, observing the needle as it enters the foramen. The needle is advanced slowly; further insertion is halted if the patient reports a paresthesia or the needle reaches the mid-portion of the foramen in the AP dimension.
The final needle position is checked and recorded on an AP view, which documents the medial extent of the needle’s advancement. To ensure that the final needle position does not change with attempts to connect and disconnect syringes directly to the needle, a short length of sterile connecting tubing is attached to the needle and further injections carried out through the distal end of this tubing. Under direct, real-time fluoroscopy in the AP view, a small volume of nonionic contrast medium (≤1.0 mL) is injected. The solution should outline the proximal end of the exiting nerve root and spread centrally underneath the pedicle toward the epidural space (Fig. 49-2E).
Potential Problems
Only a small volume of contrast medium (≤1.0 mL) is required to outline the dural sleeve of the spinal nerve. As it spreads onto the thecal sac, the contrast medium assumes a linear configuration (see Fig. 49-2E). Rapid dilution of the contrast medium implies subarachnoid spread, which may occur if the needle has punctured the thecal sac when there is lateral dilation of the dural root sleeve into the intervertebral foramen. In that case, the procedure should be abandoned and rescheduled lest subsequently injected material penetrate the puncture made through the dura.