Misty mesentery: Increased attenuation of mesentery with fat stranding and induration
• Chronic phase

 .
.
 . No diagnosis was made at this time, and the patient was not given treatment.
. No diagnosis was made at this time, and the patient was not given treatment.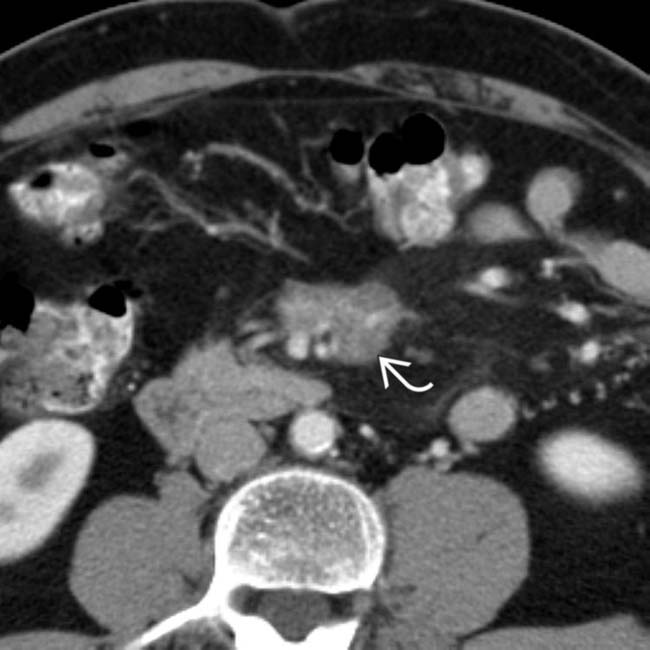
 in the mesentery that encases and narrows the mesenteric vessels.
in the mesentery that encases and narrows the mesenteric vessels.
 within the fibrotic mesenteric mass. The infiltrated mesentery and pseudocapsule
within the fibrotic mesenteric mass. The infiltrated mesentery and pseudocapsule  are still evident. This case illustrates progression of the disease over time.
are still evident. This case illustrates progression of the disease over time.IMAGING
General Features
CT Findings
• Acute mesenteritis (mesenteric panniculitis and lipodystrophy)
 Often associated with misty mesentery: Increased attenuation of mesentery with fat stranding and induration
Often associated with misty mesentery: Increased attenuation of mesentery with fat stranding and induration
 Often associated with misty mesentery: Increased attenuation of mesentery with fat stranding and induration
Often associated with misty mesentery: Increased attenuation of mesentery with fat stranding and induration
• Chronic phase (retractile mesenteritis)
DIFFERENTIAL DIAGNOSIS
Retroperitoneal and Mesenteric Lymphoma
• Early-stage lymphoma appears identical to mesenteritis with misty mesentery, mildly enlarged nodes, and rarely, fat halo sign
CLINICAL ISSUES
Presentation

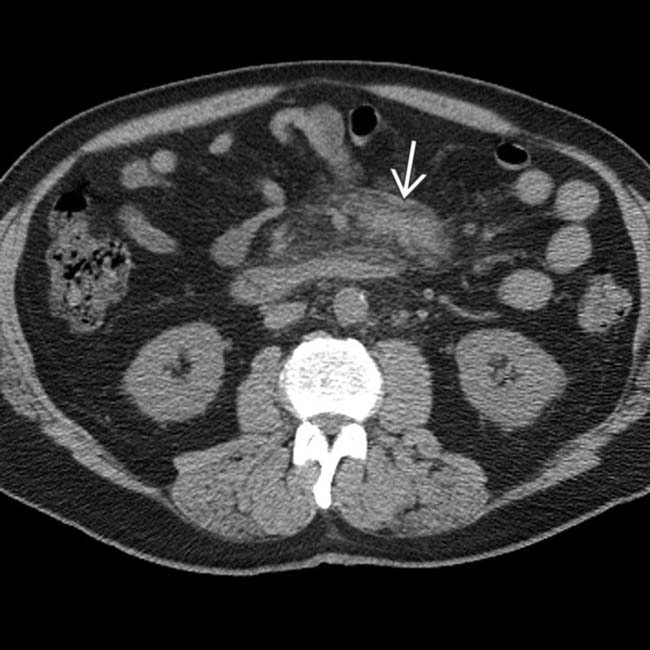
 . Multiple prominent mesenteric nodes are present
. Multiple prominent mesenteric nodes are present  with a fat halo. PET showed no increased activity, and symptoms improved with steroids.
with a fat halo. PET showed no increased activity, and symptoms improved with steroids.
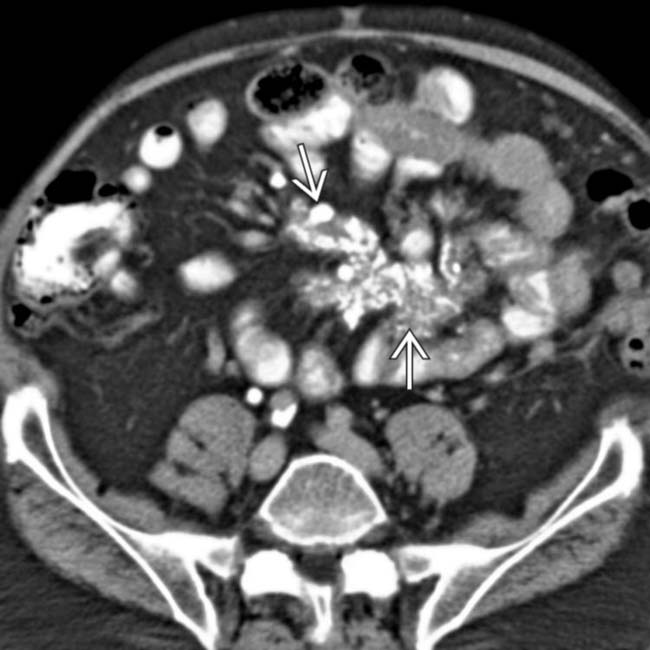
 . The mesenteric vessels
. The mesenteric vessels  are encased but not obstructed. This was found to represent sclerosing mesenteritis.
are encased but not obstructed. This was found to represent sclerosing mesenteritis.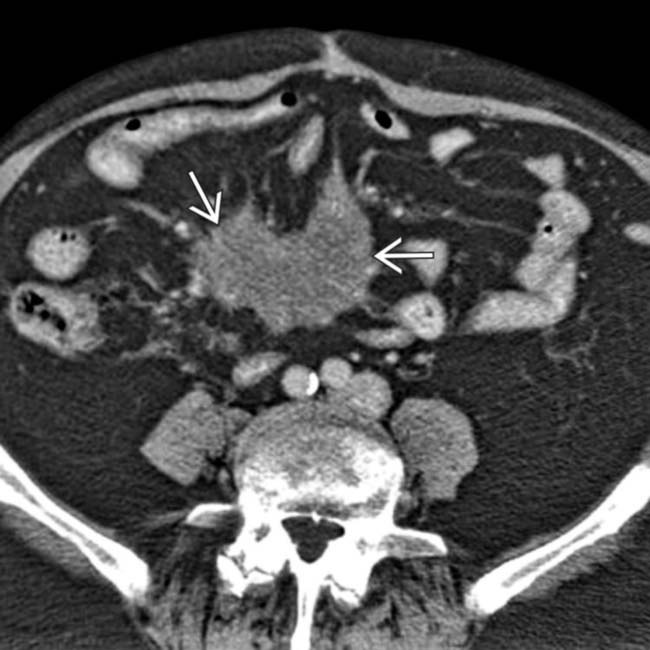
 that encases blood vessels. Note the engorgement of the mesenteric veins. This was found to represent sclerosing mesenteritis.
that encases blood vessels. Note the engorgement of the mesenteric veins. This was found to represent sclerosing mesenteritis.
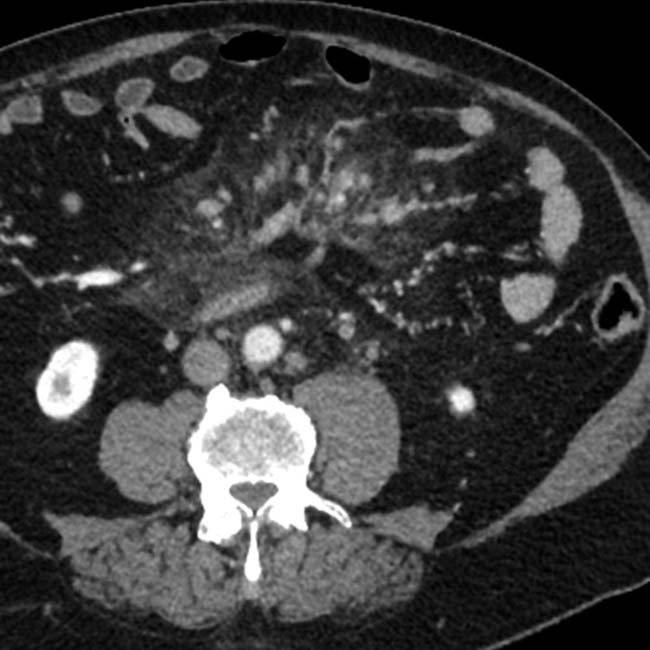
 at the base of the small bowel mesentery, encasing and narrowing the mesenteric vessels
at the base of the small bowel mesentery, encasing and narrowing the mesenteric vessels  . This was found to represent fibrosing mesenteritis at biopsy.
. This was found to represent fibrosing mesenteritis at biopsy.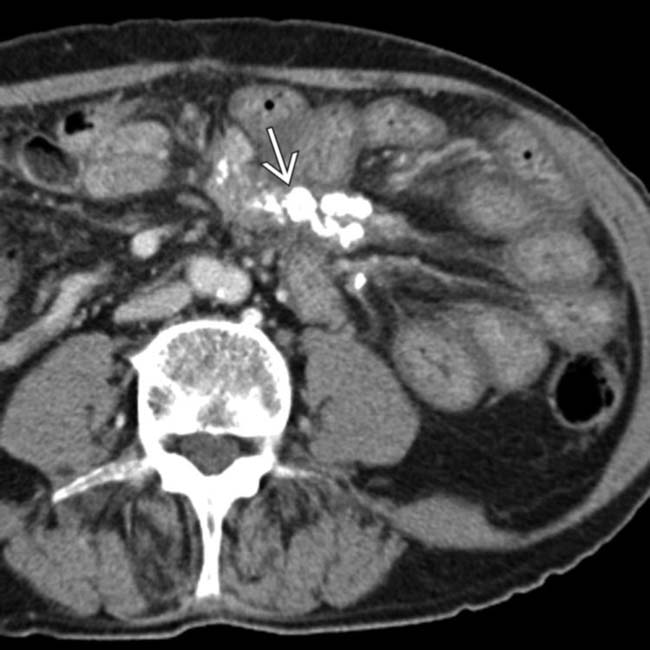
 in the left upper quadrant mesentery with tethering of surrounding bowel loops.
in the left upper quadrant mesentery with tethering of surrounding bowel loops.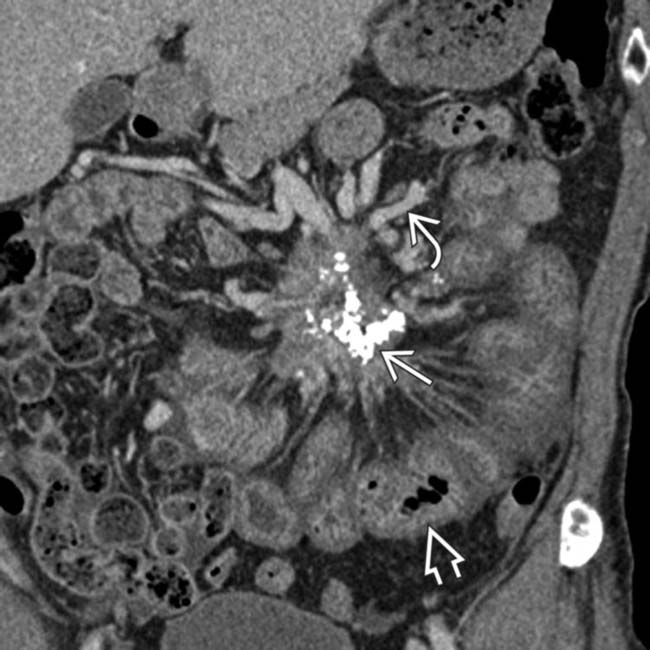
 . Note the venous collaterals
. Note the venous collaterals  due to obstruction of the superior mesenteric vein, as well as diffuse small bowel wall thickening
due to obstruction of the superior mesenteric vein, as well as diffuse small bowel wall thickening  due to venous/lymphatic obstruction. This was biopsy-proven retractile mesenteritis.
due to venous/lymphatic obstruction. This was biopsy-proven retractile mesenteritis.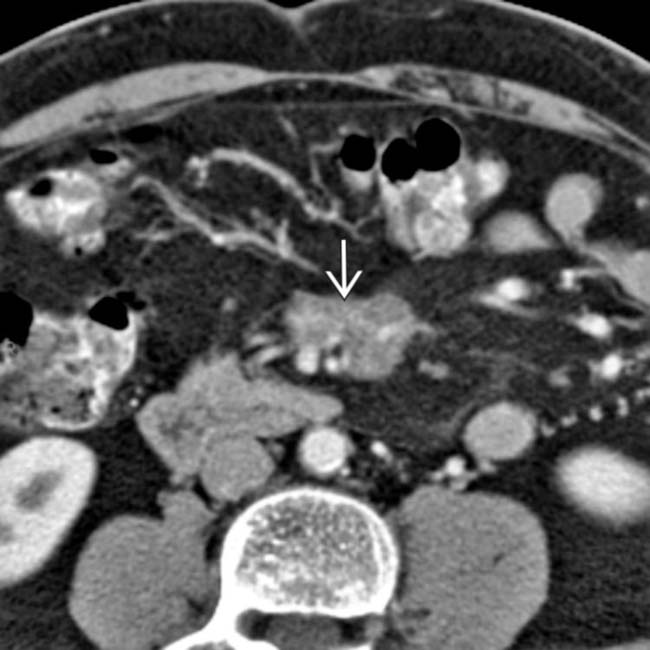
 encasing vessels, causing mesenteric venous distention. This was found to represent sclerosing mesenteritis.
encasing vessels, causing mesenteric venous distention. This was found to represent sclerosing mesenteritis.
 and vascular engorgement. This was found to represent sclerosing mesenteritis.
and vascular engorgement. This was found to represent sclerosing mesenteritis.
 and mesenteric adenopathy due to mesenteritis.
and mesenteric adenopathy due to mesenteritis.
 .
.
 that encases vessels and distorts the bowel.
that encases vessels and distorts the bowel.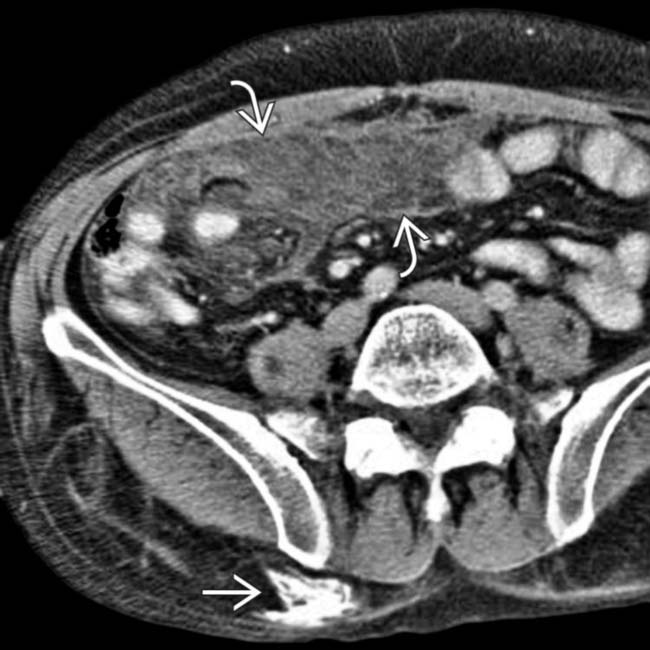
 along with subcutaneous calcification
along with subcutaneous calcification  .
.

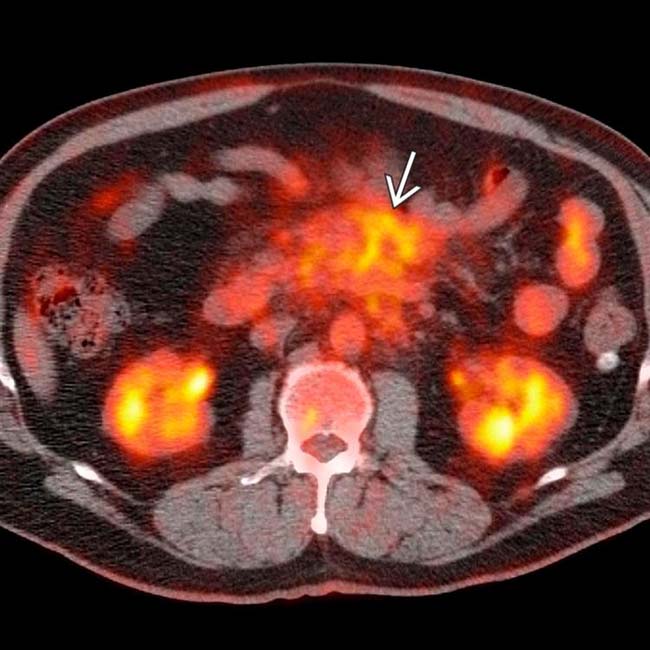
 was moderately FDG avid, raising concern for malignancy, either metastatic from the patient’s known esophageal carcinoma (considered unlikely) or from a 2nd malignancy, such as non-Hodgkin lymphoma. Laparoscopic biopsy of the mass demonstrated only inflammation and fibrosis, interpreted as sclerosing mesenteritis. Acute and chronic inflammatory processes, such as sclerosing mesenteritis and IgG4-related sclerosing disease, often demonstrate moderate to marked FDG avidity on PET, constituting a potential pitfall in misdiagnosis as malignancy.
was moderately FDG avid, raising concern for malignancy, either metastatic from the patient’s known esophageal carcinoma (considered unlikely) or from a 2nd malignancy, such as non-Hodgkin lymphoma. Laparoscopic biopsy of the mass demonstrated only inflammation and fibrosis, interpreted as sclerosing mesenteritis. Acute and chronic inflammatory processes, such as sclerosing mesenteritis and IgG4-related sclerosing disease, often demonstrate moderate to marked FDG avidity on PET, constituting a potential pitfall in misdiagnosis as malignancy.

































































 within the jejunal mesentery.
within the jejunal mesentery.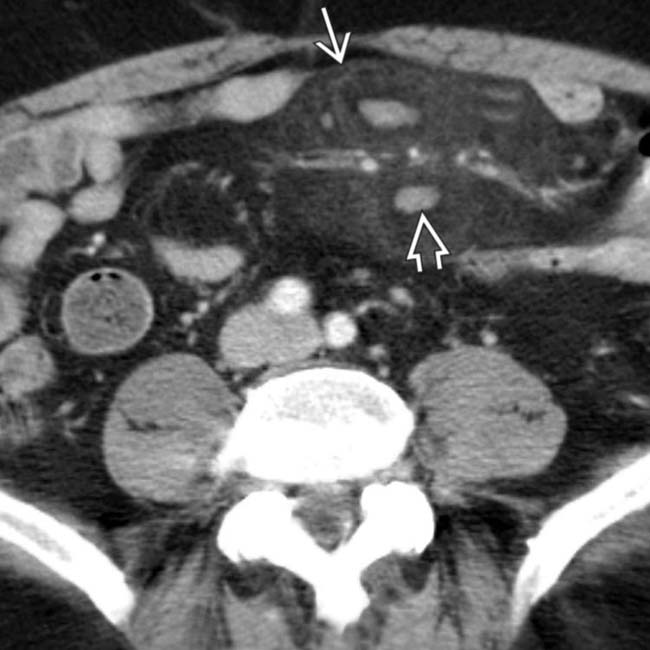
 with a surrounding halo and a pseudocapsule
with a surrounding halo and a pseudocapsule  . A positron emission tomogram (PET scan) showed no increased metabolic activity within the mass, helping to exclude the diagnosis of lymphoma. Symptoms improved with oral steroid medication.
. A positron emission tomogram (PET scan) showed no increased metabolic activity within the mass, helping to exclude the diagnosis of lymphoma. Symptoms improved with oral steroid medication.


