CHAPTER 55 Scaphoid Hemiresection and Arthrodesis of the Radiocarpal Joint
Indications and Contraindications
The underlying pathology of radiocarpal arthritis frequently is due to trauma or degenerative changes or both. The leading causes are malunited or nonunited fractures of the radius or scaphoid, radiocarpal or intercarpal dislocations or dissociations, or forms of primary osteoarthritis or inflammatory arthritis. Management has focused on reducing pain to increase function, while, when possible, preserving some degree of motion, with total wrist arthrodesis being the ultimate salvage procedure.1,2 Surgical approaches that attempt to preserve some motion have included proximal row carpectomy, four-corner fusion with and without scaphoid excision, radiolunate arthrodesis, radioscapholunate arthrodesis, and lunocapitate arthrodesis.2–7
Motion-sparing surgical procedures require healthy articular cartilage at the site of preserved motion. For proximal row carpectomy, a healthy capitate head and lunate fossa are required; for a four-corner fusion, the lunate and its fossa of the radius must have a healthy articular surface. Radiolunate and radioscapholunate arthrodesis require a healthy midcarpal joint and can provide stability, but result in a significantly limited arc of motion and a moderately high failure rate because the scaphoid acts as a strut between the proximal and distal carpal rows.2,8
Biomechanical studies have shown the effect of preserving versus osteotomizing the scaphoid on midcarpal joint motion, with osteotomy significantly increasing the degree of allowable motion through the midcarpal joint.5,8 When the lunate and the scaphoid fossae are arthritic, but the midcarpal articulation of the capitate in its lunate and scaphoid fossae remains healthy, it is logical to attempt to preserve and use the midcarpal joint to retain motion, while eliminating pain through an arthrodesis of the arthritic radiocarpal surfaces.2,9
This chapter describes a step-by-step technique of using a tensioned, flexible plating system (Small Bone Innovations, Morrisville, PA) to perform a scaphoid hemiresection and recessed arthrodesis of the radiocarpal joint (the SHARC procedure). This procedure allows the capitate to move within its midcarpal joint as a “universal” joint.8 The ideal candidate is a patient with radiocarpal arthritis and a healthy midcarpal articulation. Contraindications to performing the procedure are active local infection, systemic disease, midcarpal arthrosis, and unwillingness of the patient to comply with postoperative instructions and rehabilitation protocols.
Technique
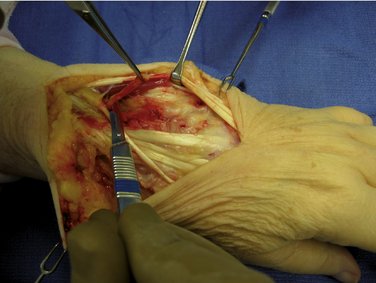
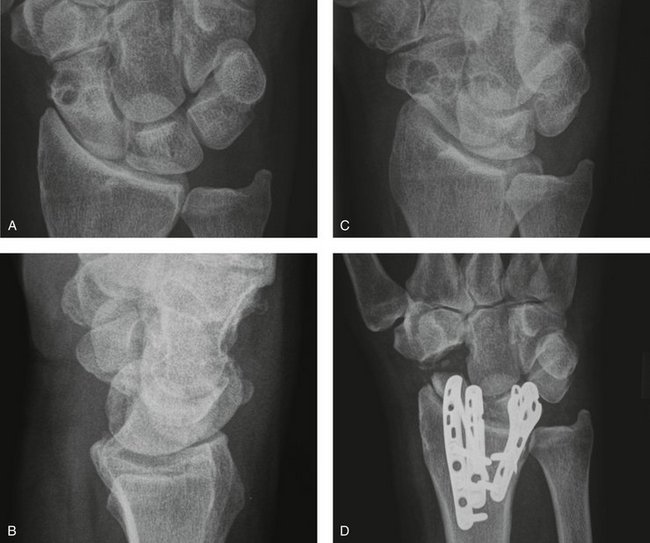
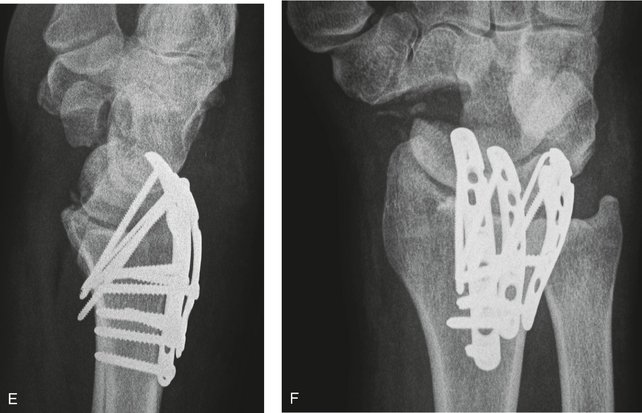
A dorsal midline incision is used in all cases. The extensor retinaculum is step-cut and reflected, and the extensor tendons from the first through the fifth compartment are mobilized and retracted (Fig. 55-1). As an adjunct for postoperative pain relief, a posterior interosseous sensory neurectomy is performed (Fig. 55-2).10 The radiocarpal joint capsule is incised longitudinally and elevated medially and laterally exposing the entire distal radius, scaphoid, lunate, and midcarpal joint. The radiocarpal articulation should be assessed at this point, confirming the preoperative diagnosis of arthritic degeneration of the radioscaphoid and radiolunate articular surfaces with preservation of a healthy articulation at the capitolunate joint (Fig. 55-3).
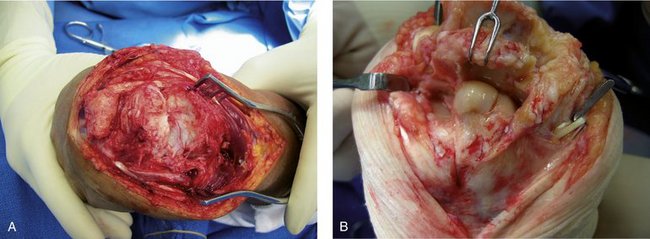
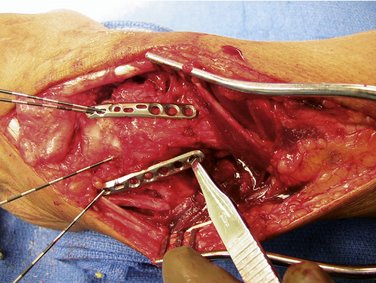
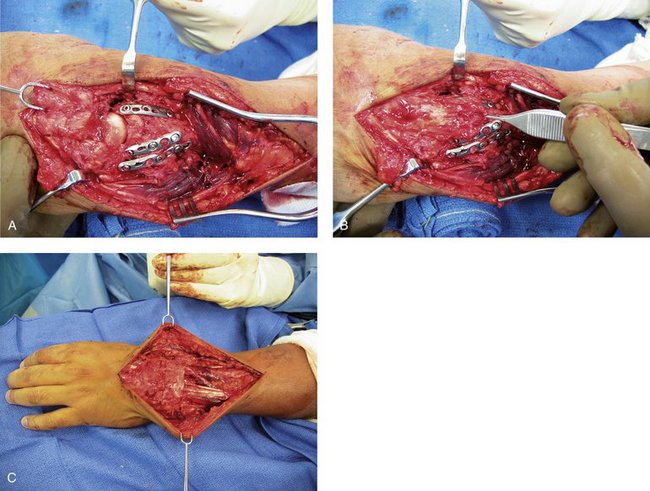
Residual degenerative articular surface of the proximal lunate and scaphoid is removed with a curet, rongeur, or high-speed bur (Fig. 55-4), and a bur is used to create a complementary recessed “cup” in the distal radial metaphysis (Fig. 55-5). The scaphoid is next osteotomized at its waist, and the distal half of the scaphoid is morcellated and sharply excised (Fig. 55-6). The proximal scaphoid and lunate, with exposed raw cancellous bone along their entire proximal surfaces, are recessed into the hollowed-out distal radius in a neutral position (Fig. 55-7). From the Wrist-Fit fixation set (Small Bone Innovations, Morrisville, PA), 0.045-inch Kirschner wires (K-wires) are inserted from dorsal distal to palmar proximal in an oblique fashion, placing at least three K-wires between the scaphoid and the lunate into the radius (Fig. 55-8).
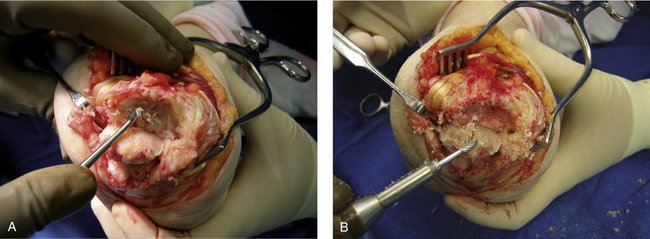
FIGURE 55-4 A and B, Cartilage remnants are removed with a curet, and the residual degenerative articular surface of the proximal lunate and scaphoid is removed with a high-speed bur, exposing a cancellous surface.
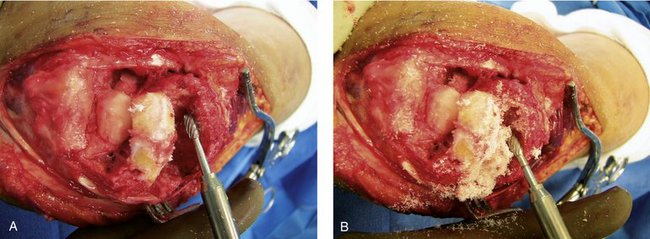
FIGURE 55-5 A and B, A bur is used to create a complementary recessed “cup” in the distal radial metaphysis.

FIGURE 55-7 The proximal scaphoid and lunate are recessed into the hollowed-out distal radius in a neutral position.

FIGURE 55-8 Kirschner wires from the Wrist-Fit fixation set (Small Bone Innovations, Morrisville, PA) are inserted from dorsal distal to palmar proximal in an oblique fashion.
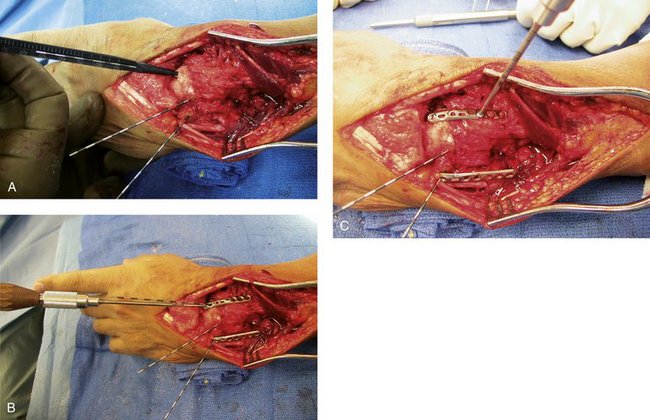
Alternatively, the pin plates from the distal radius fixation system (Tri-Med, Valencia, CA) may be used. In most cases, two K-wires are placed in the scaphoid longitudinally, and two are placed in the lunate transversely. Three flexible conforming plates are slid over the K-wires (Fig. 55-9), held in place while the screw holes are predrilled, measured, and secured down with cortical screws, “tension-locking” the pin plate constructs into place. The depth of the K-wires is measured, and the K-wires are replaced with high angle screws from the set (Fig. 55-10). X-ray confirmation ensures satisfactory alignment of the recessed scapholunate arthrodesis and maintenance of the capitate within the scapholunate midcarpal fossa, now functioning as a “universal joint” (Fig. 55-11).
When secure fixation is achieved, the capsule is reapproximated and closed anatomically; a slip of the step-cut extensor retinaculum is sometimes placed beneath the extensor tendons over the distal portion of the pin plates, while the more proximal portion of the retinaculum is reapproximated holding the extensor tendons in place (Fig. 55-12). The overlying subcutaneous tissue is approximated with interrupted inverted absorbable sutures, and the skin is closed with a running absorbable subcuticular 6-0 suture.
Results
The senior author (W.H.S.) has now successfully used this technique in more than 30 cases. In an initial review presented at the 59th American Society for Surgery of the Hand (ASSH) annual meeting (2004, New York City) and submitted for publication, 12 patients with radiocarpal arthritis were managed with the SHARC procedure. The authors used a tension plating system (Small Bone Innovations, Morrisville, PA, or Tri-Med, Valencia, CA) designed and contoured for distal radius fractures. There were 11 men and 1 woman an average age of 57.1 years (age range 28 to 79 years). Diagnoses included post-traumatic arthritis following malunited distal radius fracture (three patients), fracture-dislocation of the wrist (four patients), scapholunate dissociation with advanced collapse (four patients), and scaphoid nonunion with advanced collapse (one patient).
Discussion
Radiocarpal arthritis of various etiologies frequently involves the radioscaphoid articulation, but sometimes spares the radiolunate joint. When the proximal lunate articular surface and its fossa within the radius are well preserved, proximal row carpectomy and four-corner fusion have been shown to be effective, motion-preserving reconstructive procedures, relieving the pain of arthritis.3,5–7 Similarly, midcarpal arthritis is well treated with four-corner fusion.3–5
Because the scaphoid represents a stable strut between the proximal and distal rows, its integrity precludes significant midcarpal motion. When it remains intact after radioscapholunate arthrodesis, there is a much longer lever arm acting to create motion at the attempted arthrodesis site, which can lead to nonunion. Conversely, if union is obtained, stresses may now be transmitted to the scaphotrapezial joint, creating painful arthrosis at this location. The biomechanical effect of this stable strut between the proximal and distal rows also explains why excision can enhance motion even when four-corner fusion is performed.4,5,8
Limited, “anatomy-specific” fixation using tensioned K-wires or screws with flexible contoured plates and cortical screws has been shown to provide an extremely secure fixation around the distal radius.11 Application of this technique uses a minimal amount of hardware to provide secure fixation of the lunate and proximal half of the scaphoid into the concavity of the distal radius, while allowing early controlled motion through the new midcarpal “universal” joint.
In the authors’ experience, total wrist arthrodesis or possibly total wrist arthroplasty are the alternative procedures, and in our estimation should be reserved as salvage procedures. In the face of advanced diffuse radioscapholunate arthritis with evidence of a healthy midcarpal joint, the SHARC procedure is an effective reconstructive procedure, providing stability, relieving pain, and preserving functional mobility. Results of the SHARC procedure are comparable to the results of other successful motion-sparing procedures, providing an alternative when the entire radial articular surface is degenerative.2,3,5–7 It provides a functional alternative to wrist arthrodesis and enhanced motion compared with radioscapholunate arthrodesis alone, with more functional outcomes and fewer complications.1,2 This procedure does not preclude salvage with total wrist arthrodesis or arthroplasty.
1. De Smet L, Truyen J. Arthrodesis of the wrist for osteoarthritis: outcome with a minimum follow-up of 4 years. J Hand Surg. 2003;28B:575-577.
2. Nagy L, Büchler U. Long-term results of radioscapholunate fusion following fractures of the distal radius. J Hand Surg. 1997;22B:705-710.
3. Krakauer JD, Bishop AT, Cooney WP. Surgical treatment of scapholunate advanced collapse. J Hand Surg. 1994;19A:751-759.
4. Kobza PE, Budoff JE, Yeh ML, et al. Management of the scaphoid during four-corner fusion—a cadaveric study. J Hand Surg. 2003;28A:904-909.
5. Tomaino MM, Miller RJ, Cole I, et al. Scapholunate advanced collapse wrist: proximal row carpectomy or limited wrist arthrodesis with scaphoid excision? J Hand Surg. 1994;19A:134-142.
6. Tomaino MM, Delsignore J, Burton RI. Long-term results following proximal row carpectomy. J Hand Surg. 1994;19A:694-703.
7. Wyrick JD. Proximal row carpectomy and intercarpal arthrodesis for the management of wrist arthritis. J Am Acad Orthop Surg. 2003;11:277-281.
8. McCombe D, Ireland DCR, McNab I. Distal scaphoid excision after radioscaphoid arthrodesis. J Hand Surg. 2001;26A:877-882.
9. Garcia-Elias M, Lluch A, Ferreres A, et al. Treatment of radiocarpal degenerative osteoarthritis by radioscapholunate arthrodesis and distal scaphoidectomy. J Hand Surg. 2005;30A:8-12.
10. Berger RA. Partial denervation of the wrist: a new approach. Tech Hand Upper Extrem Surg. 1998;2:25-35.
11. Dodds SD, Cornelissen S, Jossan S, et al. A biomechanical comparison of fragment-specific fixation and augmented external fixation for intra-articular distal radius fractures. J Hand Surg. 2002;27A:953-964.