12 Sciatic Block
Traditional Block Technique
Placement
Anatomy
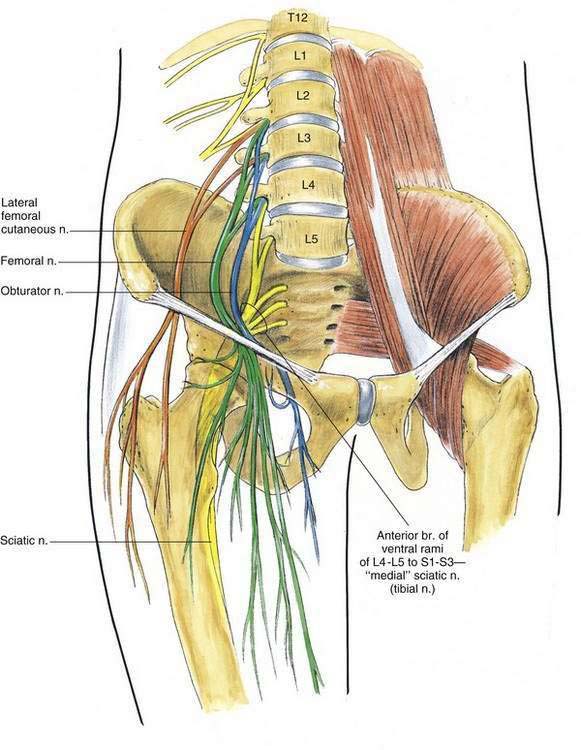
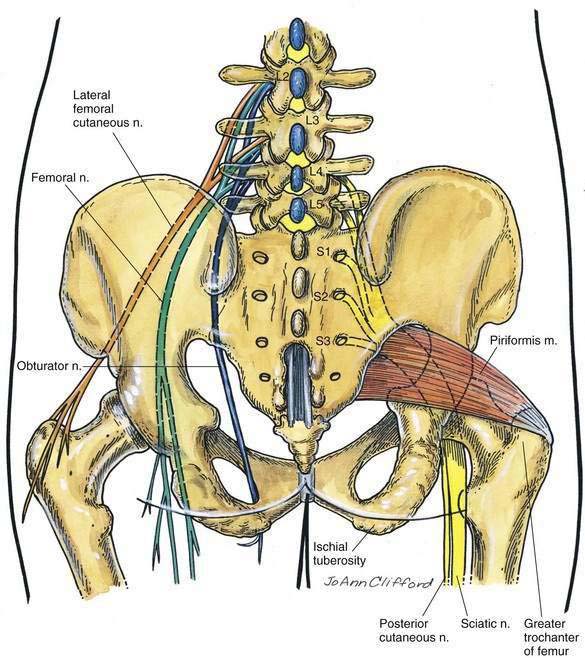
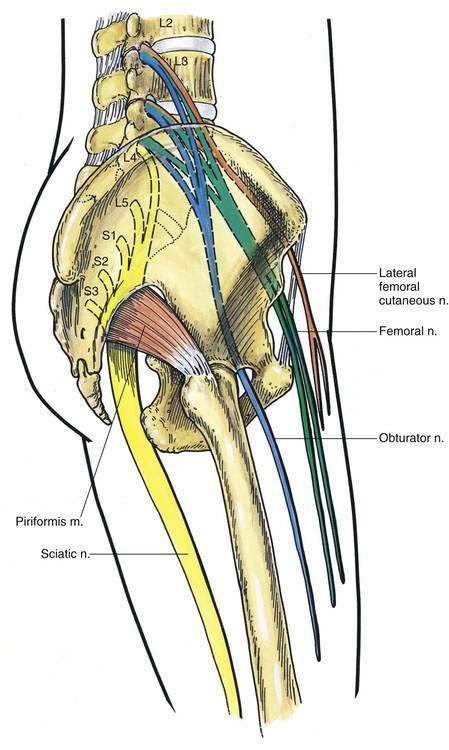
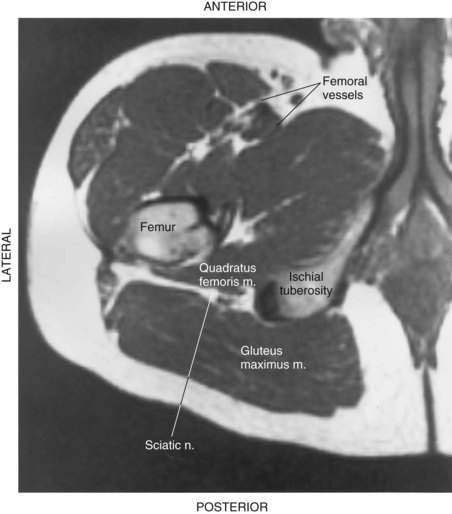
The sciatic nerve is formed from L4 through S3 roots. These roots of the sacral plexus form on the anterior surface of the lateral sacrum and are assembled into the sciatic nerve on the anterior surface of the piriformis muscle. The sciatic nerve results from the fusion of two major nerve trunks. The “medial” sciatic nerve is functionally the tibial nerve, which forms from the ventral branches of the ventral rami of L4-L5 and S1-S3; the posterior branches of the ventral rami of these same nerves form the “lateral” sciatic nerve, which is functionally the peroneal nerve. As the sciatic nerve exits the pelvis, it is anterior to the piriformis muscle and is joined by another nerve, the posterior cutaneous nerve of the thigh. At the inferior border of the piriformis, the sciatic and posterior cutaneous nerves of the thigh lie posterior to the obturator internus, the gemelli, and the quadratus femoris. At this point, these nerves are anterior to the gluteus maximus. Here, the nerve is approximately equidistant from the ischial tuberosity and the greater trochanter (Figs. 12-1 to 12-3). The nerve continues downward through the thigh to lie along the posteromedial aspect of the femur. At the cephalad portion of the popliteal fossa, the sciatic nerve usually divides to form the tibial and common peroneal nerves. Occasionally, this division occurs much higher, and sometimes the tibial and peroneal nerves are separate through their entire course. In the popliteal fossa, the tibial nerve continues downward into the lower leg, whereas the common peroneal nerve travels laterally along the medial aspect of the short head of the biceps femoris muscle.
Classic Approach
Position
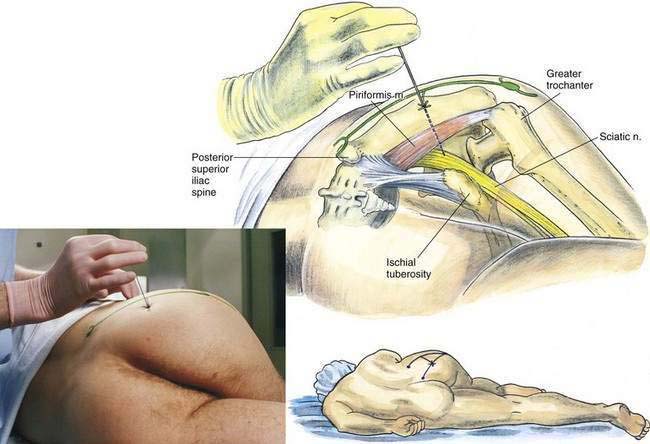
The patient is positioned laterally, with the side to be blocked nondependent. The nondependent leg is flexed and its heel placed against the knee of the dependent leg (Fig. 12-4). The anesthesiologist is positioned to allow insertion of the needle, as shown in Figure 12-4.
Needle Puncture
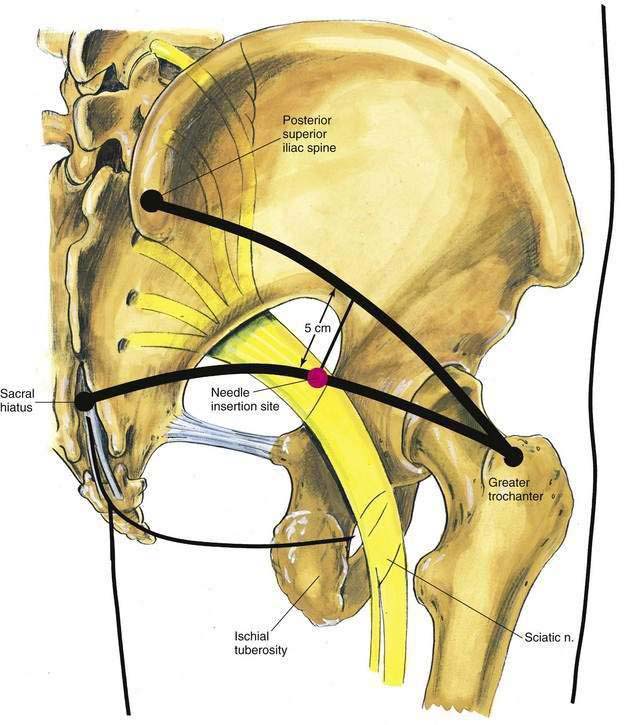
A line is drawn from the posterior superior iliac spine to the midpoint of the greater trochanter. Perpendicular to the midpoint of this line, another line is extended caudomedially for 5 cm. The needle is inserted through this point (Fig. 12-5). As a cross-check for proper placement, an additional line may be drawn from the sacral hiatus to the previously marked point on the greater trochanter. The intersection of this line with the 5-cm perpendicular line should coincide with the needle insertion site.
At this site, a 22-gauge, 10- to 12-cm needle is inserted, as illustrated in Figure 12-4. The needle should be directed through the entry site toward an imaginary point where the femoral vessels course under the inguinal ligament. The needle is inserted until a paresthesia is elicited or until bone is contacted. If bone is encountered before a paresthesia is elicited, the needle is redirected along the line joining the sacral hiatus and the greater trochanter until a paresthesia or motor response is elicited. During this needle redirection, the needle should not be inserted more than 2 cm past the depth at which bone was originally contacted, or the needle tip will be placed anterior to the site of the sciatic nerve. Once a paresthesia or motor response is elicited, 20 to 25 mL of local anesthetic is injected.
Anterior Approach
Needle Puncture
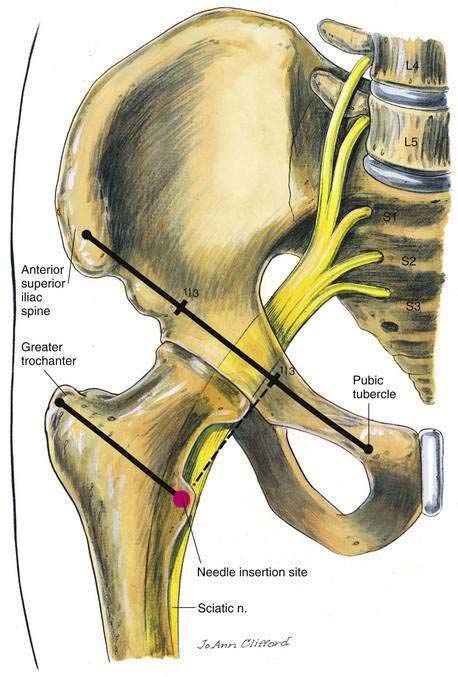
In the supine patient, a line should be drawn from the anterior superior iliac spine to the pubic tubercle. Another line should be drawn parallel to this line from the midpoint of the greater trochanter inferomedially, as illustrated in Figure 12-6. The first line is trisected, and a perpendicular line is drawn caudolaterally from the juncture of the medial and middle thirds, as shown in Figure 12-6. At the point where the perpendicular line crosses the more caudal line, a 22-gauge, 12-cm needle is inserted so that it contacts the femur at its medial border. Once the needle has contacted the femur, it is redirected slightly medially to slide off the medial surface of the femur. At approximately 5 cm past the depth required to contact the femur, a paresthesia or motor response should be sought to ensure successful block (Fig. 12-7). Once a paresthesia or motor response is obtained, 20 to 25 mL of local anesthetic is injected.
Ultrasonography-Guided Technique
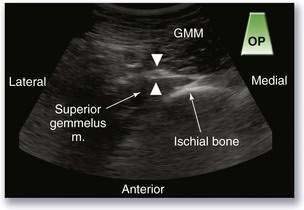
Subgluteal Approach
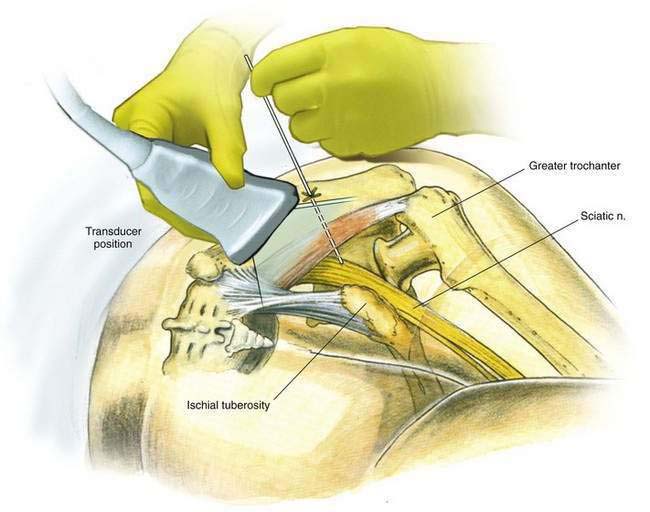
With the patient in the lateral or prone position, the operator should palpate the infragluteal crease to feel for the ropelike complex of the biceps femoris tendon. The transducer should be placed over this region (Fig. 12-8). The first objective is to identify one or both bony landmarks. At this level, the sciatic nerve is flanked by the greater trochanter laterally and the ischial tuberosity medially, both of which appear as highly reflective hyperechoic structures. The sciatic nerve should appear as a hyperechoic oval 1 to 2 cm in diameter and slightly lateral to the tendon of the biceps femoris muscle, which may also appear as an oval hyperechoic structure (Fig. 12-9). Using either the in-plane or out-of-plane technique, the needle is advanced toward the sciatic nerve. Local anesthetic is deposited by injection in a circumferential pattern around the nerve.