Chapter 89 Scheuermann Disease
Scheuermann Disease or Kyphosis
In 1920, Holger Werfel Scheuermann, a Danish surgeon, described a rigid kyphosis of the thoracic or thoracolumbar spine occurring in adolescents.1 The disease, now known as Scheuermann disease, manifests itself at puberty and involves ventral wedge formation of one or more vertebral bodies, leading to a rigid kyphotic deformity of the affected segments.2,3 It is the second most frequent etiologic factor in back pain in children and adolescents following spondylolysis and spondylolisthesis.4 Scheuermann disease typically involves the midthoracic spine, with the apex at the T7 and T8 vertebrae.5 Sorenson6 defined the radiographic diagnosis of Scheuermann kyphosis on the basis of anterior wedging of 5 degrees or more of at least three adjacent vertebral bodies. Scheuermann disease typically involves the thoracic spine but can also occur solely in the thoracolumbar spine in 25% of patients.
Incidence
Scheuermann disease affects between 1% and 8% of the general population.6,7 In a review of 1384 cadaveric specimens, Scoles et al.7 reported a prevalence of 7.4%. Scheuermann disease affects the growing, maturing spine and is usually identified in adolescents between 11 and 17 years of age. In Sorenson’s review, 58% of those affected were male and 42% were female. There are, however, widely divergent reports regarding the relative gender prevalence. Bradford8 reported a female-to-male ratio of 2:1. In contrast, Murray et al. reported a 2:1 prevalence in males9; 20% to 30% of the patients also have scoliosis. Additionally, there is an increased incidence of spondylolysis in patients with thoracic Scheuermann kyphosis.10
A familial occurrence of the disease has been described.2 Damborg et al.11 reviewed 35,000 twins and found a prevalence of Scheuermann disease of 2.8% (3.6% in males and 2.1% in females). Both the pairwise and probandwise concordance for monozygotic twins was significantly greater than that for dizygotic twins, and the hereditability was 74%. These findings may indicate a strong genetic contribution to the etiology of the condition.
Pathogenesis
The etiology of Scheuermann kyphosis remains unknown.8,12,13 Many theories have been proposed to explain the progressive wedge shaping of the involved vertebrae. Scheuermann1 considered the condition a form of avascular necrosis of the ring apophysis that leads to a growth arrest, resulting in wedging of the ventral portion of the vertebral bodies. However, Bick and Copel14 later showed that the ring apophysis does not contribute to vertebral growth. Furthermore, avascular necrosis has never been identified in affected vertebral segments of patients with the disease.8,12,15 Schmorl16 postulated that herniations of disc material through the vertebral end plates (which now bear his name) lead to a loss of disc height and ventral wedging of the vertebral body. Subsequent studies disproved these early theories but have not yet established a cause.
Osteoporosis may be an etiologic factor in the development of Scheuermann kyphosis. Bradford et al.17 prospectively studied 12 patients with an extensive osteoporosis workup and iliac crest biopsy. They identified increased levels of serum alkaline phosphatase and urinary hydroxyproline, in conjunction with reduced bone mineral density. However, when compared with age-matched controls, no specific relationship could be identified. The authors postulated that Scheuermann disease may be related to a generalized skeletal disease that presents during the adolescent growth spurt. Gilanz et al.18 subsequently reported on 20 adolescent patients 12 to 18 years of age with Scheuermann kyphosis and could demonstrate no evidence of osteoporosis (as assessed by quantitative CT).
Mechanical factors have also been postulated in the development of Scheuermann kyphosis.13,17 Strenuous physical activity has been associated with compression of the vertebrae of patients with this disease.13 Ogden et al.19 believe that the term Scheuermann disease is a misnomer; these authors state that the changes noted radiographically are altered remodeling responses to abnormal biomechanical stresses and are not secondary to an underlying disease process. They theorized that the kyphosis occurs first and that the ventral vertebral body is then subjected to increased forces that suppress ventral growth and perpetuate the deformity. The reported success of brace treatment lends support to the mechanical theory.20 Lambrinudi21 and others have suggested that the upright posture and tightness of the anterior longitudinal ligament of the spine contribute to the deformity. Most investigators believe that the growth plate becomes disorganized first and the emerging kyphosis follows. The kyphosis and growth plate changes may ultimately potentiate each other. The kyphosis likely results in increased pressure on the vertebral end plates ventrally, allowing for uneven growth of the vertebral bodies with wedging (as per Wolff law).
Recently, Fotiadis et al.22 screened 10,057 students and found 175 children with Scheuermann disease (study group). The length of the sternum was greater in the healthy (control) group. There was a statistically significant difference between the two groups with regard to sternum length. The children with Scheuermann disease were taller in relation to the control group. These authors concluded that the shorter length of sternum than normal has a possible correlation with the appearance of Scheuermann disease. Presumably the shorter length of the sternum increases the compressive forces on the vertebral end plates anteriorly, allowing uneven growth of the vertebral bodies with wedging.
Clinical Features
Patients generally present with an angular thoracic or thoracolumbar kyphosis accompanied by a compensatory hyperlordosis of the lumbar spine. Their compensatory lordosis may lead to an increase in pelvic tilt.3 Frequently, the cervical lordosis is increased with forward projection of the head. The kyphosis is fixed and remains apparent on hyperextension of the spine. In rare instances, advanced thoracic kyphosis can lead to thoracic spinal cord compression and paraparesis.23 Thoracic disc herniation may also be associated with Scheuermann kyphosis, and the patient may present with signs and symptoms of myelopathy.2,24,25 Pain, when present, is usually at the site of the thoracic deformity. Sorenson described pain as the major symptom in 50% of patients with advanced disease.6
Clinical examination often reveals tight hamstrings as well as a popliteal angle of less than 30 degrees and subtle neurologic findings. Tight hamstrings have recently been implicated as a possible cause of sagittal decompensation.26
In addition to the kyphosis of the thoracic spine, affected individuals demonstrate varying degrees of structural scoliosis.5,15,17 Blumenthal et al.13 noted lumbar scoliosis in 85% of 50 patients with type I Scheuermann disease. Spondylolysis and spondylolisthesis are also common in the lumbar spine.2,17 Ogilvie and Sherman27 observed a 50% incidence of asymptomatic spondylolysis in 18 patients with type I disease. They postulated that the excessive hyperlordosis places stress on the pars of the L4 and L5 vertebrae, resulting in the spondylolysis. Increased cervical lordosis also develops as a compensatory mechanism and causes the head to protrude forward (gooseneck deformity), producing a negative sagittal balance with the C7 plumb line lying posterior to the sacral promontory.4
Radiographic Features
Both the vertebral wedging and kyphosis should be measured by the Cobb method. When evaluating serial radiographs to document progression, care should be taken to ensure that the same end-vertebral bodies are measured each time. The normal range of thoracic kyphosis is 20 to 45 degrees on a standing lateral radiograph28–30 as measured by the Cobb method. Normal kyphosis increases with age and is slightly greater in women than in men.31,32 Ventral wedge compression of one or more vertebral segments in association with kyphosis is the hallmark radiographic feature in Scheuermann disease.1 Wedging of at least 5 degrees of three or more vertebrae is diagnostic of Scheuermann disease. The kyphosis in Scheuermann disease is usually incompletely reducible with postural and positional changes. The vertebra with the greatest ventral deformity is located at the apex of the kyphotic curve. The kyphosis may approach 100 degrees in advanced cases with a compensatory hyperlordosis of both the cervical and lumbar spine.3
Early in the progression of the disease, the end plates may appear irregular.3,5,16,33 The changes have been described as moth-eaten and relate to growth retardation rather than to a destructive process.5 As the disease progresses, the growth plates appear sclerotic, but despite interspace narrowing the change is not associated with interbody fusion. The absence of fusion helps distinguish Scheuermann disease from other kyphotic deformities of the spine.5,8,13
An MRI before surgery is recommended to rule out any incidental thoracic disc herniation, epidural cyst, or possible spinal stenosis. The literature has shown such exceptional cases in various reports of neurologic complications in Scheuermann kyphosis.2,24,25,29 The MRI also assesses the lumbar spine discs, because disc degeneration of the lumbar spine may explain, in some cases, the pain rather than the kyphotic deformity itself.
It is important to differentiate Scheuermann kyphosis from a postural roundback deformity. Adolescents with postural roundback deformity have a slight to moderate increase in the degree of thoracic kyphosis (usually ≤60 degrees), which is less acutely angulated and may be associated with an accentuated lumbar lordosis. This type of kyphosis is flexible and not associated with muscle contractures. There is also a normal appearance of the vertebrae without evidence of wedging, end-plate irregularity, or premature disc degeneration on imaging.4,33,34
Natural History
The natural history of Scheuermann disease remains very controversial. The condition tends to be symptomatic during the teenage years. However, in the late teenage years, it often produces less pain. If the residual kyphosis in these patients remains less than 50 to 60 degrees, there is usually little discomfort in adult life.35 In a long-term follow-up study, Sorenson noted pain in the thoracic region in 50% of patients during adolescence, with the number of symptomatic patients decreasing to 25% by the time of skeletal maturity.6 Later, other authors offered a contrasting view, stating that adults with Scheuermann kyphosis have a higher incidence of disabling back pain than the normal population.2,8 Murray et al.9 performed a study in 67 patients with Scheuermann kyphosis diagnosed by Sorenson’s criteria (i.e., physical examination, trunk strength, radiography, a detailed questionnaire, and pulmonary function testing). The patients had an average kyphotic deformity of 71 degrees, and average follow-up was 32 years. An age-matched comparison group was used as a control. Normal or above-normal averages for pulmonary function were found in patients in whom the kyphosis was less than 100 degrees. Patients in whom the kyphosis was greater than 100 degrees and the apex of the curve was in the first to eighth thoracic segments had restrictive lung disease. The authors concluded that patients may have functional limitations but that these did not result in severe limitations due to pain or cause major interference with their lives. Lowe and Kasten state that adults with greater than 75 degrees of kyphosis can have severe thoracic pain secondary to spondylosis that can limit their activity.36
Treatment
Nonsurgical Treatment
Exercise
Exercise has never been shown to improve or halt progression of fixed Scheuermann kyphosis.26 However, a thoracic extension program coupled with an aerobic exercise program does improve conditioning and may alleviate pain. In adults, the exercise program concentrates on stretching the hamstring and pectoral muscles and strengthening the abdominal muscles, which will probably alleviate the back pain but not alter the deformity. Weiss et al.37 reported pain reduction between 16% and 32% in a group of 351 patients with a painful Scheuermann kyphosis who were treated conservatively with physical therapy, osteopathy, manual therapy, exercises, and psychological therapy.
Bracing
Bracing and casting are of value only in patients with mobile kyphotic deformity and with a sufficient amount of growth remaining.26 The few available brace treatment studies are retrospective, have different inclusion criteria, and do not have control groups. The initial report of Bradford et al.38 regarding Milwaukee brace treatment of Scheuermann kyphosis in 75 patients demonstrated a 40% decrease in mean thoracic kyphosis and a 35% decrease in mean lumbar lordosis after an average of 34 months of brace wear. Gutowski and Renshaw39 reported on the use of Boston lumbar and modified Milwaukee orthoses for Scheuermann kyphosis and abnormal juvenile round back, with an average 26-month follow-up. Of the 75 patients in their group, 31% rejected the brace within 4 months. Compliant patients had an improvement of 27% in the Boston group and 35% in the Milwaukee group. Whether the corrections were maintained over time is not known. Bracing can be expected to provide up to a 50% correction of the deformity, with some gradual loss of correction over time. Sachs et al.40 followed 120 patients for more than 5 years after discontinuation of the brace and demonstrated that 69% still had improvement of 30 degrees or more.
The Milwaukee brace is the most commonly used brace. It is indicated when the apex of the kyphosis is at or above T8 and for the overweight patient or the female patient with large breasts. The underarm orthosis or thoracolumbosacral orthosis is indicated when the apex of the kyphosis is at or below T9.34
The classic prerequisites for brace treatment of Scheuermann kyphosis include a progressive curve beyond 45 degrees. Patients with a kyphosis of up to 65 degrees may be successfully treated. Treatment using a Milwaukee brace was shown to be effective to relieve pain and correct curves less than 74 degrees in skeletally immature patients, but curves greater than 74 degrees have been associated with higher failure rates.40 Patients must have some flexibility and some remaining growth. Bracing and/or casting is ineffective once the patient’s Risser sign is 4 or 5.26 The brace is typically worn for 23 hours a day for 1 to 2 years.
Surgical Treatment
Surgical indications have evolved over the past 2 decades. The operative indications for Scheuermann kyphosis are similar to those of patients with other deformity types: (1) progression of deformity, (2) neurologic compromise, (3) worsening pain, and (4) cosmesis.6,40,41 Some authors also list unacceptable trunk appearance as an indication.36 An adolescent with kyphosis greater than 75 degrees despite a trial of bracing may be a surgical candidate. An adult may become a candidate when severe refractory pain develops secondary to a curve of at least 60 degrees. A formal indication for surgery would be a neurologic complication appearing in the context of Scheuermann disease. The cord compression is more commonly due to thoracic disc lesions. Such complications would require neurologic decompression through an anterior thoracotomy or a posterolateral decompression.2,24,25
Biomechanical principles of the correction of the kyphosis include lengthening of the concavity (anterior column) and shortening of the convexity (posterior column). The goal of surgical intervention is a solid arthrodesis throughout the length of the kyphosis; ventral-only, ventral-dorsal, and dorsal-only approaches can accomplish this. Kostuik42 described a ventral-only approach with interbody fusion and ventral instrumentation with a Harrington distraction system augmented by postoperative bracing. He reported the results in 36 patients, with a mean preoperative reduction from 75.5 to 60 degrees. Subsequently, ventral fusion has not gained significant acceptance for the correction of Scheuermann kyphosis.
Bradford et al. originally reported the correction of deformity by a dorsal instrumentation approach.43 They noted excellent initial correction of deformity but loss of correction and pseudarthrosis in kyphotic curves exceeding 70 degrees and recommended a combined ventral-dorsal spine arthrodesis. Otsuka et al.,44 using heavier Harrington compression rods in 10 patients, reported correction from a mean of 71 to 39 degrees at 26-month follow-up. These authors performed dorsal-only surgery if the kyphosis decreased to 50 degrees or less on a hyperextension lateral radiograph. Researchers have attributed the loss of correction after dorsal-only surgery to the fusion being performed on the tension side of the spine, the failure of implants, the lack of ventral support, and inadequate correction of a severe deformity with a short construct.35
The correction of deformity by a dorsal instrumentation approach is possible by performing segmental posterior closing-wedge osteotomy across the apex of the kyphosis. Sturm et al.41 performed surgical instrumentation and fusion on 39 patients with Scheuermann disease. They found that single dorsal internal fixation and fusion was effective in correcting kyphosis (mean correction from 71.5 to 37.7 degrees) and arresting the progression in 30 of 39 patients at 72-month follow-up. The authors argued that a long dorsal fusion is the surgical treatment of choice, obviating the need for ventral approaches.
The role of an additional anterior release is more important in large and rigid curves (75 degrees or greater that do not correct to less than 50 degrees on hyperextension lateral radiographs), which are spanning few levels and are creating an acutely angular deformity, especially in the presence of a bony ankylosis across the anterior aspect of the vertebral bodies and the anterior longitudinal ligament at the apex of the kyphosis.4 Recently, the combined procedure has been performed at one operative setting; however, some authors still advocate staged procedures. The ventral portion can be performed open or endoscopically.45–48 The approach is typically performed on the right side to avoid the great vessels. A ventral release and bone graft is performed at all the levels that are wedged or have narrowed disc space. Lim et al.49 reviewed 23 patients who underwent operative treatment using multisegmental instrumentation for Scheuermann kyphosis. The mean follow-up was 38 months. Preoperative kyphosis averaged 83 degrees. Twenty of the 23 patients (87%) underwent combined anterior release/arthrodesis with posterior arthrodesis/multisegmental instrumentation. The remaining three patients underwent posterior arthrodesis/multisegmental instrumentation. Postoperative total kyphosis averaged 46 degrees and 51 degrees at final follow-up. Lee et al.50 compared posterior-only treatment (18 patients) results with segmental thoracic pedicle screw constructs versus combined anterior/posterior fusion (21 patients) in patients with Scheuermann kyphosis. The study showed a better degree of kyphosis correction in the posterior-only group and a similar small loss of deformity correction at follow-up between the two groups. They did have a patient who had a permanent paraplegia in the anteroposterior group. They concluded that posterior-only treatment with thoracic pedicle screws achieved and maintained better correction and had significantly fewer complications than with circumferential fusion. Geck et al.51 reported a series of 17 patients who underwent posterior shortening via segmental osteotomies followed by pedicle screw fixation without loss of kyphosis correction of more than 4 degrees across the instrumented level and no neurologic complications. Lonner et al.52 reported a large series comparing anteroposterior correction of kyphosis to the posterior-only approach. The authors found comparable initial correction of the deformity between the two groups but a better loss of kyphosis correction at follow-up in the posterior-only group.
Transthoracic endoscopic techniques, compared with thoracotomy, provide a less invasive method of accessing the ventral spinal column, with benefits of an excellent exposure and minimal soft tissue disruption. With the simultaneous technique, staged or subsequent procedures can be eliminated and a circumferential structural release, as well as control of the mobilized spine, can be achieved. This simultaneous technique can be extended for use in correction of a variety of thoracic spinal pathologies.46
The precise determination of the vertebrae to include within the instrumented, corrected segment is important. Despite the early recognition that fusing too short results in persistent or recurrent deformity at follow-up,38 this complication persists in even the most recent series.36 Selection of fusion levels is integral in decision making, yet no well-established criteria that have been validated with long-term follow-up are available. In the standing patient with kyphosis, the greater the deformity, the greater the compression moment across the thoracic spine.53 When using operative techniques with claw constructs at the rostral (usually T2-3 and T4-5) and caudal (usually L2-3) ends of the deformity, the remaining levels must be instrumented with the hooks placed in compression toward the apex. Using compression across the apex of the kyphosis lessens the actual bending of the rod and requires less force to be dissipated at either end of the construct. The posterior instrumentation and fusion should extend from the most proximal level of the measured kyphosis to incorporate the first lordotic segment distally as is determined on a standing lateral radiograph. Therefore, the most caudal instrumented vertebra is the one below the first lordotic disc.4 A recent study by Cho et al.54 suggested that the distal end of a fusion for thoracic hyperkyphosis should include the sagittal stable vertebra (SSV). The SSV is defined as the most proximal vertebra touched by the posterior sacral vertical line (PSVL). The PSVL is a line drawn vertically from the posterior superior corner of the sacrum on the lateral upright radiograph. Levels that include the first lordotic vertebra but not the SSV frequently lead to postoperative distal junctional kyphosis. It is also important that the fusion should be balanced on either side of the apex of the curve and that the gravity line dropped down from C7 should pass by the middle of the last fused vertebra.26
The problem of junctional kyphosis at the rostral or caudal end of the fusion mass has received significant attention in the recent literature.55,56 Factors that may predispose the patient to junctional kyphosis include the following:
• Osteoporosis may be an associated factor for junctional kyphosis at the middle or upper thoracic spine in adults.55
• Instrumentation may be too short because of failure to determine the end vertebra accurately.36 Many authors have reported that the instrumentation and fusion must extend over the entire length of the kyphosis to avoid loss of correction57 and junctional kyphosis.58 Instrumentation should not terminate at the middle or low thoracic level.55
• Excessive intraoperative dissection of the soft tissues and ligaments of the most rostral and caudal vertebral levels may weaken the construct. Wiring of the spinous processes may diminish the incidence of this complication.59
• Some authors have reported that excessive correction of kyphosis may lead to junctional kyphosis.36
• Operative techniques using pure cantilever correction of a thoracic kyphosis frequently lead to junctional kyphosis.32,60
Junctional kyphosis has been reported with Coutrel-Dubousset instrumentation. It is likely related to sagittal balance and selection of fusion levels.36,44 Lowe and Kasten37 found that these patients tend to be in negative sagittal balance. This may be exaggerated by surgery, thus predisposing to junctional kyphosis. The most recent recommendations include fusion levels, the end vertebra of the kyphosis rostrally, and the extent of the fusion to the first lordotic disc beyond the transitional zone distally.26,36,44 To correct a typical Scheuermann kyphosis adequately, dorsal corrective instrumentation from the T3 to the L2 level is necessary. Recommendations have also been made to limit the correction to 50% or less of the original deformity, in an attempt to prevent proximal junctional kyphosis.36 Overcorrection should be avoided. The use of contemporary multisegmental rod, hook, and pedicle screw systems has increased the ability of the surgeon to obtain and maintain correction. Long-term follow-up of these newer techniques is needed to assess their efficacy. More in-depth research is needed to analyze the effect of living one’s entire life with a 65-degree kyphosis as compared with having it corrected to 35 degrees and possibly subjecting patients to future problems with junctional kyphosis.
The lumbar hyperlordosis tends to improve significantly after correction of the thoracic hyperkyphosis. Jansen et al.61 measured maximum kyphosis, maximum lordosis, sacral slope, and L5-S1 angle in the preoperative and postoperative standing lateral radiographs of the spine of 30 patients. They showed a significant correlation between kyphosis and lordosis before and after surgery. Surgical correction of thoracic hyperkyphosis gave a predictable spontaneous decrease of lumbar lordosis. Correction of lordosis occurred mainly in the upper segment of lumbar lordosis.
Most surgeons who treat patients with Scheuermann kyphosis favor surgery only in the rare patient with advanced kyphosis refractory to external bracing.40,58 The dorsal approach is advocated, unless ventral compressive pathology exists. A long dorsal stabilization and internal fixation construct with segmental fixation and the use of autologous fusion provides excellent results.43,44,48,62 Five cases are provided in the following sections to illustrate the previously mentioned points.
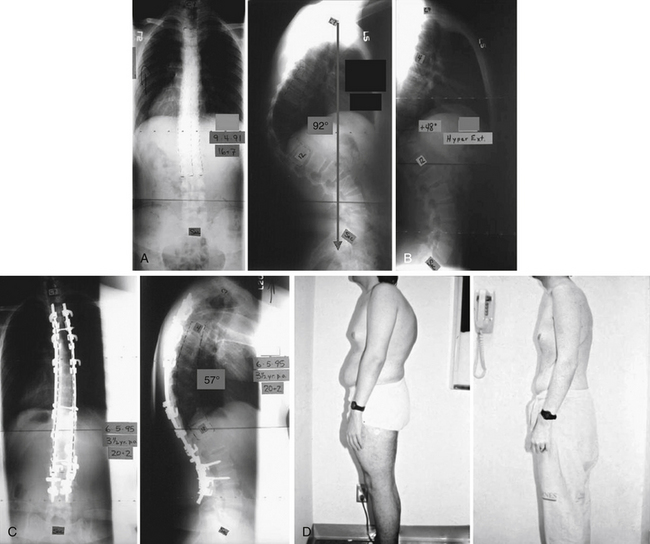
Case One
A male, 16 years and 9 months of age, with a 92-degree Scheuermann kyphosis is shown in Figure 89-1A. On a supine hyperextension lateral, he corrects to 48 degrees (Fig. 89-1B). He is treated with ventral release/discectomy/morselized bone grafting, followed by dorsal instrumentation and fusion. The construct consists of six pedicle hooks/transverse process claws above the apex. Multiple hooks and multiple pedicle screws are placed below the apex. His result at 3½ years following surgery is shown in Figure 89-1C. Clinical appearance before and after surgery is pictured in Figure 89-1D.
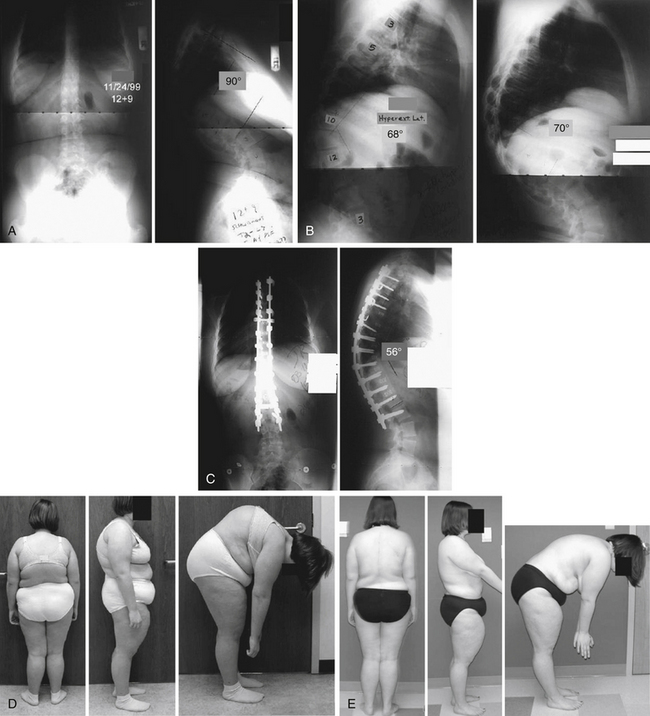
Case Two
A female, 12 years and 9 months of age, with a 90-degree Scheuermann kyphosis is presented in Figure 89-2A. On the hyperextension lateral, she corrects to roughly 70 degrees (Fig. 89-2B). She is treated with multilevel ventral release/discectomy/morselized bone grafting with some cages ventrally. Following this treatment, a dorsal fusion and instrumentation with mostly pedicle screws is performed. The 2-year postoperative result with correction to 56 degrees of kyphosis is shown in Figure 89-2C. Her preoperative clinical appearance and 2-year postoperative appearance are pictured in Figures 89-2D and E, respectively.
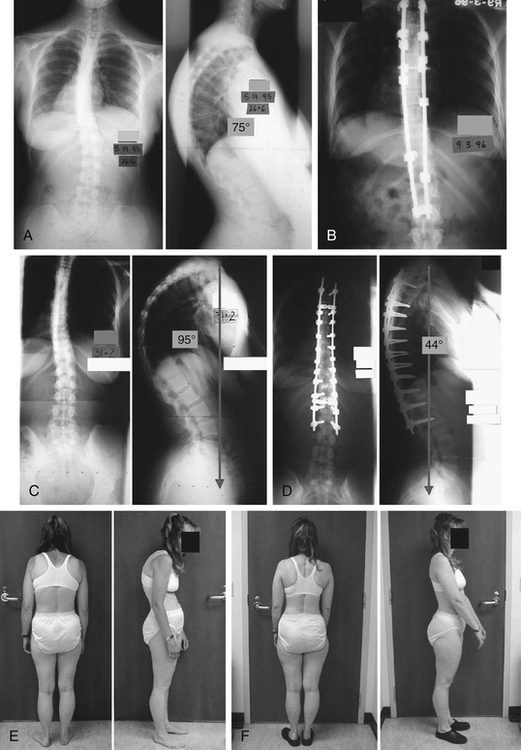
Case Three
A female, 26 years and 6 months of age, initially presented with a 75-degree Scheuermann kyphosis (Fig. 89-3A). Her initial treating surgeons attempted a dorsal-only construct (Fig. 89-3B). This construct failed, and her implants were removed. She subsequently progressed to a 95-degree kyphosis (Fig. 89-3C). With a supine hyperextension maneuver, this deformity only corrected to 85 degrees. She was then treated with a multilevel ventral release, followed by multiple Smith-Peterson osteotomies at essentially all levels and pedicle screw fixation at virtually all levels. Her kyphosis was corrected to 44 degrees (Fig. 89-3D). Her radiographic (see Fig. 89-3D) and clinical results following revision (Fig. 89-3E) and appearance at 1 year, 3 months following operation (Fig. 89-3F) are shown. She is converted from positive to negative sagittal balance.
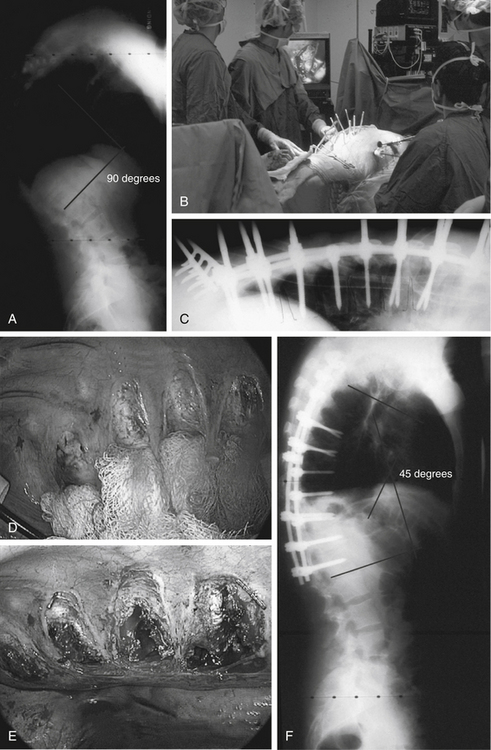
Case Four
A male, 19 years of age, presented with a 90-degree painful, progressive, and rigid Scheuermann kyphosis (Fig. 89-4A). His main concern was cosmesis. To avoid a front-back-front approach and a thoracotomy scar, a simultaneous anterior endoscopic release with interbody bone grafting and posterior segmental pedicle screw/hook instrumentation with bone grafting was recommended. In the operating room, the patient was positioned prone for the two-team approach (Fig. 89-4B). Correction was obtained by virtue of the multilevel releases with 4 to 5 degrees obtained at each level (Figs. 89-4C–E). Final correction and sagittal balance were achieved and maintained at 45 degrees (Fig. 89-4F). This case illustrates the utility and advantages of the simultaneous approach as an alternative to consider in rigid hyperkyphotic deformities.
Case Five
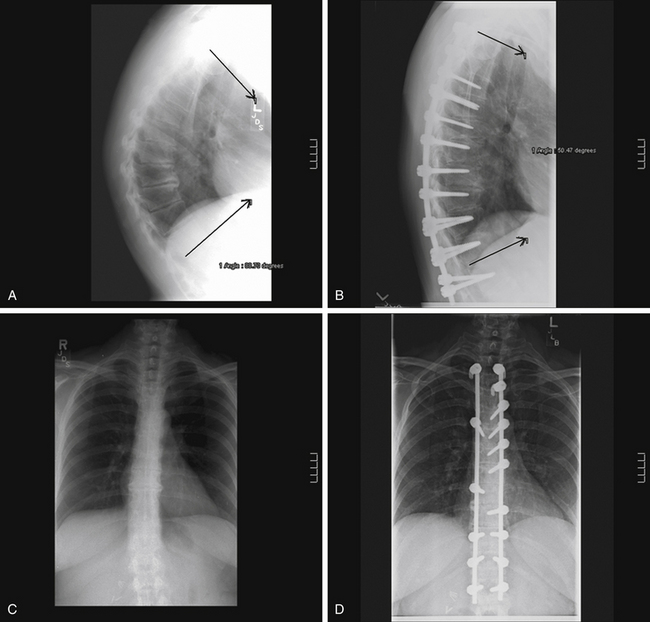
A female, 59 years of age, presented with progressive mechanical back pain and rigid Scheuermann kyphosis (Figs. 89-5A and B). A multilevel anterior release and fusion followed by posterior T3 to L1 segmental instrumentation correction and fusion were performed. Postoperatively, her curve (T3 to T12) was corrected from 90 degrees to 50 degrees.
Other Kyphotic Disorders of the Growing Spine
Two other disorders associated with kyphosis occur in the juvenile spine. Roundback deformity is a posture-related kyphosis that is reducible with extension.39 It is the most common type of thoracic kyphosis identified in patients. Its etiology is unknown but is believed to be related to poor posture during spine maturation.15 Balderston reported that it is more common in adolescent females and likely represents a compensatory slouch to developing breasts. Postural round back is differentiated from Scheuermann disease by kyphosis that corrects with hyperextension, absence of ventral vertebral deformities, lack of interbody fusion, and absence of compensatory pelvic tilt and hamstring shortening.8,38 The treatment of postural round back is observation. Occasional exercise and bracing are useful as an adjunct in patients with persistent pain.15
Congenital kyphosis of the spine is rare and results from the congenital absence or malformation of one or more vertebral segments.15 It is characterized by two distinct forms: (1) congenital absence of one or more vertebrae or (2) failure of segmentation of two or more vertebrae.3 Failure of formation may lead to neurologic compromise. However, failure of segmentation does not, and it is the failure of segmentation that often looks very much like Scheuermann kyphosis clinically and radiographically. Winter described 130 patients with congenital kyphosis of the spine.53 The female-to-male ratio was 2:1. Eighty-six patients had failure of formation of one or more segments. The treatment of patients with congenital kyphosis revolves around preventing neurologic deterioration and arresting the progressive kyphosis. Bracing is ineffective in young patients. Dorsal instrumentation and fusion is recommended in patients younger than 5 years of age with kyphosis of less than 55 degrees.15,56 Older patients with advanced kyphosis and neurologic involvement are typically managed with a ventral decompression and release, followed by a dorsal instrumentation and fusion.
Arlet V., Schlenzka D. Scheuermann’s kyphosis: surgical management. Eur Spine J. 2005;14(9):817-827.
Betz R.R. Kyphosis of the thoracic and thoracolumbar spine in the pediatric patient: normal sagittal parameters and scope of the problem. Instr Course Lect. 2004;53:479-484.
Cho K.J., Lenke L.G., Bridwell K.H., et al. Selection of the optimal distal fusion level in posterior instrumentation and fusion for thoracic hyperkyphosis: the sagittal stable vertebra concept. Spine (Phila Pa 1976). 2009;34(8):765-770.
Damborg F., Engell V., Andersen M., et al. Prevalence, concordance, and heritability of Scheuermann kyphosis based on a study of twins. J Bone Joint Surg [Am]. 2006;88(10):2133-2136.
Fotiadis E., Grigoriadou A., Kapetanos G., et al. The role of sternum in the etiopathogenesis of Scheuermann disease of the thoracic spine. Spine (Phila Pa 1976). 2008;33(1):E21-E24.
Geck M.J., Macagno A., Ponte A., et al. The Ponte procedure: posterior only treatment of Scheuermann’s kyphosis using segmental posterior shortening and pedicle screw instrumentation. J Spinal Disord Tech. 2007;20(8):586-593.
Jansen R.C., van Rhijn L.W., van Ooij A. Predictable correction of the unfused lumbar lordosis after thoracic correction and fusion in Scheuermann kyphosis. Spine (Phila Pa 1976). 2006;31(11):1227-1231.
Lee S.S., Lenke L.G., Kuklo T.R., et al. Comparison of Scheuermann kyphosis correction by posterior-only thoracic pedicle screw fixation versus combined anterior/posterior fusion. Spine (Phila Pa 1976). 2006;31(20):2316-2321.
Lim M., Green D.W., Billinghurst J.E., et al. Scheuermann kyphosis: safe and effective surgical treatment using multisegmental instrumentation. Spine (Phila Pa 1976). 2004;29(16):1789-1794.
Lonner B.S., Newton P., Betz R., et al. Operative management of Scheuermann’s kyphosis in 78 patients: radiographic outcomes, complications, and technique. Spine (Phila Pa 1976). 2007;32(24):2644-2652.
Papagelopoulos P.J., Klassen R.A., Peterson H.A., et al. Surgical treatment of Scheuermann’s disease with segmental compression and instrumentation. Clin Orthop Relat Res. 2001;386:139-149.
Papagelopoulos P.J., Mavrogenis A.F., Savvidou O.D., et al. Current concepts in Scheuermann’s kyphosis. Orthopedics. 2008;31(1):52-58. quiz 59–60
Pizzutillo P.D. Nonsurgical treatment of kyphosis. Instr Course Lect. 2004;53:485-491.
Tsirikos A.I. Scheuermann’s kyphosis: an update. J Surg Orthop Adv. 2009;18(3):122-128.
Weiss H.R., Dieckmann J., Gerner H.J. Effect of intensive rehabilitation on pain in patients with Scheuermnan’s disease. Stud Health Technol Inform. 2002;88:254-257.
1. Scheuermann H. Kyphosis dorsalis juvenilis. Ugeskr Laeger. 1920;82:385-393.
2. Bradford D.S., Moe J.H., Winter R.B. Scheuermann’s juvenile kyphosis and postural round back deformity. Rothman R.H., Simeone F.A., editors. The spine. 1975;vol 1:361-379. Philadelphia, WB Saunders
3. Tachdjian M.O., editor. Scheuermann’s juvenile kyphosis, ed 2. Pediatric Orthopedics. 1990;vol 3:2380-2390. Philadelphia, WB Saunders
4. Tsirikos A.I. Scheuermann’s kyphosis: an update. J Surg Orthop Adv. 2009;18(3):122-128.
5. Rothman R.H., Simeone F.A., Rothman R.H., Simeone F.A., editors. Scheuermann’s juvenile kyphosis, ed 3. The spine. 1992;vol 1:2380-2388. Philadelphia, WB Saunders
6. Sorenson K.H. Scheuermann’s juvenile kyphosis: clinical appearances, radiography, aetiology, and prognosis. Copenhagen: Munksgaard; 1964.
7. Scoles P.V., Latimer B.M., Digiovanni B.F., et al. Vertebral alterations in Scheuermann’s kyphosis. Spine (Phila Pa 1976). 1991;16:509-515.
8. Bradford D.S. Juvenile kyphosis. In In Moe’s textbook of scoliosis and other spinal deformities, ed 2, Philadelphia: WB Saunders; 1987:347-368.
9. Murray P.M., Weinstein S.L., Spratt K.F. The natural history and long-term follow-up of Scheuermann’s kyphosis. J Bone Joint Surg [Am]. 1993;75:236-248.
10. Betz R.R. Kyphosis of the thoracic and thoracolumbar spine in the pediatric patient: normal sagittal parameters and scope of the problem. Instr Course Lect. 2004;53:479-484.
11. Damborg F., Engell V., Andersen M., et al. Prevalence, concordance, and heritability of Scheuermann kyphosis based on a study of twins. J Bone Joint Surg [Am]. 2006;88(10):2133-2136.
12. Aufdermaur M. Juvenile kyphosis (Scheuermann’s disease): radiography, histology, and pathogenesis. Clin Orthop Relat Res. 1984;154:166-174.
13. Blumenthal S.L., Roach J., Herring J.A. Lumbar Scheuermann’s: a clinical series and classification. Spine (Phila Pa 1976). 1987;12:929-932.
14. Bick E.M., Copel J.W. The ring apophysis of the human vertebra. Contribution to human osteogeny. J Bone Joint Surg [Am]. 1951;33:783-787.
15. Moe J.H., Winter R.B., et al. Juvenile kyphosis. In: Moe J.H., Bradford D.S., Winter R.B., et al, editors. Scoliosis and other spinal deformities. Philadelphia: WB Saunders; 1978:331-343.
16. Schmorl G. Die Pathogenese der Juvenilen Kyphose. Fortschr Rontgenstr. 1930;41:359.
17. Bradford D.S., Brown D.M., Moe J.H., et al. Scheuermann’s kyphosis: a form of osteoporosis? Clin Orthop Relat Res. 1976;118:10-17.
18. Gilanz V., Gibbens D.T., Carlson M., et al. Vertebral bone density in Scheuermann’s disease. J Bone Joint Surg [Am]. 1989;71(6):894-897.
19. Ogden J.A., Ganey T.M., Sasse J. Development and maturation of the axial skeleton. Weinstein S.L., editor. The pediatric spine: principles and practice, vol 1. New York: Raven Press, 1994.
20. Vendantam R., Lenke L.G., Keeney J.A., et al. Comparison of standing sagittal spinal alignment in asymptomatic adolescent adults. Spine (Phila Pa 1976). 1998;23:211-215.
21. Lambrinudi C. Adolescent and senile kyphosis. Br Med J. 1934;2:800-804.
22. Fotiadis E., Grigoriadou A., Kapetanos G., et al. The role of sternum in the etiopathogenesis of Scheuermann disease of the thoracic spine. Spine (Phila Pa 1976). 2008;33(1):E21-E24.
23. Bradford D.S., Garcia A. Neurological complications in Scheuermann’s disease: a case report and review of the literature. J Bone Joint Surg [Am]. 1989;51:567-572.
24. Bhojraj S.Y., Dandawate A.V. Progressive cord compression secondary to thoracic disc lesions in Scheuermann’s kyphosis managed by posterolateral decompression, interbody fusion and pedicular fixation. A new approach to management of a rare clinical entity. Eur Spine J. 1994;3:66-69.
25. Chiu K.Y., Luk K.D. Cord compression caused by multiple disc herniations and intraspinal cyst in Scheuermann’s disease. Spine (Phila Pa 1976). 1995;20:1075-1079.
26. Arlet V., Schlenzka D. Scheuermann’s kyphosis: surgical management. Eur Spine J. 2005;14(9):817-827.
27. Ogilvie J.W., Sherman J. Spondylolysis in Scheuermann’s disease. Spine (Phila Pa 1976). 1983;12:251-253.
28. Bernhardt M., Bridwell K.H. Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and the thoracolumbar junction. Spine (Phila Pa 1976). 1989;14:717-721.
29. Tribus C.B. Scheuermann’s kyphosis in adolescents and adults: diagnosis and management. J Am Acad Orthop Surg. 1998;6:36-43.
30. Wenger D.R., Carollo J.J., Wilkerson J.A.Jr. Biomechanics of scoliosis correction by segmental spinal instrumentation. Spine (Phila Pa 1976). 1982;7:260-264.
31. Fon G.T., Pitt M.J., Thies A.C. Thoracic kyphosis: range in normal subjects. AJR Am J Roentgenol. 1980;134:979-983.
32. Gelb D.E., Lenke L.G., Bridwell K.H., et al. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older volunteers. Spine (Phila Pa 1976). 1995;20:1351-1358.
33. Papagelopoulos P.J., Mavrogenis A.F., Savvidou O.D., et al. Current concepts in Scheuermann’s kyphosis. Orthopedics. 2008;31(1):52-58. quiz 59–60
34. Pizzutillo P.D. Nonsurgical treatment of kyphosis. Instr Course Lect. 2004;53:485-491.
35. Lowe T.G. Scheuermann’s disease. J Bone Joint Surg [Am]. 1990;72:940-945.
36. Lowe T.G., Kasten M.D. An analysis of sagittal curves and balance after Coutrel-Dubousset instrumentation for kyphosis secondary to Scheuermann’s disease. Spine (Phila Pa 1976). 1994;19:1680-1685.
37. Weiss H.R., Dieckmann J., Gerner H.J. Effect of intensive rehabilitation on pain in patients with Scheuermnan’s disease. Stud Health Technol Inform. 2002;88:254-257.
38. Bradford D.S., Moe J.H., Montalvo F.J. Scheuermann’s kyphosis and roundback deformity: results of Milwaukee brace treatment. J Bone Joint Surg [Am]. 1969;51:567-572.
39. Gutowski W.T., Renshaw T.S. Orthotic results in adolescent kyphosis. Spine (Phila Pa 1976). 1988;13:485-489.
40. Sachs B., Bradford D.S., Winter R. Scheuermann’s kyphosis: follow-up of Milwaukee brace treatment. J Bone Joint Surg [Am]. 1987;69:50-54.
41. Sturm P.F., Dobson J.C., Armstrong G.W.D. The surgical management of Scheuermann’s. J Bone Joint Surg [Am]. 1993;18:685-691.
42. Kostuik J.P. Anterior Kostuik-Harrington distraction systems. Orthopedics. 1988;11:1379-1391.
43. Bradford D.S., Moe J.H., Montalvo F.J., et al. Scheuermann’s kyphosis: results of surgical treatment by posterior spine arthrodesis in 22 patients. J Bone Joint Surg [Am]. 1975;57:439-448.
44. Otsuka N.Y., Hall J.E., Mah J.Y. Posterior fusion for Scheuermann’s kyphosis. Clin Orthop Relat Res. 1990;51:134-139.
45. Heniford B.T., Matthews B.D., Lieberman I.H. Laparoscopic lumbar interbody spinal fusion. Surg Clin North Am. 2000;80(5):1487-1500.
46. Lieberman I.H., Salo P.T., Orr R.D., Kraetschmer B. Prone position endoscopic transthoracic release with simultaneous posterior instrumentation for spinal deformity: a description of the technique. Spine (Phila Pa 1976). 2000;25:2251-2257.
47. McLain R.F., Lieberman I.H. Endoscopic approaches to metastatic thoracic disease. Spine (Phila Pa 1976). 2000;25:1855-1858.
48. Regan J.J., Yuan H., McCullen G. Minimally invasive approaches to the spine. Springfield D.S., editor. Instructional course lectures. 1997;vol 46:127-141. Rosemont IL, American Academy of Orthopedic Surgeons
49. Lim M., Green D.W., Billinghurst J.E., et al. Scheuermann kyphosis: safe and effective surgical treatment using multisegmental instrumentation. Spine (Phila Pa 1976). 2004;29(16):1789-1794.
50. Lee S.S., Lenke L.G., Kuklo T.R., et al. Comparison of Scheuermann kyphosis correction by posterior-only thoracic pedicle screw fixation versus combined anterior/posterior fusion. Spine (Phila Pa 1976). 2006;31(20):2316-2321.
51. Geck M.J., Macagno A., Ponte A., et al. The Ponte procedure: posterior only treatment of Scheuermann’s kyphosis using segmental posterior shortening and pedicle screw instrumentation. J Spinal Disord Tech. 2007;20(8):586-593.
52. Lonner B.S., Newton P., Betz R., et al. Operative management of Scheuermann’s kyphosis in 78 patients: radiographic outcomes, complications, and technique. Spine (Phila Pa 1976). 2007;32(24):2644-2652.
53. Winter R.B., Moe J.H., Wang J.F. Congenital kyphosis: its natural history and treatment as observed in a study of one hundred thirty patients. J Bone Joint Surg [Am]. 1973;55:189-193.
54. Cho K.J., Lenke L.G., Bridwell K.H., et al. Selection of the optimal distal fusion level in posterior instrumentation and fusion for thoracic hyperkyphosis: the sagittal stable vertebra concept. Spine (Phila Pa 1976). 2009;34(8):765-770.
55. Lettice J., Ogilvie J., Transfeldt E. Proximal junctional kyphos following Coutrel-Dubousset instrumentation in adult scoliosis. Orthop Trans. 1992;16:162.
56. Reinhardt P., Bassett G.S. Short segmental kyphosis following fusion for Scheuermann’s disease. J Spinal Disord. 1990;3:162-168.
57. Speck G.R., Chopin D.C. The surgical treatment of Scheuermann’s kyphosis. J Bone Joint Surg [Br]. 1982;68:189-193.
58. Herndon W.A., Emans J.B., Micheli L.J. Combined anterior and posterior fusion for Scheuermann’s kyphosis. Spine (Phila Pa 1976). 1980;6:125-130.
59. La Grone M.O. Loss of lumbar lordosis: a complication of spinal fusion for scoliosis. Orthop Clin North Am. 1988;19:383-393.
60. Coscia M.F., Bradford D.S., Ogilvie J.W. Scheuermann’s kyphosis: results in 19 cases treated by spinal arthrodesis and L-rod instrumentation. Orthop Trans. 1988;12:255.
61. Jansen R.C., van Rhijn L.W., van Ooij A. Predictable correction of the unfused lumbar lordosis after thoracic correction and fusion in Scheuermann kyphosis. Spine (Phila Pa 1976). 2006;31(11):1227-1231.
62. Papagelopoulos P.J., Klassen R.A., Peterson H.A., et al. Surgical treatment of Scheuermann’s disease with segmental compression and instrumentation. Clin Orthop Relat Res. 2001;386:139-149.